Pediatrician salaries in the United States can vary widely based on factors like location, experience, subspecialty, and employment type. Many organizations provide national estimates and salary estimates to reflect the national average, but these figures can differ based on hours per week worked and each pediatrician’s specific job requirements.
Despite recent compensation growth, pediatrics remains a lower-paid physician specialty. According to the latest data from the Bureau of Labor Statistics (BLS), general pediatricians earn a mean annual wage of about $205,860.
Other surveys of physicians report higher averages of around $244,000–$260,000 per year, reflecting total compensation, including bonuses. Below, we break down pediatrician salaries by influential factors, geographic differences, subspecialties, and trends into 2025.
Factors Influencing Pediatrician Salaries
Work schedule, specialization, and even gender trends all play a role in determining income differences within the field. Entry-level pediatricians will see different median wages compared to more seasoned colleagues, highlighting the importance of experience level in overall earning potential. Let’s take a closer look at these factors below.
Full-time vs. Part-time Positions
One major factor is whether a pediatrician works full-time or part-time. Pediatricians working part-time naturally earn less per year, though their hourly pay is often similar to full-time peers.
Many pediatricians (especially women) choose part-time schedules for work-life balance – female pediatricians are likelier to work part-time than males. This contributes to income differences, as part-timers will have lower annual salaries.
Specialization (General vs. Subspecialist):
Within pediatrics, pursuing a subspecialty fellowship can lead to higher or lower pay compared to general pediatrics. General pediatricians (primary care) have average incomes in the mid-$200,000s. Some subspecialties that involve more acute or high-stakes care pay significantly more. For instance, pediatric cardiologists and critical care specialists often earn between $290,000–$350,000 per year, well above a general pediatrician.
Pediatric emergency medicine and neonatology (newborn intensive care) also command higher salaries (often in the $250,000+ range) due to demanding hours and specialized skills. On the other hand, subspecialties like pediatric infectious disease or adolescent medicine tend to earn less – sometimes in the low $200,000s or below – in part because these fields often involve academic or public health settings with lower pay.
Overall, choosing a pediatric subspecialty can swing a physician’s salary by tens of thousands of dollars.
Gender Pay Differences
Like many medical fields, pediatrics has a notable gender pay gap. Male pediatricians, on average, earn more than female pediatricians, partly because female physicians more often work fewer hours or take on roles with lower pay.
Unadjusted surveys have found female pediatricians earn only 76% of what male pediatricians earn on average – roughly $51,000 less per year early in their careers.

Even after adjusting for factors like hours worked, years of experience, and practice type, a recent study in the journal Pediatrics (2024) found female pediatricians earned about 93% of male pediatricians’ pay – an ~$11,000 annual gap in otherwise similar roles.
Practice Environment Impact
The practice setting and employer type greatly influence salary. Pediatricians in private practice (especially those who own or co-own their practice) might have higher earning potential based on patient volume and ancillary service revenue but also face overhead costs.
Many pediatricians are employed by hospitals, health systems, or large medical groups – these salaried positions offer stability and benefits, though sometimes slightly lower base pay than private practice partners.
Industry data show pediatricians in outpatient care centers or private physician offices earn around $213,000–$225,000 on average. Those working for local government agencies (e.g., county hospitals or public clinics) earned about $236,850 on average.
Academic pediatricians (teaching in medical schools and working at university hospitals) often earn less than private-sector peers. For example, one survey found the median academic general pediatrician salary was only around $157,000.
Average Pediatrician Salaries by Geography
Geography is one of the biggest determinants of pediatrician pay. Salaries vary from state to state and between urban and rural areas, often reflecting cost of living differences and local supply/demand for pediatric services. While there is growing salary transparency in many states, actual compensation can still differ significantly across regions.
Pediatrician Salaries by State
According to the latest data from the U.S. Bureau of Labor Statistics (BLS) as of May 2023, the national mean annual wage for general pediatricians is $205,860. However, salaries vary significantly by state, with some regions offering substantially higher compensation. Here’s a great map to get an overview of pediatric salaries by state.
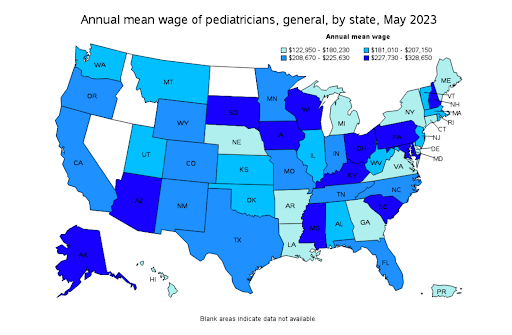
Top-Paying States for Pediatricians
The highest-paying states for general pediatricians, based on mean annual wages, are:
- Mississippi – $328,650
- Iowa – $264,400
- Wisconsin – $255,960
- South Carolina – $244,780
- Pennsylvania – $240,120
These states, many of which have lower population densities or fewer pediatricians per capita, tend to offer higher salaries to attract and retain medical professionals.
Lowest-Paying States for Pediatricians
Conversely, some states report significantly lower wages for general pediatricians. Based on the BLS salary distribution map, some of the lowest-paying states (those in the $122,950–$180,230 range) include:
- Louisiana
- Nebraska
- Hawaii
- Georgia
- Michigan
Regional Pay Trends
- Higher pay is often found in lower cost-of-living states, particularly in the South and Midwest, where pediatrician shortages drive up wages.
- Lower salaries are more common in states with a high supply of pediatricians or major urban centers where academic and hospital-based positions may offer lower compensation.
This salary distribution reflects the broader trend in medical compensation, where rural and underserved areas must offer higher pay to attract specialists, whereas states with large pediatric hospital networks tend to have lower salaries due to physician oversupply.
Urban vs. Rural Earnings
The difference in pediatrician pay between urban and rural areas is not as drastic as one might assume. While rural and small-town practices may offer incentives (sign-on bonuses, loan repayment, housing allowances) to attract pediatricians, the base salaries tend to be roughly in line with urban areas – often within 5–10% difference.
A physician recruiter quoted in NEJM Career Center noted that rural pediatrician offers might be at most 10% higher than urban ones in some cases, but generally, “salary differences are minimal.” For example, a pediatrician in a mid-sized city might be offered $220,000, whereas a very rural clinic might offer around $230,000 for a similar role.
The cost of living and payer mix can influence this: rural pediatricians might serve more Medicaid patients (leading to lower reimbursement rates) which can cap salaries despite demand.
However, rural jobs often come with other perks like lower living costs, possible state/federal loan forgiveness, or stronger community ties. In urban centers, pediatricians sometimes earn higher hourly rates if working extra shifts or in urgent care networks, but they also face higher expenses.
Overall, while there are pockets of higher pay in less populated areas, the urban-rural salary gap in pediatrics is modest compared to some other specialties. Pediatricians should consider quality of life and support resources in addition to salary when comparing urban vs. rural opportunities.
Pediatrician Salaries by Subspecialty
Not all pediatricians are generalists – many undertake additional training in pediatric subspecialties, which can dramatically affect salary. Here’s a breakdown of pediatrician salaries by subspecialty, from the highest-paying to the more modest.

Highest-Paying Pediatric Subspecialties
Subspecialties that deal with acute, complex conditions or procedural skills tend to offer the highest compensation. These include pediatric cardiology, pediatric critical care, neonatology, and emergency medicine.
Pediatric Cardiology ($300,000–$350,000 per year)
Pediatric cardiologists specialize in diagnosing and treating congenital heart defects, arrhythmias, and other cardiovascular conditions in children. Their expertise is critical, as many heart conditions in infants and young children require early intervention to ensure normal development.
In addition to managing long-term conditions, many pediatric cardiologists perform diagnostic procedures such as echocardiograms and, in some cases, interventional catheterization, which adds to their earning potential.
Pediatric Critical Care Medicine ($280,000–$340,000 per year)
Also known as pediatric intensivists, these specialists work in Pediatric Intensive Care Units (PICUs), where they manage critically ill children with life-threatening conditions, such as severe infections, respiratory failure, or post-surgical complications.
Given the 24/7 demands of intensive care and the need for rapid, high-stakes decision-making, pediatric critical care physicians earn competitive salaries. They often work in large children’s hospitals or academic medical centers, where advanced treatments such as extracorporeal membrane oxygenation (ECMO) and mechanical ventilation are common.
Neonatology ($280,000–$340,000 per year)
Neonatologists focus on the care of premature and critically ill newborns, typically working in Neonatal Intensive Care Units (NICUs). They manage conditions such as respiratory distress syndrome, neonatal sepsis, and congenital abnormalities, often making split-second decisions that can have lifelong consequences.
Due to the delicate nature of their patients and the round-the-clock nature of NICU care, neonatologists are among the higher earners in pediatrics.
Pediatric Emergency Medicine ($260,000–$330,000 per year)
Pediatric emergency physicians work in hospital emergency rooms and trauma centers, handling everything from minor injuries to life-threatening conditions such as sepsis, severe asthma attacks, and traumatic injuries. Their work is fast-paced and high-pressure, requiring broad expertise in acute care, resuscitation, and procedural interventions such as intubations and fracture reductions.
The unpredictable nature of emergency medicine, combined with irregular hours and high patient volumes, contributes to their relatively high salaries.
Pediatric Gastroenterology ($230,000–$290,000 per year)
Pediatric gastroenterologists diagnose and treat digestive disorders in children, such as celiac disease, inflammatory bowel disease (IBD), and gastroesophageal reflux disease (GERD). Many also perform endoscopic procedures like colonoscopies and upper endoscopies, which can increase earning potential. Their expertise is especially valuable in major children’s hospitals and specialized digestive health centers.
Pediatric Pulmonology ($210,000–$250,000 per year)
Pediatric pulmonologists specialize in lung and respiratory disorders, treating conditions such as asthma, cystic fibrosis, and chronic lung disease in premature infants. They may work in hospitals managing ventilator-dependent patients or in outpatient settings providing long-term asthma and allergy care. Those involved in procedural work, such as bronchoscopy or ventilator management, tend to earn on the higher end of the salary range.
It’s worth noting that even the top pediatric subspecialties often pay less than adult medicine equivalents; for instance, adult cardiologists earn around $507,000, while pediatric cardiologists average much lower. Nonetheless, within the pediatric realm, choosing a subspecialty like cardiology or ICU can mean earning $50,000–$100,000 more than a general pediatrician.
Lower-Paying Pediatric Subspecialties
On the other end, some pediatric subspecialists earn below the general pediatrics average. These include pediatric infectious disease, endocrinology, hematology, oncology, and rheumatology.
These are usually fields that are primarily cognitive (consultative) rather than procedural or have a large portion of practitioners in academic settings. These fields might rely on clinic visits and counseling rather than procedures, and sometimes are grant-funded or academic roles, hence the lower pay.
Below is a breakdown of some key pediatric subspecialties with relatively modest compensation despite their critical importance.
Pediatric Infectious Disease ($180,000–$210,000 per year)
Pediatric infectious disease (ID) specialists diagnose and treat serious infections in children, including antibiotic-resistant bacteria, viral outbreaks, and immune-compromised patients. They play a crucial role in hospital infection control, outbreak response, and antibiotic stewardship programs. However, because many work in academic hospitals, public health organizations, or research settings rather than private practice, their salaries tend to be lower compared to procedural specialties.
Pediatric Endocrinology ($220,000–$300,000 per year)
Pediatric endocrinologists specialize in hormone-related disorders, managing conditions such as type 1 diabetes, growth hormone deficiencies, and thyroid disorders. While their salaries are mid-range within pediatrics, they tend to be on the lower side for specialists with extensive experience. This is likely due to the fact that most of their work involves outpatient management rather than high-revenue procedures.
However, those involved in advanced diabetes management, insulin pump therapies, or research may earn at the higher end of this range.
Pediatric Hematology-Oncology ($200,000–$230,000 per year)
Hematologist-oncologists treat children with blood disorders such as sickle cell disease and leukemia, as well as other pediatric cancers. The work is emotionally demanding, involving long-term patient relationships and complex treatments like chemotherapy and bone marrow transplants.
Despite the high stakes, many pediatric hematologist-oncologists work in large children’s hospitals or academic institutions where salaries are lower than in private practice. The field also requires extensive training, making the pay gap compared to other specialists more noticeable.
Pediatric Rheumatology ($190,000–$220,000 per year)
Pediatric rheumatologists diagnose and treat autoimmune and inflammatory diseases such as juvenile arthritis, lupus, and vasculitis. Because these conditions require long-term management and often involve complex medication regimens rather than high-revenue procedures, salaries in this field tend to be on the lower end.
Additionally, there are fewer pediatric rheumatologists compared to other subspecialties, which can impact salary growth potential due to limited demand.
Adolescent Medicine ($200,000 or below per year)
Adolescent medicine specialists focus on health concerns unique to teenagers, including puberty-related issues, eating disorders, reproductive health, and mental health care.
Since much of their work is clinic-based and involves counseling rather than procedures, their compensation is typically lower. Many also work in academic or public health roles, which further limits earning potential.
Developmental-Behavioral Pediatrics ($200,000 or below per year)
Developmental-behavioral pediatricians specialize in diagnosing and managing conditions such as autism, ADHD, learning disabilities, and developmental delays. Their work often involves extended evaluations, family counseling, and coordination with schools and therapists. Because this specialty does not rely on high-cost procedures and is sometimes grant-funded, salaries remain modest compared to other fields in pediatrics.
General Pediatrics vs. Subspecialty
It’s interesting to note that some data have shown that after the lengthy extra training, certain pediatric subspecialists actually lose financial ground compared to if they had stayed in general pediatrics. A study of lifetime earning potential found that many pediatric subspecialists earn significantly less over a career than their counterparts in adult medicine, and in some cases even less than general pediatricians, due to a later start in practice and often lower pay scales.
For example, a general pediatrician starting at age 29 and eventually making partner in a practice might outearn a pediatric nephrologist who trains until 33 and works in academia.
Thus, pediatricians should choose subspecialties based on passion and interest, with the understanding that only some subspecialties (like cardiology, critical care, neonatology) offer a clear financial boost.
On the whole, subspecialization can raise or lower income: those in procedural, hospital-based subspecialties often earn more, whereas those in clinic-based or research-focused subspecialties may earn less than if they remained generalists.
Locum Tenens Pediatricians
Locum tenens pediatricians play a vital role in maintaining continuity of care when hospitals and clinics face staffing shortages. Their work not only helps underserved areas but also provides physicians with unique career flexibility and diverse clinical experiences. Some find the locum tenens lifestyle appealing because it allows them to choose assignments and shape their own annual pediatrician salary trajectory.
Pay Structure of Locum Tenens Pediatricians
Locum tenens pediatricians work on temporary contracts – filling in at hospitals or clinics for a few days to months. Their compensation is typically based on an hourly or daily rate rather than a fixed annual salary. Because locums take on short-term assignments (often in high-need areas), their hourly pay is relatively high.
According to a physician staffing firm, locum tenens pediatricians can earn up to $125 per hour. If a locum worked full-time hours year-round at that rate, it would equate to roughly $260,000 per year. In practice, locum pediatricians have flexibility in how much they work. Some may do locum tenens full-time, moving between assignments to maximize income, while others pick up occasional locum shifts to supplement their regular job.
Locum Tenens vs. Full-Time Salaries

On an annualized basis, a busy locum tenens pediatrician can out-earn the average employed pediatrician. Locum tenens doctors can make about 7% more than a permanent pediatrician on average. For example, if the average staff pediatrician earns ~$244,000, a locum working similar hours might gross around $260,000.
However, direct comparisons are tricky. Locum tenens physicians do not receive benefits like paid vacation, health insurance, retirement contributions, or paid malpractice (sometimes agencies cover malpractice, but not always things like health insurance). They also might have unpaid gaps between contracts.
Meanwhile, full-time employed pediatricians often have stable salaries and benefits, but if they work beyond their scheduled hours (evenings, extra call) their salary might not increase, whereas a locum gets paid for every hour worked.
In short, locum tenens work offers higher hourly pay and great flexibility – which can be lucrative, especially for mid-career pediatricians looking to boost income or semi-retirees wanting part-time work. A locum assignment in a rural area might pay a premium rate (due to urgent need), further increasing earnings. Many pediatricians will do locum stints on the side (e.g., covering hospital shifts on weekends) to supplement income. It’s a trade-off: higher pay and freedom vs. benefits and stability.
Notably, some locum pediatricians enjoy the travel and varied experience, while others eventually seek a permanent position for a steadier routine. Overall, for those willing to be flexible, locum tenens can be a financially rewarding path in pediatrics.
Expected Salary Trends in 2025
Heading into 2025, expert forecasts predict modest growth in pediatric salaries. The physician recruiting firm Weatherby Healthcare notes that pediatric pay has increased two years in a row but still “remains among the lowest-paid specialties.” They reported pediatricians had 4% growth in 2023 and project continued increases, albeit not as dramatic.
By 2025, it wouldn’t be surprising to see average salaries in the low-to-mid $270,000 range for general pediatrics, assuming demand stays strong.
Some forecasts even suggest a potential leveling off: for instance, one compensation study projected a slight dip to ~$226,000 median by 2025, though this outlier may reflect conservative assumptions or median vs. mean differences. Most experts, however, anticipate continued upward pressure on pediatric pay due to physician shortages in primary care.
The AAP (American Academy of Pediatrics) and other groups have voiced concerns about fewer medical graduates choosing pediatrics, which could force employers to offer more competitive salaries to attract talent.
Another factor for 2025 is inflation and reimbursement changes. If healthcare reimbursement for pediatric services (office visits, immunizations, etc.) increases under new insurance contracts or government programs, practices might have more revenue to pay pediatricians. Conversely, tightening healthcare budgets could slow salary growth. Thus far, the outlook is positive: even after accounting for inflation, pediatric salaries in 2023 showed real growth.
Final Thoughts on Pediatrician Salaries
Pediatrician salaries vary based on experience, location, and workplace setting. On average, they earn a competitive income, with specialists and those in high-demand areas making more. While the profession offers financial stability, factors like student debt and work-life balance also play a role in career satisfaction.
Understanding these salary trends can help aspiring and current pediatricians make informed career decisions.
.jpg)
