Healthcare is facing a critical HR turning point. You’re managing higher turnover, more vacancies, and burnout levels that are pushing your staff to the edge.
At the same time, you're under pressure to maintain patient care standards, control costs, and respond quickly to union activity or new benefits expectations. Hiring takes longer, and the supply of experienced healthcare professionals is shrinking, especially in rural markets.
This article gives you a clear look at the numbers behind those problems. You’ll see what’s driving them, how others are responding, and which trends should shape your decisions going into 2025.
Let’s start with the numbers that define the current state of healthcare HR.
Key HR Statistics in Healthcare
Here are some of the most important HR statistics shaping healthcare workforce decisions in 2025:
- In 2024, the U.S. healthcare sector employed 18 million individuals.
- The U.S. is projected to face a shortage of 78,610 full-time RNs in 2025 and 63,720 by 2030.
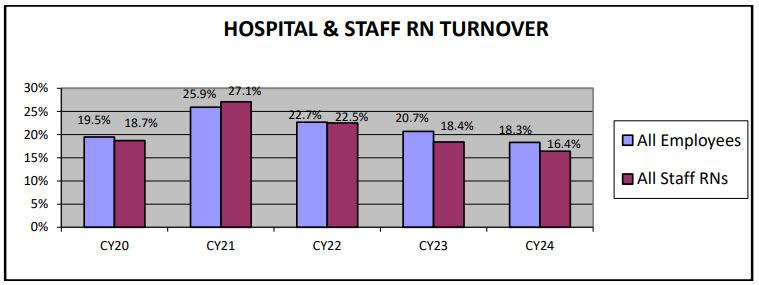
- The 2025 NSI report shows hospital turnover at 18.3% and RN turnover at 16.4% in 2024.
- According to a NCSBN report in 2025, 39.9% of RNs and 41.3% of LPN/VNs intend to leave the workforce or retire within five years.
- In 2024, nearly 60% of physicians said they would choose medicine again.
- In 2024-2025, 90% of physicians expect telehealth use to keep growing.
- In 2025, 97% of hospital systems plan to expand flexible work options.
- Around 63% of U.S. healthcare employers are offering sign-on bonuses in 2025.
- In 2025, RN turnover costs U.S. hospitals an average of $61,110 per nurse.
Healthcare Workforce Shortages: 2025 Data and Trends
Staffing gaps across the healthcare sector are creating risks for patient access, operational continuity, and cost control. These workforce challenges are growing more severe each year.
Here are nine data points that show how deep the staffing shortages have become and where the pressure is building the fastest:
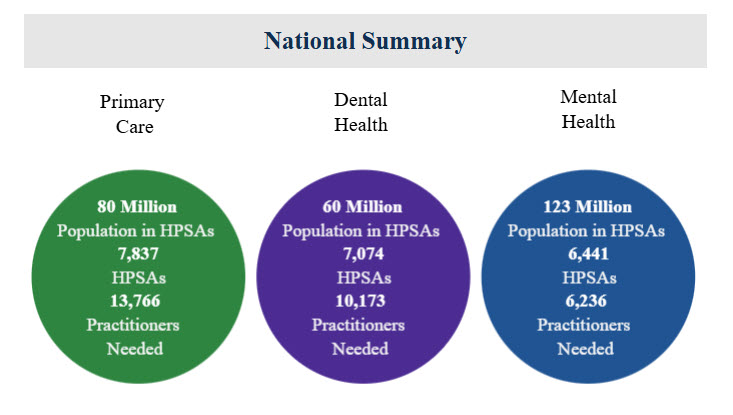
1. According to HRSA, 80M Americans live in primary care shortage areas. 60M live in dental health shortage areas. 123M live in mental health shortage areas.
As of mid-2024, millions of Americans lack reliable access to basic services because their communities are federally designated Health Professional Shortage Areas (HPSAs).
These gaps in access are especially serious in rural regions, where smaller hospitals and clinics struggle to attract licensed providers. The shortage affects both routine and crisis care delivery, which leads to longer wait times and delayed patient outcomes.
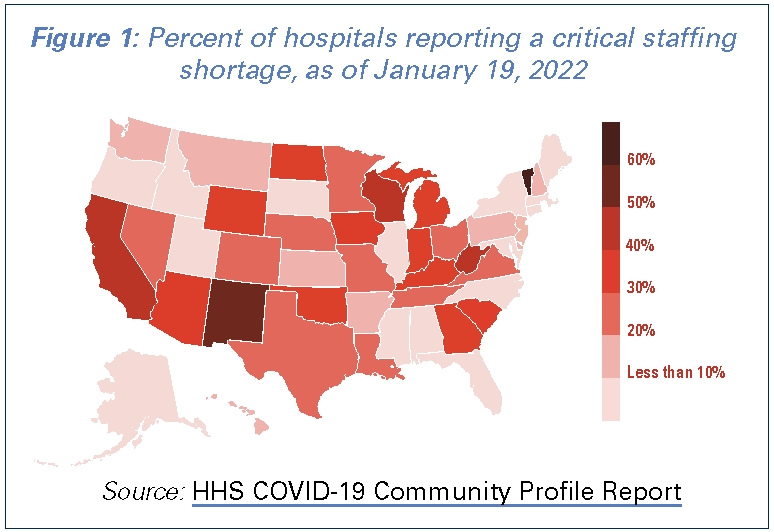
2. As of 2022, over 1,400 U.S. hospitals report critical staffing shortages. The matter is becoming more serious; 42 out of 50 states are projected to deal with critical shortages by 2030.
Roughly one-third of hospitals formally reported shortages in key roles. This included bedside nurses, respiratory therapists, imaging techs, and more.
These shortages disrupted staff scheduling, forced service delays, and required higher spending on contract labor. For HR teams, it has meant ongoing emergency hiring efforts and longer reliance on stopgap staffing models.
3. 94% of hospital CEOs cited RN shortfalls as a top concern.
For the first time since 2004, labor shortages topped the list of executive concerns. Registered nurses were identified as the most difficult role to staff, followed by allied health and physician specialties.
This reflects how workforce gaps are no longer just an HR problem. They are a board-level issue affecting budgets, compliance, and patient safety.
4. Over 500,000 RNs were projected to retire by 2022. By 2030, this number will increase to over 1 million.
This wave of retirement has already taken a visible toll. With so many experienced nurses leaving, hospitals face both hiring volume and experience gaps.
For example, early-career nurses usually require more support and supervision. This adds strain to existing staff and affects employee performance in high-acuity areas.
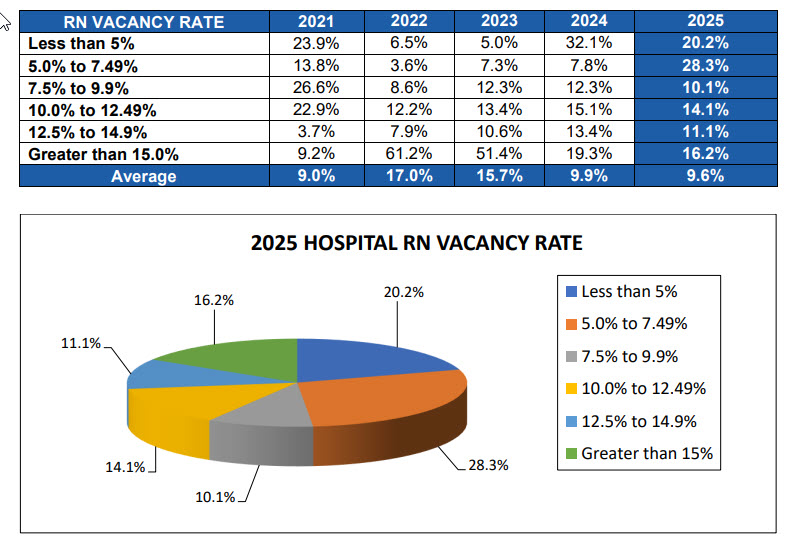
5. RN vacancy rates hit 9.6% in 2025.
Despite recent hiring efforts, the average hospital still had nearly 1 in 10 RN roles unfilled in 2025. Over 40% of hospitals reported vacancy rates above 10%.
That level of shortfall drives up overtime, worsens employee burnout, and pushes more staff toward resignation. In many hospitals, this has become a cycle that threatens job satisfaction and quality care.
6. The U.S. faces a physician shortage of up to 124,000 by 2034.
According to AAMC projections, the shortage spans both primary care and specialty fields. Contributing factors include limited residency slots, an aging clinician base, and rising demand from older patients.
More than 40% of today’s physicians will reach retirement age in the next decade. This leaves a leadership and experience gap that weakens the U.S. health system over time.
7. Skilled nursing facilities have 8.3% fewer staff than pre-pandemic levels.
SNFs have struggled to recover their workforce since 2020. Lower pay, physically demanding work, and high infection risk have pushed many out of these roles. For long-term care administrators, the staffing issue affects both admissions capacity and quality ratings tied to patient satisfaction.
8. Ancillary/support roles face a 4.6M worker gap by 2026.
Roles like nursing assistants, home health aides, and patient transporters are seeing the sharpest exits.
According to Mercer, 6.5 million are projected to leave these jobs by 2026, and only 1.9 million replacements are expected to enter. This 4.6 million shortfall creates operational strain on nurses and contributes to a fragmented continuum of care.
9. Behavioral health may lose 400,000 workers by 2026.
Demand for behavioral health services is rising, yet the workforce pipeline isn’t keeping up. An estimated 400,000 mental health workers (many of them mid-career clinicians) are likely to exit the field by 2026. Without expanded training and development, this sector faces severe access issues, especially for Medicaid and safety-net populations.
Burnout in Healthcare Workers: Statistics and Impact on Well-being
Long hours, emotional strain, and persistent understaffing have taken a measurable toll on healthcare workers. These issues aren’t isolated but widespread and growing across roles and settings.
Here are the key data points that reflect how burnout is affecting your teams’ stability, morale, and long-term commitment to the healthcare system:
10. Half of healthcare workers felt burned out in 2024.
Half of healthcare workers reported burnout, with many of them also saying they felt overworked. These signs highlight structural risks within the work environment, especially for hospitals lacking support systems like dedicated wellness programs or flexible scheduling tools.
11. Physician burnout peaked at 62.8% in 2021.
Burnout among physicians rose sharply during the pandemic, with over 6 in 10 reporting symptoms in 2021. That’s a steep rise from 38% just one year prior. The causes ranged from stress to staffing shortages and delayed patient health care. These are conditions that directly threaten long-term physician retention.
12. Over two thirds of nurses report burnout multiple times a week in 2025.
That number is up considerably. In 2022, nearly 1 in 5 nurses said they experienced burnout several times weekly, while a quarter reported feeling burned out every day.
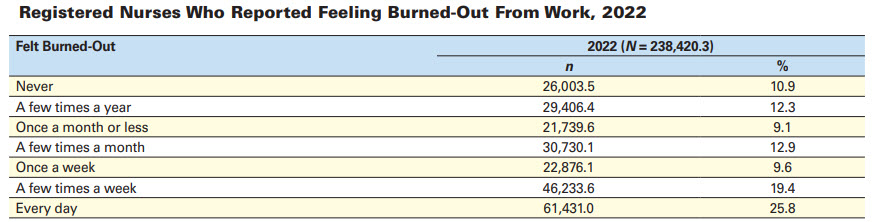
These levels of emotional exhaustion put nurses at high risk for errors, absenteeism, and reduced employee performance, all of which impact safety and staffing continuity.
13. 31.5% of nurses who leave their jobs quote burnout as their main reason.
However, burnout is the dominating factor for nurses working over 40 hours per week. The growing strain impacts retention, job satisfaction, and patient care. This also makes nurse well-being a key focus in workforce planning.
14. According to a recent study, 74% of nurses reported anxiety and 70.08% reported depression.
These figures come from surveys that found frontline workers dealing with high levels of mental distress. Without targeted mental health support, the rising anxiety and depression rates can weaken employee experience and drive even higher turnover.
15. There are 13.2 physical assaults and 38.8 non-physical violent events per 100 nurses each year.
More recent data is not available at the time of this writing, although 13.4% of healthcare workers experience workplace harassment in 2022. At that time, incidents of harassment had nearly doubled from 2018 levels, and this number is growing.
Verbal abuse, inappropriate behavior, and staff conflict have become more common, particularly in strained units. For HR management, this increases legal risk, erodes organizational culture, and makes recruiting into these environments harder.
16. 65% of nurses reported verbal or physical assault by patients or families.
Aggression toward nurses has grown, with 65% having reported some form of assault. Patients frustrated by long waits or policies usually take it out on staff. These events contribute to trauma and further destabilize healthcare human resources teams already managing exit risks.
17. According to the Journal of General Internal Medicine, 28.7% of healthcare workers (41% of nurses) intend to quit within 2 years.
Nearly one-third of workers (and over 40% of nurses) said they planned to leave their jobs by 2025. The consequences are loss of institutional knowledge, training costs, and added strain on recruitment and staffing efforts already under pressure.
18. 44.2% were actively job-hunting in 2022. More recently, 40% of them were looking for new roles within their organizations.
Beyond intent to leave, nearly half of healthcare workers were already looking for new jobs in 2022. This suggests a volatile workforce environment where even passive turnover can quickly become active attrition if HR teams don't respond with stronger engagement and retention strategies.
19. Only 57.1% of doctors would choose medicine again.
A stark drop from 72% in 2020, this statistic points to falling morale among physicians. It reflects how systemic stress from administrative burdens to burnout has made the role feel unsustainable. That sentiment makes it harder to attract new talent and retain experienced staff in medical practices.
Healthcare Recruitment and Retention: 2025 Challenges and Solutions
High turnover, long hiring timelines, and rising labor costs continue to pressure hospital budgets and planning strategies. Leaders are looking for ways to control spending while keeping clinical roles filled.
These are the current realities shaping recruitment and retention across U.S. hospitals:
20. Since 2016, 83% of RNs have turned over at least once.
Over several years, the majority of registered nurses left or changed roles at least once. This signals instability in core staffing and weakens continuity of care. It also forces repeat spending on hiring, onboarding, and training needs across the same positions.
21. 62% of hospitals saw more nurse exits in 2023.
In a year-over-year comparison, most hospitals reported a rise in nurse departures, especially among early-tenure staff. These exits add pressure on HR teams to rethink orientation, scheduling flexibility, and how to retain talent past the 12-36 month risk window.
22. Hospitals need 62-103 days to hire an experienced RN.
Time-to-fill varies by specialty, but hospitals report needing two to three months to replace one RN. That lag time leaves care units short-staffed and increases overtime burdens. Efficient workforce planning tools and clinical partnerships are now essential to reduce gaps.
23. Every RN lost costs about $40,038.
When a bedside nurse leaves, the total cost (including recruiting, onboarding, and lost productivity) averages over $40K. These losses stack quickly when turnover spikes. Tying investments to employee engagement and well-being can reduce the exit rate and protect staffing budgets.
24. Hospitals can save $3,083,600 by retaining 20 staff nurses instead of hiring travelers.
Travel nurses cost significantly more per hour, typically double or triple staff pay rates. Replacing just 20 travelers with retained staff can save over $3 million per year. Long-term savings depend on building better support systems and career advancement opportunities.
25. Travel nurse pay dropped to 42% from the pandemic peak.
Pay for travel RNs has come down as demand leveled off from emergency highs. This shift gives human resource management teams room to rebalance budgets and shift funds back toward permanent hires, internal float pools, and long-term retention incentives.
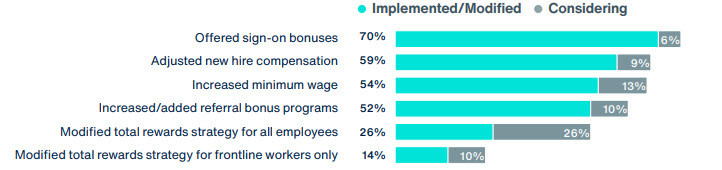
26. According to BenefitsPRO, 70% of hospitals increased starting pay in 2023, and 54% raised minimum wages for support staff.
Hospitals responded to labor competition by adjusting wages. These adjustments help attract candidates in a tight market but also raise baseline costs. Clear compensation frameworks and tools can help you track equity and align pay to tenure.
Healthcare Workforce Demographics and Diversity Stats
Demographic shifts are reshaping workforce planning across health systems. Aging clinicians, international workers, and racial representation gaps all play a role in how hospitals build long-term capacity and improve equity.
Here are the key data points to guide your diversity and inclusion strategies:
27. 88.5% of RNs are female.
The RN workforce remains overwhelmingly female. While male representation has grown slightly, nursing still reflects a narrow gender distribution. This can affect workplace dynamics and calls for intentional recruitment from diverse backgrounds, especially in leadership and advanced practice roles.
28. 38% of physicians are female.
Though progress has been made, women still account for less than 40% of practicing physicians. Closing this gap depends on mentorship, training and advancement pathways, and inclusive promotion policies across specialties with historically low female representation.
29. 34% of RNs are Baby Boomers who will reach retirement by 2030.
A third of the RN workforce is nearing retirement age. As these experienced clinicians exit, hospitals risk losing institutional knowledge unless talent development efforts, such as preceptorships and knowledge transfer programs, are actively built into succession planning.
30. 20% of doctors were 65+ in 2024.
One in five physicians is already beyond the traditional retirement threshold. Specialties like pulmonary medicine are aging faster than others. This makes pipeline expansion and early-career retention an urgent focus for long-term human resources strategy.
31. 18.2% of U.S. RNs are foreign-born.
Nearly one in five nurses working in the U.S. were born outside the country. These workers bring valuable language skills and cultural insight but may also require tailored onboarding and credentialing support to meet regulatory compliance standards.
32. 24.7% of U.S. physicians are international graduates.
International medical graduates (IMGs) play a significant role in healthcare delivery, especially in underserved areas. Recruiting and retaining IMGs requires hospitals to invest in legal support, clinical reentry programs, and fair access to training institutes and leadership roles.
33. In 2024, RN racial breakdown: 67% White, 11% Black, 9% Asian, 9% Hispanic.
Nursing shows increasing racial diversity. While Hispanic and Black representation has increased slightly, gaps persist when compared to the general population. Supporting inclusive hiring requires updated sourcing practices and better partnerships with collaborative working environment networks.
34. In 2024, the physician racial breakdown was 65.6% White, 18.1% Asian, 8.9% Hispanic, and 4.7% Black.
By comparison, in 2022, the physician racial breakdown was: 56.5% White, 18.8% Asian, 6.3% Hispanic, 5.2% Black. We can note a considerable decrease in White physicians. Asian and Black physician numbers have also decreased, while Hispanic increased.
Physician diversity also varies widely across specialties. For hospitals aiming to meet diversity, equity, inclusion, and belonging benchmarks, improving representation among leadership and faculty can help build more inclusive care environments and address patient trust gaps.
35. According to the U.S. Bureau of Labor Statistics, 34% of nursing assistants and 28% of home health aides were Black in 2022.
Statista presents similar numbers: quoting 37% of nursing assistants as being Black and 40% as being White. Healthcare support roles, such as aides and assistants, are more racially diverse than clinical leadership positions. This disparity highlights the need for stronger career pathways that help frontline workers advance into supervisory, licensed, or leadership roles across the organization.
Healthcare Training and Development Trends
Workforce expansion is only as strong as the pipeline behind it. From medical school seats to hospital reimbursement policies, training investment plays a direct role in how fast you can scale and stabilize staffing.
Here are the training and development figures shaping workforce growth in 2025:
36. According to HRSA, medical school enrollment rose 6% between 2019–2024, a 14% rise in female med students during that time, and new RN grads grew 36.1% from 2019-2023.
Between 2019 and 2024, education pipelines have expanded steadily. More medical and nursing graduates are entering the field, especially women. These increases create opportunities for training programs that accelerate readiness and align with real staffing gaps across departments.
37. 13,000 qualified nursing applicants were turned away in 2024 from graduate programs.
Despite rising demand, tens of thousands of qualified nursing students couldn’t enroll due to faculty shortages and limited clinical space. Hospitals that partner with training institutes or preceptor programs can play a direct role in solving this supply bottleneck.
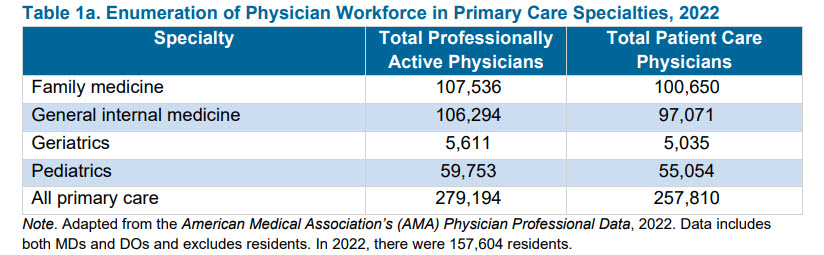
38. 157,604 physicians were in residency in 2022. In 2024, there were 162,644 active residents and fellows.
The number of residents continues to rise, but growth varies by specialty. Without targeted training rotations or rural incentives, many areas will still face shortages. Long-term talent development planning must include post-grad training access, not just degree output.
39. 95% of hospitals offer tuition reimbursement.
Education assistance is now a near-standard benefit. These reimbursement programs help retain early-career staff, upskill internal teams, and support employee relations management goals. Forward-thinking hospitals link reimbursement to high-need roles or future leadership development tracks.
40. Federal spending on behavioral health training hit $253.6M in FY2024.
Behavioral health workforce programs received a $56M boost in 2024, funding training for roughly 15,500 professionals. This surge reflects a growing demand for psychiatric care and signals the need for internal performance management plans to retain newly trained staff.
41. 72.7% of hospitals plan to expand their workforce in 2025.
Most hospitals say they’ll grow their staff over this year, either through hiring or internal development. That puts pressure on human resources leaders to align education, technology, and budget to build sustainable talent pipelines without increasing churn risk.
HR Technology and Automation in Healthcare: 2025 Insights
Digital tools have moved from optional to essential in healthcare HR. But adoption remains uneven. These statistics show where automation is helping and where gaps still hold teams back.
42. There are currently over 116 million users of online physician consultations at a global level.
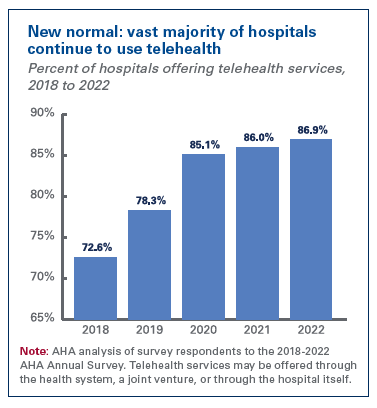
This trend kept increasing after the 2019 COVID pandemic. In fact, 74% of physicians used telehealth in 2022, up from 14% in 2018.
The surge in physician telehealth adoption reflects broader changes in care delivery and workforce flexibility, especially for rural systems or specialists working across locations. It also signals lasting infrastructure investments in virtual health.
43. 76% of US hospitals currently provide telehealth, and most Medicaid programs cover it.
This number represents a slight decrease because 86.9% of hospitals offered telehealth services in 2022. Even so, the number is up from 72.6% in 2018. For HR leaders, this expands hiring opportunities beyond geography but also requires updated onboarding, credentialing, and performance policies to manage remote or hybrid care teams effectively.
44. 93% of employers report efficiency gains after automating hiring.
Organizations that adopted tools like applicant tracking systems, AI screening, or automated scheduling saw measurable results. Time-to-fill dropped, team workloads eased, and budget use improved. But only those with the right infrastructure and change management saw these gains stick.
45. Only 69% of HR tasks are currently automated across providers.
While automation improves speed and accuracy, most healthcare HR departments still rely heavily on manual work. With workforce gaps widening, automating repetitive HR tasks such as benefits admin or compliance tracking can reduce overhead and free teams to focus on retention.
Healthcare Compensation and Benefits Statistics
As turnover risk rises and talent pools tighten, hospitals are rethinking how they attract and retain staff. These figures reflect how wages and benefits have shifted across the sector.
46. According to Health System Tracker, SNF wages rose 26.5% in the same period, and hospital wages rose 20.3% from Feb 2020 to Jan 2024.
Compensation increased sharply during this period, especially in skilled nursing, where pay jumped 26.5%. Hospital workers saw a 20.3% increase. These shifts reflect growing demand and difficulty staffing certain care settings despite ongoing financial constraints.
47. According to an Aon survey, 70% of hospitals use sign-on bonuses, 52% added referral bonuses, and 54% raised minimum wage.
Hospitals expanded short-term financial incentives to compete in a tight labor market. Sign-on and referral bonuses are now common, and over half of the organizations raised base pay for frontline roles to improve recruitment and retention outcomes.
48. Aon reported that 77% of hospitals offered more hybrid (virtual and office) work and 56% offered flexible hours (day start or end) in 2023.
Workplace flexibility has moved from perk to expectation. Many hospitals adapted, offering hybrid work for eligible roles and flexible hours for clinical staff. These changes help reduce burnout and appeal to younger workers prioritizing schedule control.
49. Aon also reported that 89% have access to mental health services and providers in 2023.
Support for mental well-being is becoming standard. Nearly nine in ten hospitals offered employees mental health resources last year. These include in-network providers, EAPs, or partnerships with virtual behavioral health platforms.
50. BenefitsPRO reports that 35% of hospitals added gender-affirming care benefits in 2024, and 15% are considering it.
Hospitals are expanding inclusive benefit offerings. A growing number now support gender-affirming services, from hormone therapy coverage to mental health support, as part of broader diversity and equity goals across HR and benefits policy.
51. 45% of hospitals offer paid parental leave.
Nearly half of hospitals now provide paid parental leave beyond legal requirements. This policy helps with the retention of early-career clinicians and contributes to a more supportive work culture for employees starting or growing families.
52. 36% of hospitals offer student loan repayment.
Loan repayment programs are growing in popularity, especially for nursing and allied health roles. These benefits can improve recruitment outcomes in underserved areas and help hospitals compete for early-career candidates facing high debt burdens.
Turnover Rates and Labor Activity in Healthcare
Labor pressures in healthcare are escalating. From rising resignations to increased strike activity, organizations are facing growing disruption in both clinical and support roles.
53. RN turnover is 13.5% in 2025.
That number represents a steady decrease. In fact, RN turnover reached 16.4% in 2023, also down from 27.1% in 2021.
Turnover among registered nurses has eased but remains a top priority. While the rate dropped from a pandemic peak of 27.1% to 16.4% in 2023 and 13.5% in 2025, it’s still high enough to disrupt continuity, drive up hiring costs, and affect patient outcomes.
54. Healthcare’s quit rate hit 6.4% in November 2021, which is the second-highest of any industry.
At the height of pandemic fatigue, healthcare saw one of the highest quit rates across all sectors. In November 2021 alone, 6.4% of workers in healthcare and social assistance left their jobs, a signal of deep systemic stress. Currently, the voluntary termination rate represents 95.4% of the turnover rate.
55. In 2024, 13% of healthcare workers and 20% of nurses are unionized.
This shows an increase over the past few years. According to the Bureau of Labor Statistics, only 6.8% of health workers were unionized in 2023.
Even so, despite growing labor unrest, most healthcare workers remain non-unionized. Union participation in this sector is above the national average, but is still low. This limits collective bargaining power for frontline staff facing rising workload and burnout pressures.
56. The Bureau of Labor Statistics also reported practitioner union density of 12% and support roles of 8.2%.
Union presence varies sharply by role. While 12% of healthcare practitioners and technical staff were union members in 2023, just 8.2% of support workers were covered. This uneven representation affects how different teams can negotiate for safer staffing or better pay.
57. There were 17 healthcare strikes by mid 2025. That’s an increase from 8 major healthcare strikes in 2022, followed by 6 more in early 2023.
Labor activity in healthcare accelerated quickly. Eight large-scale strikes occurred in 2022, involving tens of thousands of workers, and six more followed in the first half of 2023. Becker’s Hospital Review reports over 17 strikes in 2025. Most centered on short staffing, unsafe conditions, and pay disputes.
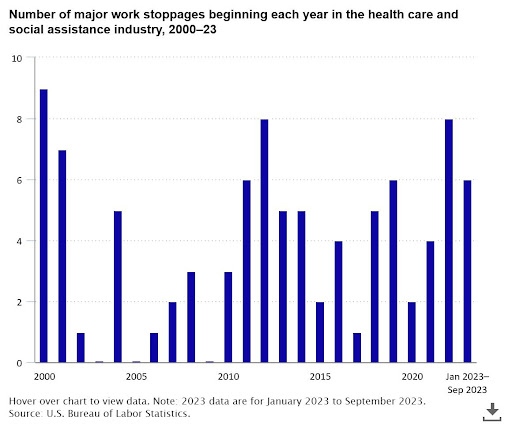
58. In 2024, 33 healthcare strikes involved 62,232 workers (24% occurred in California).
Healthcare labor actions became more frequent and widespread in 2024. Thirty-three strikes occurred across 13 states, with California alone accounting for nearly a quarter. This reflects how staffing and wage issues are converging with regional policy and cost-of-living dynamics.
59. Over 75,000 workers joined the largest healthcare strike in U.S. history in October 2023.
In October 2023, Kaiser Permanente faced an unprecedented labor action as more than 75,000 employees walked off the job. The action, driven by concerns over understaffing and pay equity, marked a turning point in national healthcare labor negotiations.
60. 47% of healthcare workers plan to leave their positions by 2025.
Nearly half of healthcare workers have considered exiting their jobs within this year. If this trend holds, it could intensify existing workforce shortages and create a major strain on care delivery, HR planning, and financial forecasting.
61. Healthcare labor expenses rose by $42.5 billion between 2021 and 2023.
The cost of employing healthcare workers is rising fast. From wage hikes to contract labor, labor expenses surged by $42.5 billion in just two years. For most health systems, this creates serious challenges in balancing budgets while meeting care demands.
Looking Ahead: Turning Healthcare Data Into Action
The numbers confirm what leaders already know: healthcare is under pressure. Talent gaps, rising labor costs, and burnout are straining your teams and budgets. These challenges won’t ease without focused intervention.
That’s where AAG Health can help. We specialize in solving high-impact recruitment problems across health systems, from RN staffing to executive hiring. Whether you’re rebuilding core teams or addressing hard-to-fill specialties, our model prioritizes speed, cost-efficiency, and long-term fit.
If your organization is ready to take a more strategic approach to healthcare hiring, reach out to AAG Health today. We’re ready to support your workforce goals for 2025.
.jpg)
