Hiring nurses and physicians has always been a challenge, but this year, we're facing something deeper. The shortages are hard to manage, and they're starting to reshape how you deliver patient care. Long hiring cycles, early retirements, and rising turnover are stretching teams thin while pushing labor costs higher.
Behind each delay is a lost shift. Behind each open role is a risk to safety or accreditation. You need real numbers that back urgent decisions, whether it’s adopting better workforce solutions, rethinking pay structures, or exploring new staffing models.
In this article, you’ll get the data to support those choices. You’ll see where the healthcare workforce is headed, how today’s gaps shape the industry, and what leaders like you can do to stay ahead.
Let’s start with the big picture.
Key Healthcare Staffing Statistics
These are some of the most important data points shaping the conversation around staffing today. Each one reflects larger shifts in hiring patterns, workforce availability, and financial pressure across U.S. healthcare systems:
- According to the 2025 NSI National Health Care Retention & RN Staffing Report, the average hospital RN turnover rate was about 16.4% in 2024.
- The NCSBN reported that over 138,000 nurses exited the workforce since 2022, and nearly 40% intend to leave by 2029.
- The registered nurse workforce is projected to reach 4.56 million by 2035.
- The State of the U.S. Health Care Workforce projects a shortage of over 187,000 full-time equivalent physicians by 2037.
- As of June 2025, the St. Louis Fed reported total healthcare employment at 18.150 million, up from 18.047 million in April 2025.
- In 2024, U.S. hospitals spent roughly $1.7 billion on travel nurses.
- Travel nurse revenue declined by 37% in 2024.
Healthcare Market Staffing Size
The healthcare staffing market continues to expand across segments, reflecting long-term demand for specialized clinicians and short-term gap coverage. These are the most recent and relevant market size projections and investment patterns that help define where the industry stands today and where it’s heading next:
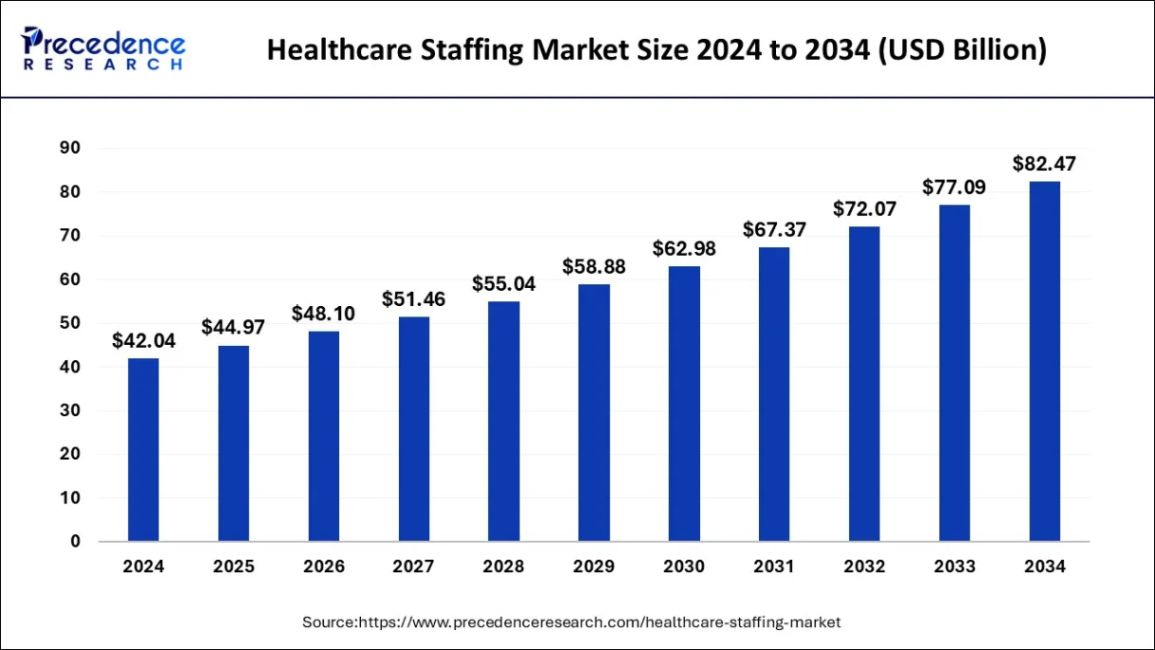
8. According to Precedence Research, global healthcare staffing is expected to reach $44.97 billion by the end of 2025.
As the market is projected to scale to $82.47 billion by 2034, global competition for clinical talent will continue rising.
U.S. systems are contending with domestic rivals and competing with international employers for the same travel nurses, technologists, and advanced practitioners. That shift puts pressure on leaders to build stronger retention plans and faster recruiting funnels.
9. Coherent Market Insights reported that the U.S. healthcare staffing market will hit $22.81 billion in 2025.
This growth includes a mix of travel roles, allied contracts, and permanent placement services. Even modest increases in contract labor spend can impact operating margins over time. That’s why you should assess whether your outsourced roles are being used strategically or simply filling cracks left by stalled internal recruitment services.
10. The travel nursing market is expected to reach $19.5 billion by the end of 2025.
The size of the travel nurse segment shows how much hospitals now depend on local and travel assignment coverage. But persistent use can signal deeper issues with retention, onboarding delays, or internal float pool gaps. Instead of tapering off post-COVID, these contracts remain essential in many regions.
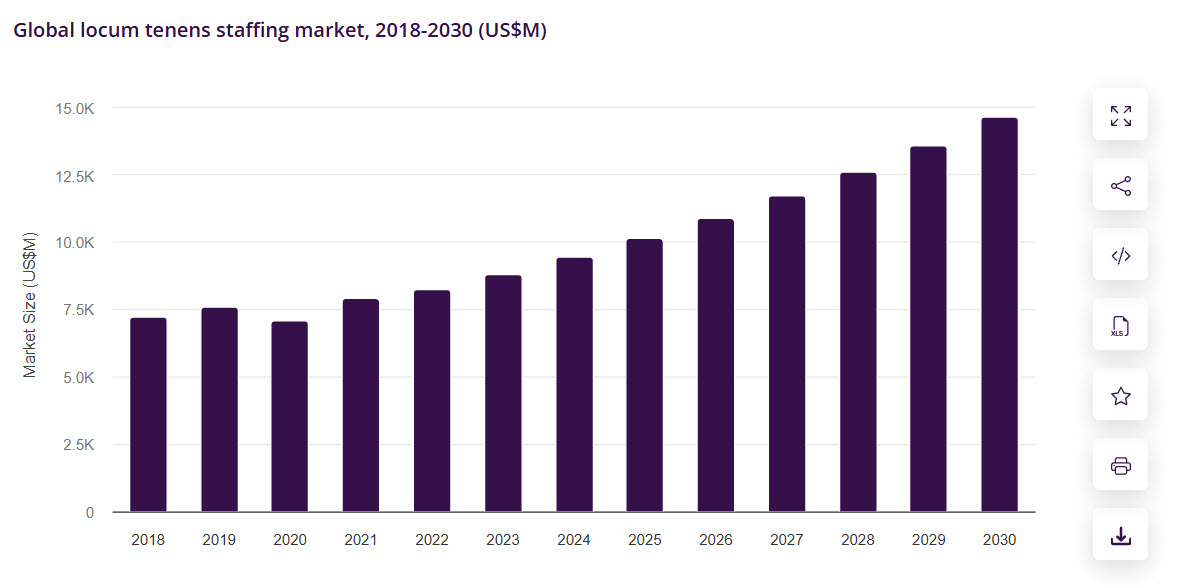
11. According to Horizon Grand View Research, the global locum tenens revenue reached $10,22 billion in 2025.
Locum tenens have become a structural part of the workforce, especially in rural care. They’re filling specialist shortages, covering burnout leaves, and stabilizing short-staffed rotations. For some systems, rotating locums now play the same role that full-time physicians did five years ago.
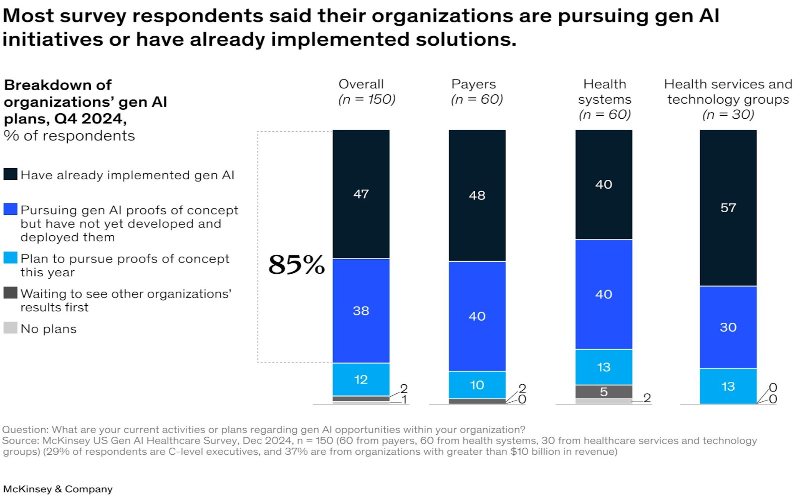
12. McKinsey reported that 85% of healthcare leaders are testing or using generative AI from Q4 2024.
Automation is no longer experimental. Leaders are applying gen AI to accelerate everything from credentialing to nurse staffing forecasts. These tools are shaping how quickly health systems can respond to surge hiring, contract ends, and shifting patient volumes. This makes AI adoption part of any serious talent solution strategy.
Nursing Workforce Statistics in U.S. Healthcare
The U.S. nursing workforce plays a central role in daily care delivery and long-term workforce planning. These are the most recent statistics that define nurse supply, employment trends, and pipeline gaps in 2025:
13. According to NCSBN, the number of licensed RNs in the U.S. reached 5.86 million in 2025.
While there are nearly 5.9 million licensed RNs in the U.S., many aren’t working in active roles. Some have shifted to administrative paths or left clinical work altogether, which makes the license count a misleading proxy for capacity. This complicates talent management decisions that rely on surface-level data.
14. According to NSI Nursing Solutions, 1.9 million healthcare jobs are opening each year.
Annual job openings tied to healthcare roles have reached 1.9 million, covering both newly created positions and turnover backfills. Clinical roles, especially nursing, make up the largest share. Without adaptable healthcare staffing solutions, many facilities risk being locked into a cycle of last-minute coverage and rising contract labor costs.
15. According to the Advisory Board, 87.7% of licensed RNs are actively working as RNs in 2025.
Roughly 12% of licensed RNs aren’t currently practicing, even though they’re qualified to do so. That represents a hidden labor pool that could help fill staffing gaps more quickly than onboarding new grads. Outreach campaigns and flexible roles could help reactivate segments of experienced healthcare talent already in the system.
16. Advisory Board also reported that 70.6% of LPN/LVN licensees are active in the workforce in 2025.
Nearly 30% of licensed LPNs and LVNs aren’t working in active roles today, despite demand in long-term care and home health sectors. For facilities in those settings, reactivating this group may offer faster relief than expanding new pipelines. Solutions could include flexible shifts, returnships, or part-time transitions.
17. U.S. Bureau of Labor Statistics notes that the RN employment is projected to grow 6% through 2033.
RN roles are expected to grow by 6% over the next decade, which will add 194,500 new nurses annually. But those projections assume that open roles can be filled. This is a risky assumption given current pipeline constraints. Without sustained investment in the U.S. job seeker pipeline, growth targets may fall short.
Healthcare Physician Workforce Demographics Trends
Understanding physician and nurse demographics helps you plan not only for coverage gaps but also for diversity, retirement risk, and participation rates. These are the key findings from 2024 and 2025 shaping your strategic decisions on physician access and nursing workforce support.
18. According to HRSA, 933,788 physicians were active, with 800,355 providing direct care in 2024.
133,000 licensed doctors weren’t engaged in patient-facing roles in 2024. They were working instead in administration, research, or non-clinical settings. That makes raw licensure data an unreliable measure for staffing forecasts. Leaders should align workforce planning around actual care delivery capacity to better reflect gaps in healthcare professional availability. As we said above, license counts is a misleading, superficial metric.
19. According to Zippia, 45.8% of all doctors are men, while 54.2% are women.
The shift toward a female-majority physician workforce reflects broader changes in education pipelines and career entry rates. But despite the numbers, disparities in leadership roles and compensation remain. Executives should reassess promotion frameworks and scheduling practices to ensure equity across medical professionals.
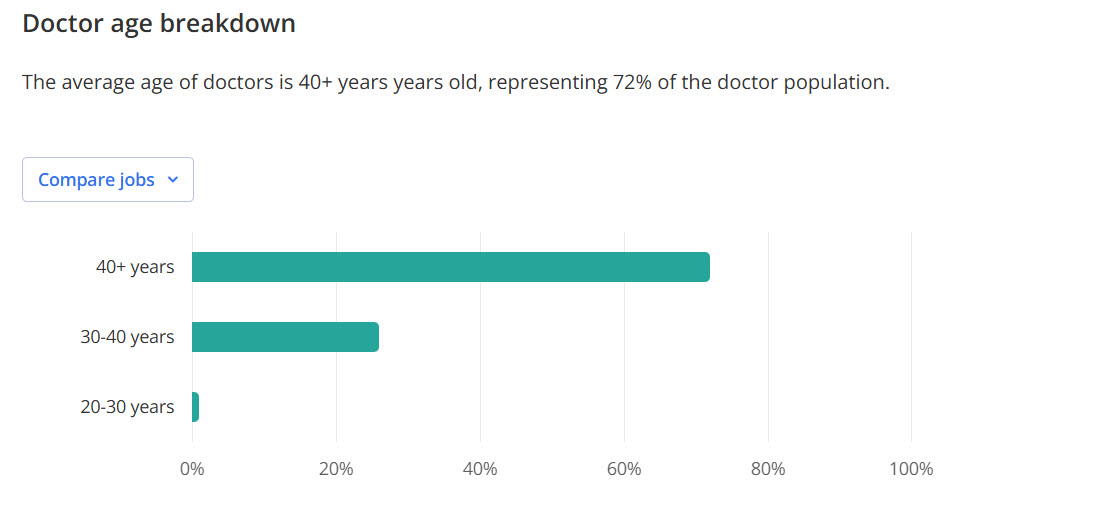
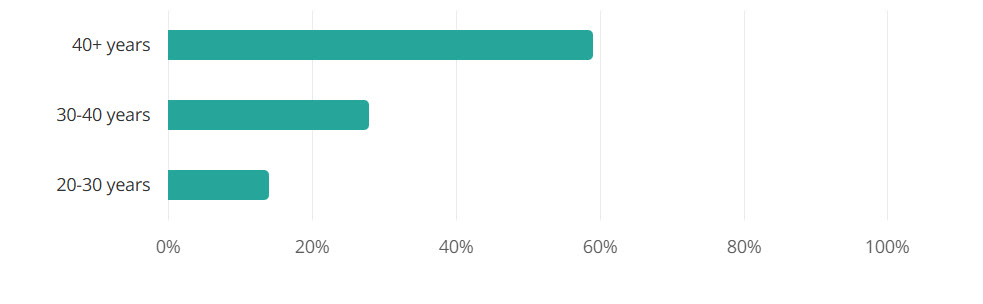
20. Zippia notes that the average doctor's age is 48 years.
With the average age of doctors nearing 50, a wave of retirements is expected over the next two decades. That means experience is aging out faster than new graduates can replace it. Organizations should build internal mentorship programs now to protect continuity and pass on institutional knowledge.
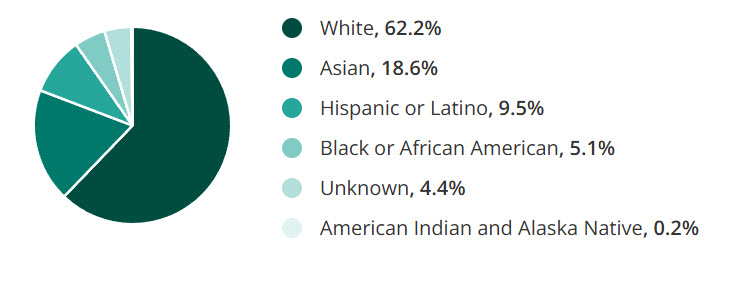
21. Zippia also reports ethnicity breakdown of physicians: 62.2% White, 18.6% Asian, 9.5% Hispanic, 5.1% Black.
Despite years of focus, physician demographics remain skewed, with 62.2% identifying as White and underrepresentation across Black, Hispanic, and other groups. The disparity limits cultural fluency in patient care settings. Long-term change depends on early pipeline expansion through community outreach and targeted scholarships for underrepresented students.
22. Another finding from Zippia is that 13% of all doctors are LGBT.
There are some physicians who identify as LGBT, which adds nuance to how workplace culture and benefits must evolve. HR and compliance teams must ensure protections, inclusive policies, and access to peer support. These shifts aren’t just values-driven but retention strategies as well.
23. A different report from Zippia noted that 86.0% of all U.S. nurses are women, while only 14.0% are men.
Nursing remains heavily gender-imbalanced, with only modest growth in male participation over recent years. That imbalance may affect workforce flexibility, especially in departments or shifts traditionally underserved by gender diversity. Recruiting campaigns could highlight role variety and career mobility to broaden appeal across all care careers.
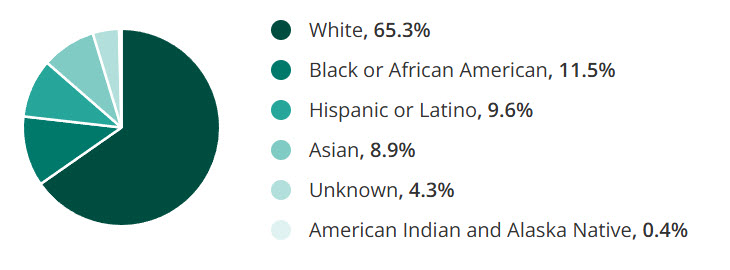
24. Zippia concluded that the ethnic breakdown in nursing is 65.3% White, 11.5% Black, 9.6% Hispanic, and 8.9% Asian.
Workforce diversity among nurses shows only incremental improvement, with 11.5% identifying as Black, 9.6% Hispanic or Latino, and 8.9% Asian. These gaps can translate to lower cultural alignment in patient care, especially in diverse communities. Expanding regional community outreach could help correct the imbalance in pipeline programs.
25. According to Zippia’s nursing report, the average age of a nurse is 43 years old.
The average age of 43 places much of the nursing workforce squarely in mid-career. That timing is critical for succession planning, burnout risk, and upskilling investments. Without strong development tracks, the healthcare staffing industry may lose experienced clinicians before they’re fully utilized in leadership or mentoring roles.
26. The nursing report from Zippia also notes that 9% of all nurses are LGBT.
Workplace policies that recognize LGBT staff needs can affect retention just as much as pay or benefits. This group usually faces higher levels of stress or bias in clinical environments. Creating space for representation and inclusion should be part of building durable healthcare talent ecosystems.
27. According to Axios, immigrants comprise 16% of hospital workers nationwide in 2025.
Immigrant workers play a foundational role in hospital operations, especially in states like California and New York, where they account for up to one-third of staff. This proves the structural role international staffing plays in keeping care delivery stable, especially as domestic hiring pipelines strain to keep up.
Burnout and Job Satisfaction in Healthcare Workers: Statistics and Impact on Well-being
Burnout isn’t just an “individual feelings” issue because it also affects care quality, retention, and organizational stability. These are the most recent statistics that show how widespread stress and dissatisfaction have become among healthcare workers:
28. 43.2% of U.S. physicians report feeling burned out in 2024.
Nearly half of physicians showed signs of burnout, with drivers ranging from EHR fatigue to limited schedule control. These pressures can affect morale but also disrupt continuity in patient care, elevate turnover risk, and contribute to rising locum tenens dependence. Systems need to address workflow design, not just offer wellness webinars.
29. According to a report from Cross Country, 65% of nurses experience high levels of stress and burnout in 2025.
Most nurses surveyed cited unsafe staffing ratios, required overtime, and emotional wear from bedside duties. These issues compound over time and can trigger spikes in absenteeism and early exits. Redesigning unit-level staffing support could reduce daily strain and preserve long-term retention.
30. According to ADA’s Communications Trend Report, around 82% of U.S. dentists reported symptoms of burnout in 2024.
Burnout in dentistry is rising, with contributing factors like solo practice isolation, high student debt, and recruitment gaps for dental assistants. That’s leading to schedule cutbacks and early retirements, especially in smaller practices. Leaders should treat burnout as a business continuity risk to avoid these issues.
31. NCSBN notes that 41.3% of LPNs/LVNs report planning to leave or retire within five years.
The departure of nearly half this workforce tier could decimate coverage in long-term and eldercare settings. These roles usually face stagnant wages and limited advancement tracks, which fuels disillusionment. Addressing career mobility and skill development may slow the exit wave and stabilize staffing in high-need areas.
32. The Doctors Company reports that only 12% of doctors would recommend medicine as a career to others.
A lack of advocacy from within the profession reflects systemic problems, including documentation overload, liability stress, and unclear career growth paths. When even veteran clinicians hesitate to recommend their field, future supply pipelines are at risk. Leaders must rethink how roles are structured, supported, and rewarded over time.
33. 40% of nurses are not sure if they'd choose medicine again.
This signals an erosion of commitment that no amount of short-term incentives can fix. Many nurses cite poor leadership communication, burnout from constant float assignments, and limited voice in care planning. To reverse this trend, systems need to invest in shared governance models and purpose-driven workforce design.
Healthcare Turnover, Retention & Pay
Turnover, retention, and compensation trends reveal where staffing is stabilizing and where pressure continues to build. These are the latest data points shaping your talent planning and workforce strategy:
34. According to NSI Healthcare Solutions, the hospital's overall turnover was 18.3% in 2024, down 2.4 percentage points from 2023.
While the decline from 2023 signals improvement, it still reflects deep workforce instability. For most systems, anything over 15% means constant recruiting, rising onboarding costs, and lost clinical experience. To stay ahead, you’ll need proactive retention initiatives, not just reactive hiring cycles.
35. NSI Healthcare Solutions also reported a RN turnover range by bed size from 5.2% to 36.4%.
This wide range shows that turnover doesn’t hit everyone equally. Smaller or rural facilities usually face higher churn due to limited resources or isolation. Benchmarks must be segmented by size and market to avoid misreading performance across your system.
Pro tip: Some roles are harder to fill than others, and more critical to retain. For example, CRNAs remain in especially high demand. We broke down the CRNA job outlook in a recent article to help organizations plan ahead.
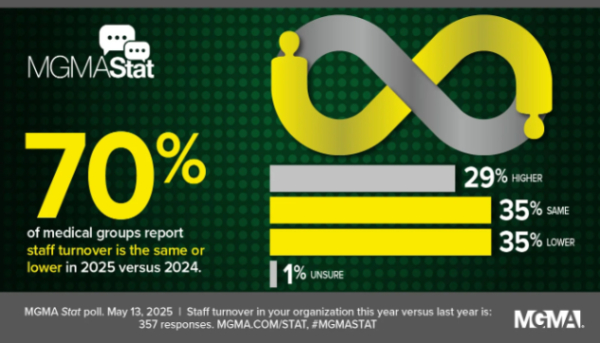
36. According to MGMA, 70% of medical practices reported 35% with turnover same as 2024, 35% saw lower turnover, and 29% experienced increased turnover in 2025.
In 2025, the Medical Group Management Association found mixed results, suggesting retention strategies are working in some organizations but not others. Internal policies, workload models, and incentives may be the differentiators.
37. 46% of healthcare executives plan to leave their organization within 12 months.
Leadership churn at this scale creates planning risk, especially in talent and operational strategy. It also signals possible misalignment between C-suite goals and frontline challenges. If you’re not tracking this trend internally, you may be blindsided by exit waves that stall major initiatives.
38. Turnover rates up to 82% annually among healthcare support staff in skilled nursing facilities.
Support roles are usually the most overlooked, yet they’re foundational to patient flow and safety. When these staff leave, it disrupts everything from ADL delivery to documentation accuracy. Redesigning incentives and recognition at this level is a stabilizing investment.
39. NSI Healthcare Solutions notes that hospitals aim to reduce turnover by 2.6%, yet 25.1% still haven’t set a clear target in 2025.
Without a clear benchmark, it’s hard to secure funding, measure ROI, or motivate cross-functional action. A vague goal invites vague execution. Even a basic 12-month retention KPI can drive alignment across HR, finance, and operations.
40. The cost per RN turnover averages $61,110, according to NSI Healthcare Solutions.
This figure includes training, onboarding, and lost revenue from unfilled shifts. Multiply that by even modest turnover, and the annual cost balloons quickly. Budgeting for retention incentives may be more cost-effective than constant backfilling.
41. NSI Healthcare Solutions has also reported that the vacancy rate for RN positions hovers around 9.6% in 2024.
At nearly 1 in 10 roles sitting open, hospitals are struggling to maintain care ratios and service lines. Vacancy also drives up overtime costs and burnout risk among current staff. You can’t fill gaps at scale without rethinking recruitment velocity and internal mobility.
42. According to NSI Healthcare Solutions, the time-to-hire average is 83 days to fill an experienced RN role.
That’s nearly three months of schedule shuffling, traveler spend, or staff overload. Delays at this stage usually reflect broken intake processes or poor handoffs between TA and clinical leaders. Mapping friction points in your hiring funnel could recover weeks of lead time.
43. The average annual salary for a registered nurse is $94,480 in 2025.
Pay remains a top factor in both retention and recruiting, but salary alone won’t guarantee loyalty. Nurses also want input, growth paths, and better scheduling tools. Raising wages without fixing those factors may lead to higher costs but no stronger retention.
44. Fully licensed doctors in the U.S. earn an average annual salary of $363,000.
For doctors, compensation remains strong, yet rising administrative burden is eroding job satisfaction. That disconnect is why retention can't rely on pay alone. Reducing friction in their day-to-day workflow (through tech or staffing support) will carry more long-term weight.
45. According to the U.S. Bureau of Labor Statistics, nurse anesthetists earn $223,210, nurse practitioners earn $129,210, and nurse midwives earn $128,790 annually.
These roles are growing fast and filling critical care gaps. As they take on more autonomy, demand is surging, especially for NPs and CRNAs. Systems that want to scale must adjust scope-of-practice frameworks, salary bands, and support teams accordingly.
Staffing Impact on Patient Outcomes in U.S. Healthcare
Understaffing undermines both care delivery and organizational credibility. The data points below show how staffing pressures directly affect patients and trust in leaders. The first nine statistics come from the 2025 State of Massachusetts Nursing Survey:
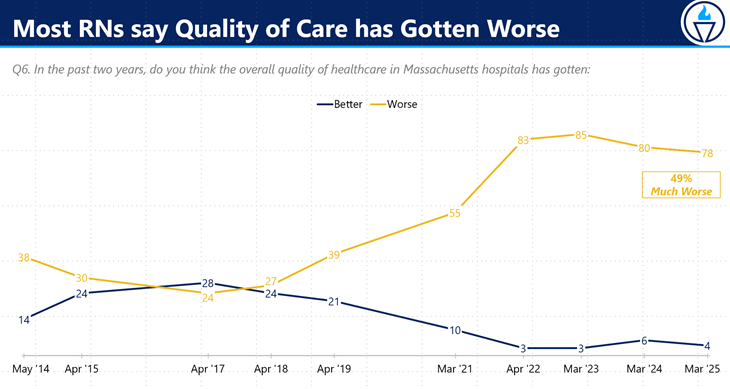
46. 78% of nurses say hospital care quality has declined in the past two years due to ongoing understaffing.
When more than three-quarters of nurses signal a drop in care quality, it's a red flag for safety metrics and accreditation exposure. This perception can drive down patient satisfaction scores and hurt reimbursement. As a leader, you’ll need targeted staffing investments to reverse the trend.
47. 67% of nurses say they lack the time to give patients the care and attention they need.
Two-thirds of bedside nurses say they can't provide essential care and empathy. That gap directly affects outcomes, especially for vulnerable patients. Prioritizing workload balance through staffing ratio adjustments can restore both quality and clinician morale.
48. 49% of nurses worry weekly that unsafe staffing could put their license at risk.
Half of your clinical workforce is worried about liability due to insufficient coverage. That anxiety can contribute to higher error rates and turnover risk. Addressing it is a compliance and retention imperative.
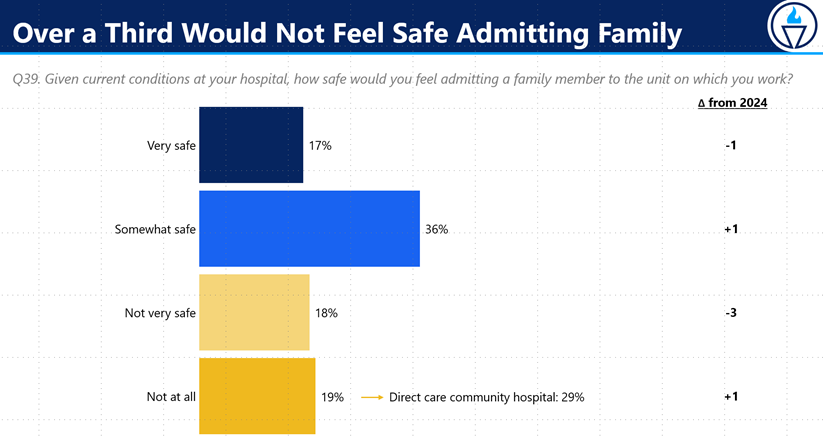
49. 37% of RNs wouldn’t feel safe admitting a loved one to their own unit.
More than one-third of nurses lack confidence in tolerating current patient loads. This is an internal trust gap leaders can’t ignore. It reflects systemic issues that patient surveys may miss.
These can include staffing ratios that consistently leave RNs overextended, workflow inefficiencies that add non-clinical burdens (e.g., excessive charting, admin tasks), or cultural norms where raising safety concerns is discouraged.
Some clinicians may also feel uneasy due to perceived gaps in competency among newer staff: whether from accelerated training programs, staffing shortages, or broader shifts in medical education standards. While efforts to diversify the healthcare workforce can have their merits, they must be paired with strong clinical training to maintain trust across teams. Timely staffing adjustments must be prioritized to close that gap.
50. 83% of RNs have seen patients miss out on needed comfort or help due to short staffing.
Around four out of five nurses report seeing patients go without comforts or vital help. These can accumulate into prolonged recovery times and safety risks. Systems that track these near-misses can better justify nurse staffing expansions.
51. 76% of nurses report not having time to educate patients or plan proper discharges.
Most nurses lack the time to prepare patients and families for safe discharges. That directly increases readmission risk and impacts value-based care results. Embedding discharge coordinators and redistributing tasks can free critical care time.
52. 26% of RNs say they’ve witnessed patient deaths linked to unsafe staffing levels.
Nurses reported direct observation of staffing-related mortality. That very high number represents real clinical impact. Leaders must treat this as a sentinel event and review unit-level staffing patterns immediately.
53. 77% of nurses say Beacon Hill lawmakers aren’t listening to their concerns about unsafe staffing.
Over three-quarters of nurses feel ignored by policy leadership on staffing. That sentiment erodes engagement and may fuel future strikes or turnover waves. Engaging with local policymakers or alliances can realign public perception and workforce trust.
Pro tip: Feeling unheard isn’t just a system-wide issue. It hits individuals, too. For CRNAs navigating respect gaps in 2025, we put together a guide on earning the recognition your role deserves.
54. 63% say hospital leaders ignore staffing feedback; 49% say unsafe assignments are rarely fixed.
Nearly two-thirds of staff believe their concerns go unheard, and half say unsafe posts aren’t resolved. Ignoring clinician input creates engagement and safety risks. Implementing a structured feedback loop could rapidly reduce risk and restore trust.
55. According to a 2025 report from Hallmark Healthcare Workforce Technology, 89% of healthcare leaders feel pressured to cut staffing expenses.
Almost nine in ten executives report cost pressure around staffing. That tension forces tradeoffs between labor budgets and care quality. You’ll need data to clearly justify staffing changes and push back against blanket cutbacks.
Healthcare Staffing Shortage Statistics & Trends
Understaffing isn’t a distant future possibility. It’s happening as we speak across multiple roles and geographies. These figures below will help you plan future capacity, assess budget impact, and prioritize where to build pipelines or tactical support. The first seven statistics from this list below are from the HRSA Health Workforce:
56. A 10% shortage of registered nurses (RNs) is projected for 2027.
Shortages of this scale mean frequent forced overtime, mandatory float, and chronic coverage gaps. Without investing in accelerated training and retention programs, hospitals risk eroding care standards. Localized partnerships with schools and reinstated retirement pipelines may help bridge near-term gaps.
57. By 2037, the RN shortage is expected to reach 6%, or 207,980 full-time equivalent positions.
That backlog accounts for both rising demand and limited inflow from nursing programs. It means your delivery networks must plan workforce capacity at the system level, not just per hospital. Building nurse educator tracks and revising retention incentives becomes essential.
58. In 2027, nonmetro areas may face a 24% RN shortage, compared to just 7% in metro areas.
Recruiting rural CRNAs faces four times the shortage rate of metro markets, largely due to a lack of incentives and educational access. That creates a two-tier landscape in care equity and makes support staffing patchy. Offset this by offering rural stipends or developing pipeline programs tied to local care career pathways.
59. By 2032, RN shortages are projected at 19% in nonmetro areas and 6% in metro areas.
Seven years later, the gap remains staggering, with urban areas better off and nonmetros showing limited gains. Systems expanding rural access must assign resources based on these diverging trajectories. Workforce planning must vary by market, not presume uniform shortage rates.
60. In 2037, nonmetro RN shortages are expected to be 13%, while metro areas face a 5% gap.
By 2037, rural care access may lag significantly, while metro areas stabilize slowly. Addressing that risk will require long-term investments in rural attractants such as housing, education access, and growth tracks. Treat this as a system-wide equity issue, not just a local staffing challenge.
61. The U.S. is projected to face a shortage of 302,440 full-time LPNs by 2037.
Licensed nursing assistants and LPNs are under intense pressure, especially in long-term and post-acute settings. With that deficit looming, turnover control and accelerated LPN programs should be top of mind. Simulation-based training partnerships could help compress onboarding timelines.
62. In 2037, the LPN supply is expected to meet only 64% of demand, down from 80% in 2027.
This downward shift from 80% in 2027 highlights deep pipeline erosion. Expectations for LPN-based workforce models may need fundamental reassessment. Health systems should consider cross-training or rebalancing skill mixes to maintain capacity.
63. According to AAMC in 2024, the U.S. is projected to be short 86,000 physicians by 2036.
This gap suggests long wait times, overloaded primary care access, and care rationing. For systems expanding access, alternative care models (telehealth, APP-tier care) must be considered. It's important to enhance clinician productivity through smarter scheduling technology.
64. The State of the U.S. Health Care Workforce reports that the U.S. is projected to face a shortage of about 187,000 full-time physicians by 2037.
That model aligns with AAMC findings but adds depth on specialty and geography splits. The shortage of physicians signals the need for state and system-level capacity planning early. As a healthcare leader, you should consider training site expansion or loan repayment partnerships to shore up coverage pipelines.
65. The U.S. faces a shortage of over 500,000 RNs in 2025.
Even with large licensure volumes, the U.S. is still over 500,000 nurses short in 2025. Retirements and limited nursing school output are straining bedside teams across most acute and post-acute settings. That gap forces executives to prioritize retention alongside direct hire strategies just to maintain baseline coverage.
66. There’s an anticipated shortage of 73,000 nurse assistants (NAs) by 2028, according to Mercer.
Loss of support roles can cause task shifting to nurses, which raises error risk and burnout. This downstream impact threatens multiple levels of care delivery. Supportive delegation models and skill-mix redesigns should be prioritized.
67. By 2028, Mercer/AHA projects a shortage of 100,000 critical healthcare workers (excluding RNs).
That broader shortage includes respiratory therapists, radiology techs, and other key roles. It means gaps beyond clinical care will affect throughput, diagnostic speed, and discharge readiness. Workforce plans should be comprehensive, not just nurse and physician-centric.
68. Mercer also reports that by 2028, some states (e.g., NY, NJ) will face acute RN shortages, while others may experience slight surpluses.
Some markets will overshoot while others lag behind. State-level tactics like redistribution, license portability, or interstate compacts might help mitigate imbalances. Systems with multi-state footprints should take advantage of this to rebalance assets.
69. Another report by Mercer notes that up to 3.2 million healthcare workers are projected to be missing by 2026.
This forecast highlights systemic labor weakness. It should push organizations toward integrated workforce forecasting, internal pipelines, and flexible staffing models. Treat this as a sector-level warning.
70. According to a report from HRSA Health Workforce, the U.S. is expected to face shortages of 113,930 addiction counselors, 87,840 mental health counselors, 79,160 psychologists, 50,440 psychiatrists, 34,170 marriage and family therapists, and 39,710 school counselors by 2037.
The forecast shows looming gaps of psychiatrists, addiction counselors, and psychologists. As behavioral health demand climbs, under-resourced programs could become further stressed. Expanding training support and credential paths is no longer elective but an operational necessity.
Recent Developments in Healthcare Staffing
Healthcare staffing continues to shift rapidly, shaped by market activity, clinician preferences, and emerging pay models. These recent statistics reflect changing conditions and signal where leaders may need to adapt hiring strategies or operational approaches:
71. MNRSA reports that despite a slowdown from 2022 levels, staffing M&A remained strong, with Q1 2025 activity up 25% compared to Q1 2024.
The uptick in M&A suggests staffing firms are consolidating to gain scale, expand digital capabilities, or diversify into new clinical segments. This could lead to more powerful vendor partnerships or fewer competitive bids. Health systems may need to revisit procurement strategies to retain bargaining power.
72. The 2025 U.S. Healthcare Staffing Report shows job listings are up 48% since 2019
Open roles are piling up faster than most teams can fill them. This level of demand stretches recruiters thin and exposes gaps in scheduling and shift coverage. Now’s the time to invest in tools that speed up screening and shorten time-to-offer.
73. The same staffing report notes that 67% of clinicians exploring new job options say they would choose a temporary role over a permanent one.
Clinician loyalty looks different now. Many want flexibility over long-term commitments, especially after years of burnout. Facilities that don’t adapt their workforce models could lose talent to staffing firms that do.
74. According to the same staffing report, 61% of clinicians would pick an agency that offers same-day pay, and 67% of recruiters say this improves hiring and retention
Getting paid faster has scaled from perk-level to being a part of the decision-making process for a growing share of clinicians. For recruiters, it’s also proving to be a practical lever to speed up placements. Payroll modernization could quickly turn into a competitive edge.
75. According to the American Hospital Association, Providence’s virtual nurse model led to a 40% drop in turnover, near-zero ancillary staff vacancies, and an expected $500,000 in annual cost avoidance after 16 weeks.
Virtual nursing is starting to prove its value beyond pilot phases. It reduces pressure on bedside staff while also closing key gaps in documentation and patient monitoring. For systems facing chronic shortages, hybrid staffing models like this could offer real relief.
Global Healthcare Workforce Outlook (for perspective)
Staffing challenges aren’t limited to the U.S. These next few global figures put local shortages into broader context and show how workforce gaps ripple across health systems worldwide:
76. The WHO projects a global shortage of 11 million health workers by 2030, mainly in low- and lower-middle-income countries.
The uneven distribution of medical professionals around the world adds pressure on high-income countries to maintain self-sufficiency. Overreliance on international recruitment may ease short-term gaps but creates longer-term ethical and supply concerns. Health systems need more homegrown workforce pipelines to stay resilient.
78. The WHO also estimates that by 2030, there will be a shortage of 4.5 million nurses and 310,000 midwives worldwide.
A lack of core providers (like nurses and midwives) disrupts access to foundational care, especially maternal and community health. Countries competing for these roles must offer more than pay to stand out. That includes safer staffing ratios, better training, and long-term career mobility.
79. Around 78% of the world’s nurses work in countries that make up only 49% of the global population in 2025.
This mismatch between workforce location and population needs is a ticking clock for underserved regions. For U.S. leaders, it reinforces the importance of aligning recruitment strategies with real service demand by region. National averages hide serious access disparities that require localized planning.
80. According to McKinsey, in 2025, addressing the global healthcare worker shortage could prevent 189 million years of life lost and add $1.1 trillion to the global economy.
While this is a workforce issue, it’s also a public health and economic one. When staffing gaps grow, so do preventable deaths and missed growth opportunities. Investing in healthcare training and retention isn’t just ethical but also financially sound.
81. Over 80% of healthcare executives anticipate external workforce challenges in 2025, including hiring struggles and talent shortages.
Most leaders are already anticipating external disruptions, whether in hiring timelines, contract labor availability, or credentialing delays. That puts internal planning in the spotlight. Teams that act early on forecasting and staffing models will be better equipped to weather what’s ahead.
Strategic Staffing Starts With Better Partners
You’re managing rising turnover, talent shortages, and care delivery targets all at once. That’s why you need staffing partners who go beyond resumes and placements. AAG Health helps you close critical workforce gaps with full-service recruiting, RPO, and executive search built for healthcare.
We’ve staffed roles from travel nurses to pediatric specialists, and we back it with consulting that improves time-to-fill, retention, and system-wide productivity. The impact is faster hiring, fewer vacancies, and better care continuity.
If you’re ready to rethink how you recruit, place, and retain clinical staff, AAG Health offers the structure and support to make it happen. Contact us today so we can discuss your situation further.

