Rural communities face a serious shortage of Certified Registered Nurse Anesthetists (CRNAs). According to a study published in The Journal of Rural Health 58.1% of rural counties lacked a Certified Registered Nurse Anesthetist (CRNA), while 81.2% had no anesthesiologist.
The shortage of skilled CRNAs limits the ability of rural healthcare facilities to perform essential medical procedures and surgical services. This, in turn, impacts patient care and comfort, as many may need to visit facilities in urban centers, even for the simplest procedures.
But why is there such a shortage of CRNAs in rural healthcare?
Recruiting qualified CRNAs in such communities is a persistent challenge.
In this blog, we’ll cover exactly why hospitals and clinics in rural areas fail to attract and retain anesthesia providers and what they can do to solve the problem. You’ll also learn how collaborating with a healthcare recruitment agency can help bridge this critical gap.
What Is a CRNA?
A Certified Registered Nurse Anesthetist, or CRNA, is an advanced practice registered nurse (APRN) who administers anesthesia for various medical procedures.
To become a CRNA, a candidate must first earn a Bachelor of Science in Nursing (BSN) or a related degree and obtain a registered nurse (RN) license. They also need at least one year of full-time critical care experience before applying to an accredited nurse anesthesia program, which typically takes 36 to 51 months to complete.
Why Recruit CRNAs for Rural Healthcare?
Rural hospitals face significant challenges in maintaining surgical services due to a shortage of anesthesia providers. CRNAs play a crucial role in bridging this gap, especially in underserved areas.
Many rural hospitals operate under a CRNA-only model, which allows them to provide essential surgical and obstetric care while reducing patient travel times. According to the American Association of Nurse Anesthesiology (AANA), CRNAs make up over 80% of anesthesia providers in rural counties.
“Just as they are the predominant providers of anesthesia care in the military, CRNAs are the primary providers of anesthesia care in rural settings, providing care to patients where they live, when they need it most,” says AANA President Dru Riddle.
In 22 states of the U.S. and Guam, CRNAs can administer anesthesia without an anesthesiologist's supervision, which makes them a vital resource for critical-access hospitals. Their ability to operate independently helps ensure that rural healthcare facilities remain functional and accessible.

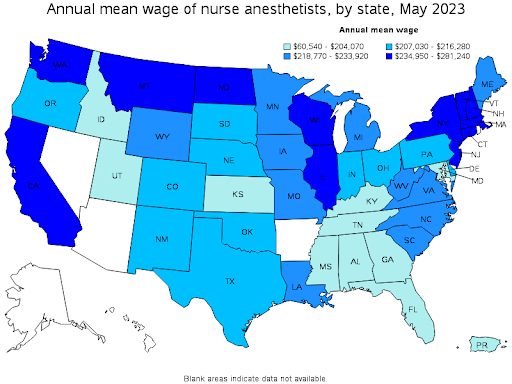
Beyond accessibility, hiring CRNAs is a cost-effective solution. When comparing anesthesiologist vs CRNA salaries, the difference is significant. The mean annual wage for nurse anesthetists is $214,200, whereas for anesthesiologists, it’s $338,470.
Since rural hospitals often have limited budgets, hiring a CRNA can be a better choice, financially. An article published in Nursing Economics concluded that hiring CRNAs is a cost-effective strategy for delivering anesthesia services.

Importance of CRNAs in Anesthesia Care
CRNAs play a critical role in delivering safe and effective anesthesia care across various healthcare settings. Their advanced education and specialized training equip them to provide anesthesia services, from preoperative assessments to postoperative management.
CRNAs commonly administer anesthesia for obstetrics, general surgery, and pain management. In many rural and underserved areas, they serve as the sole anesthesia providers, ensuring critical access to care.
According to the AANA, CRNAs safely administer over 58 million anesthetics annually in the U.S. This shows their essential contribution to patient care.
Moreover, studies have consistently demonstrated that CRNAs deliver anesthesia with a safety record just like physician anesthesiologists. A study published in Health Affairs found no statistically significant differences in patient outcomes when anesthesia care was provided by CRNAs compared to anesthesiologists.
Why Is Rural CRNA Recruitment More Difficult Than Urban Recruitment?
Compared to their urban counterparts, rural healthcare facilities face significant challenges in recruiting CRNAs.
One of the biggest hurdles is the limited local talent pool. Rural communities have smaller populations, so fewer trained anesthesia professionals are available nearby. This forces hospitals to recruit externally, often making hiring more difficult and time-consuming.
Secondly, with their limited resources, they fail to attract CRNAs, who would instead work in a city rather than a small town to get compensated more.
A meta-analysis published in the Journal of Rural Studies identified three major barriers to recruiting and retaining nurses in rural areas:
- Higher health service demands
- Rural demography
- Challenges of accessing continuous professional development and clinical progression restrictions
The analysis also highlights that “Nurses in rural areas require a different generalist skillset which can be challenging for new or urban nurses to achieve.” This suggests that the current training model may not fully prepare nurses for the demands of rural practice.
To attract nurse anesthetists, leaders in rural healthcare facilities need to match the financial compensation of their urban counterparts and incentivize the rural lifestyle by promoting its benefits.
Challenges of Rural CRNA Recruitment
Now let’s look closely at the various obstacles in CRNA recruitment in rural areas:
1. Shortage of Anesthesia Providers
There has been a shortage of anesthesia providers nationwide for a while. However, rural hospitals have experienced an even more pronounced shortage. And this trend is expected to continue well into the next decade.
According to AANA, the anesthesiology industry may see a shortage of over 12,500 workers by 2033, representing a gap of 22% in staffing needs.
As the pool is already small, rural healthcare facilities struggle to hire enough nurse anesthetists to meet their needs.
2. High-Stress Levels and Long Working Hours
CRNAs in rural healthcare settings frequently encounter high-stress levels and extended working hours. The limited number of anesthesia providers means that CRNAs handle a substantial patient load, which can lead to work-life balance challenges.
Additionally, the necessity for on-call duties can further contribute to professional burnout.
Research shows that high-stress levels and burnout significantly increase the likelihood of nurses leaving their jobs.
3. Barriers to Career Growth
Professional isolation is a common challenge for CRNAs in rural healthcare environments. The lack of mentorship opportunities and limited access to specialized training programs can hinder career advancement. This isolation may discourage skilled professionals from pursuing or continuing careers in rural locations.
In contrast, CRNAs working in urban centers have access to opportunities to advance their careers through further education and development programs. For instance, there are more educational institutes in urban areas than rural areas, which makes the former more attractive.
4. Job Security and Satisfaction Concerns
Another big challenge for rural healthcare organizations when recruiting CRNAs is financial instability. Many candidates perceive rural jobs as less secure, as budget constraints can lead to funding cuts, reduced staffing, or even hospital closures.
Moreover, limited resources and fewer professional development opportunities may impact job satisfaction. Without access to modern equipment, mentorship, and career growth, CRNAs may feel less supported in rural facilities compared to urban hospitals.
Strategies for Effective CRNA Recruitment
Recruiting CRNAs for rural hospitals and clinics requires targeted strategies to address the unique challenges of these environments. Below, we have shared some effective approaches to improve both the recruitment and retention of these skilled professionals:
1. Develop a Formal Recruitment Plan
A structured recruitment plan is essential for attracting CRNAs to rural hospitals. It should include clear objectives, timelines, and responsibilities to ensure a systematic approach to identifying and engaging potential candidates.
Use data analytics tools such as LinkedIn Talent Insights and HireVue to assess the effectiveness of recruitment efforts and refine strategies accordingly.
For instance, track metrics such as the number of applicants, interview-to-offer ratios, and time-to-fill positions to gain valuable insights into the recruitment process. Improve the process along the way.
Moreover, you can partner with CRNA staffing agencies to access a broader pool of candidates. A reliable recruitment partner can streamline the hiring process and identify CRNAs who are well-suited for the challenges of rural healthcare.
2. Promote Location-Advantages
Highlight the unique benefits of working in rural healthcare settings to attract CRNAs seeking diverse experiences. The aspects that make rural healthcare jobs different from urban ones can be used to promote the job. It’s all about changing the perspective.
For instance, rural nurse anesthetists have more autonomy. A study by the University of Minnesota Rural Health Research Center found that rural nurses have more autonomy in every aspect of their job compared to their peers working in urban locations.
Nurses appreciate this autonomy as confirmed by a survey conducted in Nebraska. Rural nurses surveyed rated the following aspects higher compared to their urban counterparts:
- Autonomy
- Positive CRNA/surgeon relationships
- Opportunity to improve professional skills
- Opportunity to meet professional goals
- Ability to practice anesthesia as trained.
Besides career advantages, emphasize the lower cost of living and tight-knit communities in country settings. According to the AANA, practicing in rural areas gives CRNAs a broader scope of practice and greater professional independence.
3. Competitive Compensation
Offering attractive salary packages is crucial in addressing workforce shortages in rural healthcare organizations. Research indicates that competitive compensation is a significant factor in recruiting and retaining CRNAs.
It’s understandable that a rural healthcare facility may be unable to match the salary with an urban hospital with a large endowment. However, they can remain competitive by emphasizing non-monetary benefits.
To make up for that, try highlighting the lower cost of living that nurses can enjoy by living in a small town.
Similarly, offer other financial incentives to compensate for the lower salary, such as free professional development or a sign-up bonus.
4. Loan Forgiveness and Scholarship Programs
Financial incentives play a significant role in attracting and retaining CRNAs in rural areas. Loan forgiveness programs, such as the National Health Service Corps (NHSC) Rural Community Loan Repayment Program, offer up to $100,000 for full-time service in eligible rural healthcare facilities.
Similarly, state-specific initiatives like Georgia's Advanced Practice RN Loan Repayment Programs award up to $10,000 per year for service in underserved areas.
Such programs ease the financial burden of education loans, making rural healthcare jobs more attractive to skilled anesthesia professionals.
5. Ensure Work-Life Balance
Work-life balance is essential for job satisfaction and retention. Rural healthcare facilities can improve it by offering flexible scheduling, providing adequate support staff, and setting reasonable on-call expectations to help reduce burnout. For example, you may allow CRNAs to have more control over their schedules.
Hospitals that introduced greater flexibility have seen higher nurse retention rates. For example, post-COVID, several hospitals were able to bring back 25% of their nurses by simply allowing more flexibility in their schedules and duties.
How to Support CRNA Professional Development in Rural Healthcare Settings?
Since career stagnation is a big concern for CRNAs, offering support for professional development can be a surefire way to recruit and retain them.
Here are some ways that can help you promote career growth:
1. Continuous Education Opportunities
Providing access to continuous education is crucial for CRNAs to stay updated with advancements in anesthesia techniques and medical procedures. Given the potential for professional isolation in rural locations, healthcare facilities can use online platforms and virtual conferences to facilitate ongoing learning.
For instance, programs like the Rural Education and Learning (REAL) initiative offer healthcare providers opportunities to broaden their knowledge in ways that serve both personal interests and community needs.
Additionally, mentorship is especially valuable for rural CRNAs as it helps them adapt to unique challenges. Studies show that nurses with mentorship opportunities experience higher job satisfaction and lower turnover rates.
Pro tip: Encourage peer learning by setting up virtual discussion groups where CRNAs can share insights, case studies, and new anesthesia techniques. This creates a collaborative learning environment, even in remote areas.
2. Training Programs for Rural Practice
Tailored training programs that address the specific challenges of rural healthcare environments can better prepare CRNAs for their roles. For example, George Fox University's CRNA program aims to train healthcare professionals to address disparities in rural anesthesia care while integrating compassionate, faith-driven service into their practice.
Such programs equip CRNAs with the skills to handle the unique dynamics of rural hospitals and healthcare delivery systems. More importantly, CRNAs can learn to work with patients from these often relatively small and tight-knit communities.
Pro tip: Partner with urban hospitals or academic institutions to offer rural CRNAs short-term exchange programs. This allows them to gain hands-on experience in diverse settings while bringing back valuable skills to their rural practice.
The Future of CRNA Jobs in Rural Healthcare (2025 and Beyond)
The demand for CRNAs in rural healthcare settings will rise significantly in the coming years.
According to the US Bureau of Labor Statistics, employment of nurse anesthetists is expected to grow by 40% from 2022 to 2033, a rate much faster than the average for all occupations. This surge is attributed to an increased demand for healthcare services, including elective surgeries.

As mentioned earlier, there’s an expected continuation of the shortage of CRNAs in the thousands. That makes the situation even more concerning for rural healthcare leadership, as their facilities need the CRNAs the most.
After all, nurse anesthetists ensure that rural hospitals can offer essential medical procedures and surgical services while maintaining the quality of care for underserved populations.
Educational Advancements and Requirements
From 2025 onward, all newly certified CRNAs will be required to hold a doctoral degree. This change aims to enhance clinical training and expertise by equipping nurse anesthetists with advanced skills.
For rural healthcare organizations, this advancement means access to highly skilled professionals capable of addressing complex patient care needs.
Technological Integration and Telehealth
Integrating telehealth and other technological advancements is poised to transform anesthesia departments in rural healthcare organizations. These tools can enhance patient care by facilitating remote consultations, continuous education, and collaboration among healthcare providers.
Embrace such technologies to mitigate some common challenges associated with rural healthcare delivery, including limited access to specialized medical services.
Secure Top CRNA Talent for Your Rural Facility with AAG/H
Addressing the shortage of CRNAs in rural areas requires targeted strategies, from competitive compensation to community integration efforts. You can create a sustainable CRNA workforce by promoting the unique advantages of practice in rural communities and by offering financial and educational incentives.
AAG/Health can help you address your facility’s CRNA needs by helping you tap into the right talent and retaining them in the long run.
We understand rural healthcare organizations' unique needs, strengths, and complexities. Our experts can help you hire professionals who can help you improve customer experience and serve your communities better.
FAQs
Is there a shortage of CRNAs?
Yes, there is a notable shortage of Certified Registered Nurse Anesthetists (CRNAs), particularly in rural healthcare settings.
Projections indicate that by 2033, the anesthesiology workforce may experience a shortage of approximately 12,500 providers. This shortage is anticipated to impact rural communities the most, where CRNAs are often the main or only anesthesia providers.
What is the biggest issue facing the CRNA profession?
The biggest issue is the growing demand for anesthesia services combined with workforce shortages, which can lead to burnout among CRNAs. CRNAs are often required to work longer hours or cover multiple facilities, especially in rural or underserved areas.
How can rural healthcare organizations address the salary disparity from urban areas?
Rural healthcare organizations can address salary disparities by offering competitive incentives beyond base pay. This includes loan repayment programs, scholarships for continued education, sign-on bonuses, relocation assistance, and comprehensive benefits packages.
Moreover, highlighting the lower cost of living in rural areas can help make the overall compensation more appealing, even if the base salary is lower than in urban settings.
What are loan repayment programs, and how do they help recruit CRNAs to rural areas?
Loan repayment programs are initiatives designed to relieve the student debt burden for healthcare professionals, especially those who commit to working in underserved areas. These programs can be helpful in CRNA recruiting. One example of such a program is the NHSC Rural Community Loan Repayment Program.
It provides substantial loan repayment assistance to clinicians in rural communities (designated Health Professional Shortage Areas).
.jpg)
