Hiring and keeping qualified healthcare professionals is getting more expensive by the year. Rising turnover rates, long vacancies, and growing incentives are putting direct pressure on your workforce budgets.
The truth is, every delay in the hiring process chips away at revenue and stretches already limited resources across your teams. Without clear data, it’s hard to plan, justify spend, or measure which strategies actually work.
In this article, we'll bring you hard numbers on what recruiting and retention really cost across roles like RNs and physicians. You’ll see where the money goes, how fast it adds up, and what you can do to control it.
Let’s start with the key numbers shaping your staffing costs today.
Key Healthcare Recruiting and Retention Statistics
Staffing costs don’t just appear on paper. They show up in lost revenue, strained teams, and delayed patient care. These numbers give you a clear sense of just how costly it’s become to recruit and retain healthcare professionals in today’s environment:
- According to the 2025 NSI National Health Care Retention & RN Staffing Report, it costs $61,110 to cover the turnover of one bedside RN.
- A vacant primary care physician role can lead to roughly $1 million in lost revenue annually.
- The 2025 NSI report says that a hospital loses about $4.75 million per year due to RN turnover on average.
- According to AMN Healthcare, physicians receive an average signing bonus of $31,473, while NPs and PAs average $11,758.
- The 2025 NSI report notes that for every 1% change in RN turnover, the average hospital gains or loses around $289,000 annually.
Healthcare Recruitment and Vacancy Cost Statistics
Healthcare hiring costs go far beyond salaries. Delays, incentives, and inefficiencies are draining budgets at every step. These are the numbers behind the growing cost of recruitment and vacancy management across healthcare systems:
6. 20-30% of first-year salary is the industry standard for physician recruitment fees by staffing and recruiting agencies.
Paying this much upfront cuts directly into budget flexibility. It also raises the stakes on getting each hire right the first time. If the candidate isn’t a long-term fit, the organization bears both the recruiting fee and the turnover cost.
Tip: For a deeper breakdown of how physician shortages are driving up recruiting pressure and what’s working to fix it, read our guide to physician shortages and recruiting challenges.
7. According to the 2024 Physician Hiring Trends Report, an unfilled healthcare role costs an average of $8,000 per day in lost productivity and revenue.
This figure usually surprises leadership, especially when multiple positions stay open at once. You probably already know that the ripple effect of one vacancy can stress remaining staff, increase burnout, and lead to additional resignations. That’s why vacancy costs need to be part of your larger workforce solutions strategy.
Kevin Jubbal, M.D., explains why so many primary care spots were left unfilled this year:
8. The Medix Team reported that hospitals lose $66,000 per week for an open neurosurgery role and $57,000 weekly for an unfilled gastroenterology position.
These are high-revenue specialties, so gaps leave revenue on the table daily. Delays also hurt patient access, which could impact quality scores and contracts. For many healthcare facilities, it’s not just about replacing a role but protecting core service lines.
9. Healthcare jobs take about 49 days to fill, typically longer than roles in other industries.
A long hiring cycle can stall care delivery and stretch your team thin. While other sectors may bounce back quickly, in healthcare, each extra day creates risk. That’s especially true in specialty areas, where a thin candidate pipeline slows hiring even more.
10. The average physician sign-on bonus across specialties is approximately $30,395, with a median of $20,000.
To stay competitive, you’re likely offering similar incentives, especially for hard-to-fill roles. But these bonuses add up fast when scaled across multiple hires. Without a strong retention strategy, they become expensive short-term fixes.
To help you out, we’ve outlined several practical ways to reduce bonus-driven churn in our guide to physician recruiting strategies in 2025, from retention committees to work-life incentives that actually stick.
11. According to the 2025 AAPA Salary Report, the median bonus for full‑time PAs is $7,500.
This number may seem modest compared to physicians, but it's a growing part of total hiring costs. As demand rises for advanced practitioners, even smaller incentives must be tracked to manage spend. It's one more line item worth forecasting accurately.
12. According to AMN Healthcare, physicians receive an average relocation allowance of $11,284, while NPs and PAs average $7,910.
Relocation support is standard, especially for cross-state hires. But with rising housing and travel costs, these allowances can fall short or require top-ups. In the end, they push your recruiting needs budget higher than planned.
13. AMN Healthcare also reports that physicians receive an average CME allowance of $3,969, compared to $2,195 for NPs and PAs.
These allowances may be necessary, but they increase the cost per hire, especially when included in multi-year contracts. They’re also not always used, which creates a budgeting gray area. Over time, underutilized CME dollars can skew your actual compensation spend.
14. Indeed data shows that 3.7% of all U.S. job postings in December 2024 offered signing bonuses.
This reflects a wider trend where incentives are becoming expected, not optional. What used to set you apart is now a baseline. For anyone in the healthcare staffing industry, this means incentive structures need to be updated regularly to stay competitive.
15. A 2024 study found that 54% of companies fully reimburse relocation costs, while 38% provide a lump-sum stipend.
You’ll likely need to offer one of these models to attract top talent across state lines. But these costs can escalate without tight controls. Even flat-rate packages usually need exceptions, which complicates budgeting and approval workflows.
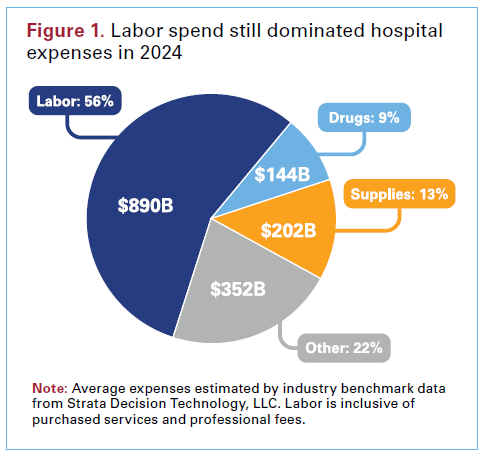
16. According to AHA’s 2025 report, hospital labor costs hit $890 billion in 2024, making up 56% of total operating expenses.
Labor is your largest single cost, and rising fast. That makes recruitment decisions incredibly high-stakes for financial leaders. Tighter cost control in healthcare staffing is one of the few levers you can pull to protect margins.
17. A survey of 105 healthcare talent leaders found that 57% are seeing longer time-to-hire compared to last year.
Hiring is slowing even as demand grows. It’s partly due to wider staff shortages, but also bottlenecks in internal approval and credentialing. Process improvements could shorten time-to-hire and help you compete better for limited talent.
.jpg)
18. In one survey, just 3% of new physicians preferred working in towns under 25,000 residents, while 84% favored communities with 100,000 or more.
That preference mismatch makes rural hiring significantly harder. To compete, rural employers typically need to boost bonuses and support, raising total costs. These areas may also depend more heavily on locum tenens, which inflates spend over time.
Healthcare Turnover and Retention Cost Statistics
Here are the most pressing statistics behind why retention also means protecting revenue and reducing churn. These are the real costs tied to turnover across the healthcare workforce:
19. According to the 2025 NSI report, the overall hospital turnover rate for all staff was 16.4% in 2024.
A rate this high signals more than dissatisfaction. It reveals a systemic issue that stretches HR teams and budgets thin. High turnover increases overtime reliance, delays onboarding, and disrupts nursing management schedules. Hospitals can’t afford to treat retention as an afterthought anymore.
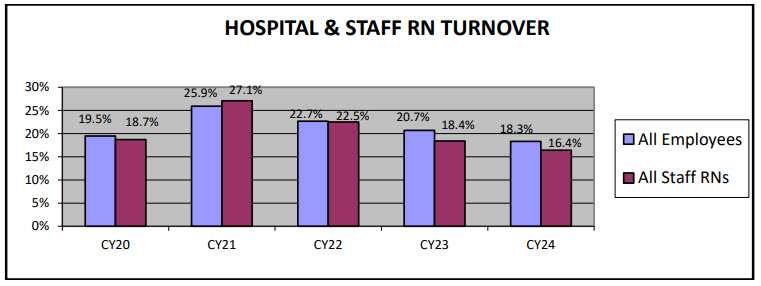
20. Across a five-year span, RNs in step-down, telemetry, and emergency units turnover at rates exceeding 110-121%.
Losing your entire nursing staff every 4-5 years creates instability in patient care delivery. These departments operate under pressure, and hence, they're more vulnerable to burnout and faster exits. That pace of churn also forces continuous recruiting cycles, which compound spending.
21. According to the AMA, physician burnout costs the system approximately $4.6 billion per year.
These costs don’t just come from resignations. They also include reduced work hours, lower productivity, and increased executive search activity to backfill roles. Burnout affects care quality and team morale, which makes this a strategic priority for C-suite leaders. Addressing it means going beyond surface-level fixes.
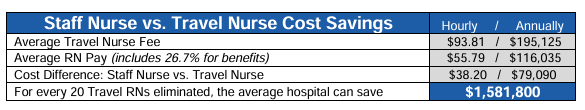
22. The 2025 NSI report notes that for every 20 travel RNs replaced by staff, a hospital can save approximately $1.58 million annually.
That savings figure is a clear argument for long-term hiring over short-term patches. Travel nurses fill urgent gaps but strain budgets quickly. Prioritizing permanent placement, where possible, stabilizes teams and reduces overall spending.
Pro tip: If you’re still relying heavily on temporary coverage, we break down the top travel nurse recruitment problems and what your team can do about them in this detailed guide on travel nurse recruiting challenges.
23. NSI’s report also shows that switching to full-time RNs from travel RNs can save hospitals $79,090.
Continuity matters just as much as cost. Full-time staff are more likely to stay invested in patient outcomes and organizational culture. Over time, this shift improves care quality while easing financial pressure.
24. A bad hire in 2025 can cost a company around 30% of that employee’s first-year salary.
These are hidden costs that add up fast, especially if hiring decisions are rushed. Poor performance, low morale, and repeat turnover stretch HR teams and inflate recruiting timelines.
Stronger vetting and onboarding practices can help avoid these expenses. To help you out, we’ve outlined how leadership hiring is shifting and what to do about it in our guide on healthcare executive recruiting trends.
25. One in five new hires leaves their job within the first 45 days.
Early exits usually point to mismatched expectations or poor onboarding. For organizations already battling healthcare turnover rate issues, this makes first impressions critical. Refining your orientation process could reduce early attrition significantly.
26. Hospital-employed hospitalists typically receive annual retention bonuses between $5,000 and $10,000, usually after three or more years on the job.
Bonuses like these signal that long-term loyalty still matters. But they must be paired with clear career paths and role support. Otherwise, they risk becoming short-term band-aids rather than real retention tools.
27. The 2025 NSI report also notes that 59.3% of hospitals reported having a formal retention strategy for nursing staff.
That means over 40% still operate without one, which is a missed opportunity. Without structure, retention efforts stay reactive and inconsistent. Formal strategies allow hospitals to benchmark progress and link retention to broader talent solutions goals.
Impact of Healthcare Understaffing on Patient Outcomes and Financial Risk
Understaffing doesn’t just stretch teams; it changes outcomes. According to a 2025 BMJ Quality & Safety study, patient safety, care quality, and hospital finances all take a direct hit when RN and NS coverage drops. These are the most urgent signals that short-staffed care environments come with real risk, based on the BMJ study:
28. Patients in understaffed RN units had a 5% death rate, compared to 4% in properly staffed units.
A 1% difference might sound small, but it represents hundreds of lives across larger systems. When RN capacity drops, the time and attention each patient receives narrows. For clinical leadership, even small gains in staffing can produce meaningful shifts in patient safety metrics.
Tip: For more ways to strengthen hiring and reduce safety risks, you can check out these six best practices for nurse recruitment in 2025.
29. Readmission rates were 15% for patients exposed to RN understaffing, versus 14% for those who weren’t.
Readmissions hit both finances and performance ratings. They also signal missed care opportunities that could have been addressed earlier. Even a 1% increase can influence contracts tied to value-based outcomes in the healthcare industry.
30. Patients stayed an average of 8 days in understaffed RN units, compared to 5 days in fully staffed units.
Longer stays increase costs and limit bed availability for new patients. This creates backlogs that affect every department. Better staffing ratios help move patients through the system safely and efficiently.
31. Those exposed to understaffing experienced an average 1.15-hour shortfall in RN care during the first 5 days.
These early hours are critical for care planning, medication management, and identifying complications. Missing that window means issues can escalate before being caught. Staffing gaps at the start of a stay usually set the tone for overall outcomes.
32. Patients not exposed to understaffing received an average of 3.36 more care hours above the ward average.
Extra time translates to more checks, clearer education, and stronger recovery support. What matters is not only volume but the impact made in each hour. That additional care can reduce downstream costs and boost quality assurance across the board.
33. Each day of RN understaffing in the first 5 days raised a patient’s risk of death by 8%.
This compounding effect makes early staffing levels especially urgent. If the first five days are understaffed, the risk adds up quickly. Systems should prioritize talent acquisition technology that helps predict and fill early-stage gaps faster.
34. Daily RN understaffing increased the chance of readmission by 1%.
Of course, this reinforces how important consistent staffing is, not just at discharge but throughout the stay. Even one understaffed day raises the likelihood of the patient coming back. Staffing decisions ripple beyond the current visit into future utilization rates.
35. When all 5 early hospital days were understaffed, patient length of stay rose by 69%.
This number dramatically shifts financial models. It means nearly doubling the expected duration of care, which throws off bed management, cost recovery, and operational planning. Better forecasting prevents this kind of disruption before it starts.
36. Each day of NS understaffing increased the risk of death by 7.2%.
Nursing support roles are usually overlooked in workforce planning. But this stat makes it clear that they’re just as critical to care delivery. Strategic investment in support staff should be a core part of professional staffing strategies.
37. NS understaffing led to a 60.8% increase in patient length of stay.
Longer stays add pressure to discharge planning, increase infection risk, and lower overall capacity. Support staffing plays a critical role in keeping throughput on track, not just in managing costs. Cutting these roles too deeply leads to delayed recoveries and squeezed margins.
38. Surprisingly, each day of NS understaffing reduced the risk of readmission by 0.6%.
This outlier may reflect patients staying longer upfront due to delayed care, which limits the need to return. But it’s not a good tradeoff since it signals inefficiency, not better outcomes. The better goal is right-sized care at the right pace from the start.
Making Smarter Workforce Investments Starts Here
Every vacancy, turnover, or staffing delay comes at a cost, and as you’ve seen, those costs compound fast. From recruiting expenses to extended patient stays, gaps in your team affect more than just coverage.
That’s why having the right strategy and partners matters. If you're looking to strengthen retention, reduce reliance on per diem staffing, or plan ahead for key roles, AAG Health can help.
Our recruitment, RPO, and consulting support can give you the structure to hire smarter and build lasting clinical talent pipelines. Reach out today to see how your team can move from reactive hiring to long-term workforce planning.
FAQs
What is more cost-effective, recruiting or retaining nurses?
Retaining nurses is generally far more cost-effective than recruiting new ones. That’s because hiring involves multiple expenses that quickly add up, such as job ads, interviews, sign-on bonuses, and onboarding. When you focus on retention, you’re protecting your investment in training and maintaining continuity in patient care.
How much does recruiting cost?
The average cost to hire an employee in the U.S. is about $4,700, but for clinical roles, that figure usually climbs much higher. This includes advertising, screening, relocation, and potential upfront fees. If you’re hiring RNs or physicians, expect that number to double or triple depending on the role and location.
What is the employee retention cost?
Employee retention costs are typically tied to programs like mentorship, continuing education, or benefits packages that keep staff engaged. These costs are steady and predictable, unlike the spikes that come with urgent recruiting. Investing in retention gives you more control over budgets and workforce stability in the long run.
What is retention in healthcare?
Retention refers to how long your nurses, physicians, or allied health professionals stay in their roles. High retention leads to lower training costs, fewer handoffs, and better patient outcomes. It’s one of the most reliable ways to reduce disruptions and increase efficiency across departments.
What is the most cost-effective source of recruitment?
Referral networks, internal pipelines, and long-term partnerships offer stronger value than one-off job ads or agencies. AAG Health, for instance, reduces repeat hiring by aligning candidates with your care standards from the start. Our full-service approach helps you hire effectively and keep positions filled longer, not just complete a contingent search.
Is nurse retention a problem?
Yes, and the numbers make it clear. First-year RN turnover is at 22.3% according to the 2025 NSI report, meaning many nurses don’t make it past month 12. That early churn is expensive, and solving it starts with better onboarding, scheduling, and team support.
.jpg)
