Radiologists are more than the people behind the scans. They’re medical doctors who help diagnose and treat disease using advanced imaging technology, which is why they’re so important in modern medicine.
From catching early-stage cancer to guiding a biopsy needle with millimeter precision, their work is critical at nearly every stage of care.
Just in the U.S., there are over 31,000 practicing radiologists earning an average of $353,960 annually, and that number is growing.
Radiology is not a monolithic discipline, though. It’s a field that’s become increasingly specialized, with physicians focusing on everything from pediatric imaging to brain and spinal disorders.
After all, imaging needs aren’t the same across age groups, organs, or health conditions. And that level of precision matters, especially when patient outcomes are on the line.
Next, we’ll break down the different types of radiologists, what they actually do, and why it makes a difference for patient care.
Let’s take a look.
Pro Tip: Understanding subspecialties is only part of the equation. Our radiologist recruiting services can help you build a team ready for the future, with the right mix of expertise across diagnostic and interventional care.
TL;DR
If you are short of time, here’s a quick breakdown:
- Diagnostic radiologists interpret medical images like X-rays, CTs, MRIs, and ultrasounds to identify conditions and support treatment decisions.
- Interventional radiologists use imaging to guide minimally invasive procedures that often replace traditional surgery.
- Subspecialties go deep, covering neuroradiology, pediatric radiology, breast imaging, musculoskeletal, cardiothoracic, emergency, nuclear medicine, head and neck, genitourinary, gastrointestinal, and bone densitometry.
- Specialized training means more accurate reads, faster decision-making in urgent situations, safer procedures, and treatment plans that fit each patient’s needs.
- This diversity in roles improves patient outcomes, from catching diseases earlier to enabling quicker recoveries after procedures.
What Are the Different Types of Radiologists?
“Radiologist” is a broad term, but it doesn’t mean just one job. At the highest level, radiologists fall into two categories: diagnostic and interventional. Each plays a distinct role in patient care.
Diagnostic radiologists focus on interpreting medical images to identify abnormalities, guide diagnoses, and support treatment planning.
They work closely with referring physicians, helping to confirm what’s going on inside the body, often before symptoms even appear.
Interventional radiologists, on the other hand, are procedural. They don’t just read images; they use them to guide minimally invasive treatments, replacing the need for traditional open surgeries in many cases.
But here’s where it gets more specialized.
Within these two main branches, radiologists complete subspecialty training (fellowships) in specific areas, like brain imaging, pediatric conditions, or cardiovascular systems.
These subspecialists bring a deeper level of expertise, which is crucial when you’re seeking fast, accurate readings and informed decisions.
And the trend is clear: Radiologists are becoming increasingly multi-specialty. An industry report found that 55% of radiologists read across three or more subspecialties, and 85% cover at least two.
Don’t view this evolution as purely academic. In our experience, it reflects growing demand and complexity in imaging, as well as a nationwide shortage of trained specialists in the U.S.
What Does a Diagnostic Radiologist Do?
Diagnostic radiologists identify what’s going wrong in the body, usually before a surgeon, oncologist, or cardiologist steps in.
Their job is to translate raw data (such as X-rays, MRIs, CT scans, and ultrasounds) into actionable insights.
They work across many imaging modalities, including:
- X-rays: Great for spotting fractures, infections, or lung conditions.
- Computed Tomography (CT): Offers detailed cross-sectional views of organs and bones.
- Magnetic Resonance Imaging (MRI): Provides high-resolution images of soft tissue, brain, and spinal structures.
- Diagnostic ultrasound: Commonly used in prenatal care, as well as liver, thyroid, and vascular exams.
Some diagnostic radiologists practice as generalists, working across multiple body systems. Others pursue additional fellowship training to specialize in areas such as abdominal imaging or musculoskeletal scans.
These subspecialists are consulted for complex cases that require greater nuance. Their work is highly collaborative, as they provide detailed findings to the referring physician, who then uses that input to build a care plan.
In fast-moving environments like ERs or stroke units, their speed and accuracy can be the difference between life and death.
And they’re busy. The average radiologist will interpret over 100 imaging studies per day, under high cognitive load and with little margin for error.
Yet despite that pressure, their work remains largely behind the scenes, quietly critical to nearly every clinical decision made.
What Is Interventional Radiology?
Interventional radiology (IR) blends imaging expertise with hands-on treatment.
These radiologists interpret scans, yes, but they also use imaging in real time to guide minimally invasive procedures that can replace traditional surgery.
Using technologies like CT, MRI, fluoroscopy, or ultrasound, they can precisely target areas of the body with tiny instruments and catheters. These procedures don’t require large incisions and, in many cases, no overnight hospital stay.
Here are some of the most common IR procedures:
- Biopsies: Taking tissue samples guided by imaging.
- Stent placement: Opening narrowed arteries to improve blood flow.
- Tumor ablation: Destroying cancer cells with heat, cold, or chemicals.
- Uterine fibroid embolization: Shrinking fibroids by cutting off their blood supply.
- Drainage and catheter placements: For infections, abscesses, or fluid build-up.
Why does this matter? Well, these procedures have faster recovery times, fewer complications, and lower costs than surgery, according to numerous reports.
Interventional radiology also has one of the highest average salaries, about $523,000, as Radiology Business reported.
Our recent analysis of radiologist salaries in 2025 confirms this pattern, placing interventional radiology among the top-paying subspecialties in the field.
Despite this, reimbursement trends aren’t encouraging. The 2025 Medicare conversion factor is set to drop -4.83% for interventional radiology, putting pressure on practices to do more with less, as The Imaging Wire reported.
IR is growing, in demand, and central to the future of procedural medicine. But it needs strategic support to keep pace with demand.
What Are the Main Radiology Subspecialties?
Radiologists usually complete fellowship training in a subspecialty after their residency. These areas of focus help them develop deeper knowledge in specific systems or patient groups.
Here's a breakdown of the major subspecialties you’ll find in practice today:

Neuroradiology
The nervous system is one of the most complex areas of the body, and imaging it requires sharp expertise.
Neuroradiologists handle high-stakes cases like stroke, trauma, and tumors affecting the brain and spine.
Here’s what defines their work:
- Focuses on the brain, spine, head, and neck.
- Common scans include MRI for stroke, multiple sclerosis, tumors, and trauma.
- Also handles neuro-interventional procedures like aneurysm coiling.
Pediatric Radiology
Children aren't just small adults. Their anatomy, diseases, and tolerance for radiation all require tailored approaches, which is where pediatric radiologists step in.
This subspecialty covers:
- Medical imaging for children.
- Adjusts for different anatomy and developmental stages.
- Lower radiation exposure with pediatric protocols.
Of course, pediatric radiology can have different subspecialties as well, targeting different body parts.
Breast Imaging
This subspecialty is at the front lines of early breast cancer detection. It combines technology with deep pattern recognition to flag issues as early as possible.
The role of a breast imaging radiologist includes:
- Screening and diagnosis of breast conditions.
- Use of digital mammography, breast ultrasound, and breast MRI.
- Early detection and treatment planning.
Musculoskeletal Radiology
When it comes to movement, pain, or trauma, musculoskeletal radiologists are key.
They work closely with orthopedists, sports doctors, and rheumatologists to pinpoint what’s going on inside the joints, bones, or muscles.
Their scope of work includes:
- Focus on bones, joints, muscles, and soft tissues.
- Interpretation of MRIs, CTs, and X-rays for injuries and abnormalities.
- Common in sports medicine, arthritis, and oncology.
Cardiothoracic Radiology
This is the primary specialty for imaging of the heart and lungs, critical in cardiology, oncology, and emergency settings. But as imaging volumes rise, so does the need for better training.
Their specialty involves:
- Focus on the heart, lungs, and chest structures.
- Diagnosing coronary artery disease, pulmonary embolism, and lung cancer.
- Supporting interventional procedures like stenting and clot removal.
Key insight: 41% of radiologists report low confidence in cardiac imaging, as Radiology Business stated, despite increasing demand.
This lack of confidence isn’t surprising. Cardiac and thoracic imaging are among the most technically challenging areas in radiology: the heart and lungs are always in motion, chest structures overlap, and new imaging technologies keep appearing (and improving).
That makes finding well-trained specialists even more critical. And it’s also more difficult for hospitals facing staffing gaps.
Alpha Apex Group Health closes that gap.
We place cardiothoracic radiologists faster than the industry average, completing searches in 55–90 days instead of 120+. With an 80% success rate on exclusive searches, 400+ candidate inquiries daily, and a 90-day replacement guarantee, we help hospitals secure specialists in one of the most complex fields of medicine.
Head and Neck Radiology
This subspecialty focuses on complex conditions in the face, neck, and throat, areas where subtle findings can be critical for treatment planning.
Key aspects include:
- Imaging of sinuses, thyroid, salivary glands, and airway structures.
- Identifying cancers, infections, and congenital anomalies.
- Supporting surgical planning for ENT and oncology teams.
Genitourinary Radiology
Genitourinary radiologists specialize in the kidneys, bladder, prostate, and reproductive organs, where imaging guides both diagnosis and treatment.
Their role covers:
- Ultrasound, CT, and MRI for urinary tract and reproductive health.
- Detecting kidney stones, tumors, and congenital anomalies.
- Supporting prostate cancer detection and treatment decisions.
Gastrointestinal Radiology
The GI tract poses unique challenges, from subtle bleeding to complex tumors. Gastrointestinal radiologists bring expertise in imaging this system.
They focus on:
- Stomach, intestines, liver, pancreas, and biliary tract imaging
- Diagnosing cancers, inflammatory bowel disease, and liver disorders
- Using CT, MRI, and fluoroscopy for functional and structural insights
Bone Densitometry
Bone health is a major concern in aging populations, and bone densitometry specialists help assess fracture risk.
Their expertise involves:
- Using dual-energy X-ray absorptiometry (DEXA) scans.
- Detecting osteoporosis and monitoring bone density over time.
- Guiding preventive care and treatment decisions for bone health.
Emergency Radiology
Time is everything in emergency care. These radiologists work on the frontline, providing real-time interpretations for trauma, stroke, and acute illness.
Their responsibilities include:
- Work in ERs and trauma units with high-pressure cases.
- Interpret scans for stroke, fractures, hemorrhages, and internal injuries.
- Being available 24/7 for immediate reads.
Nuclear Medicine
When standard scans don’t show enough, nuclear medicine adds a metabolic layer, tracking how tissues behave, not just how they look.
This includes:
- Use of radioactive tracers for detailed organ and tissue imaging.
- Support the diagnosis of cancer, heart disease, and thyroid conditions.
- Use of tools like PET scans and SPECT imaging.
One key thing to note: As the Radiologist Business also reported, 28% of radiologists feel undertrained in this area, but interest in upskilling is high.
How Do Radiologists Train for These Specialties?
Becoming a radiologist involves more than learning to read images. It requires medical expertise, technological proficiency, and strong clinical judgment. The path is long, and for subspecialists, even longer.
Here’s how the typical path looks:
- Undergraduate (4 years): Future radiologists start with a bachelor’s degree, usually in a science-related field such as biology, chemistry, or physics. Coursework in anatomy, physiology, and math lays the foundation for medical school. Many students also volunteer or shadow physicians to gain early clinical exposure.
- Medical school (4 years): Just like any physician, future radiologists start with a general medical education after they pass the Medical College Admission Test® (MCAT®).
- Internship (1 year): After graduating from medical school, new doctors complete a one-year internship. This can be a transitional year (broad clinical exposure) or a preliminary year in a specific field such as medicine or surgery. The internship builds general clinical skills and prepares them for the more specialized training in diagnostic radiology.
- Residency in radiology (4 years): After med school, they enter a radiology residency, rotating through multiple imaging modalities and clinical settings.
- Fellowship training (1–2 years): Subspecialists then pursue focused training in areas like neuroradiology, breast imaging, or interventional radiology. This deepens their expertise and prepares them for high-complexity cases.
- Board certification: Most radiologists get certified through the American Board of Radiology, with optional subspecialty certifications depending on their focus.
Why Do These Different Types of Radiologists Matter for Patients?
Specialization reflects a deliberate response to the growing complexity of modern healthcare.
As imaging has become more advanced, having the right expert read the right scan has become essential to patient safety and treatment outcomes.
Here’s what subspecialized radiology brings to the table:
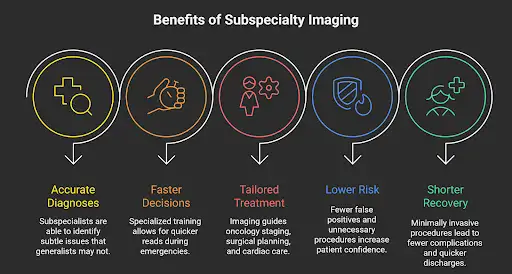
More Accurate Diagnoses
Subspecialists spend years training to recognize patterns specific to their area.
That allows them to detect subtle abnormalities a generalist might overlook, like a tiny brain aneurysm on an MRI or early-stage breast cancer on a mammogram.
In high-stakes cases, that level of precision can be the difference between catching a condition early or missing it altogether. In fact, when breast cancer is diagnosed at its earliest, localized stage, the 5-year survival rate reaches a remarkable 99%.
Faster Decisions
In emergency settings like trauma units or stroke response teams, time is critical.
Subspecialists combine greater expertise in the relevant imaging with training to make accurate interpretations in high-pressure settings.
That speeds up decision-making, which is especially important when treatment windows are measured in minutes.
Customized Treatment Plans
Radiologists serve a dual function: diagnosing disease and guiding the course of care. Subspecialists provide insights that help other physicians choose the best next steps.
In oncology, for example, the imaging can determine tumor staging, surgical planning, or eligibility for a targeted therapy. In cardiology, a precise scan read might mean avoiding unnecessary catheterization.
Lower risk
Subspecialized reads help reduce false positives and negatives, which means fewer unnecessary procedures and a lower chance of missing something critical.
For patients, that translates to less stress, fewer follow-ups, and more confidence in their care path.
Shorter recovery times
In interventional radiology, the combination of image-guided precision and minimally invasive techniques leads to fewer complications, less downtime, and faster discharges.
Patients can often go home the same day, without the longer recovery associated with open surgery.
It’s important to remember that the radiologist interpreting a scan can directly influence the diagnosis, the treatment plan, and the recovery timeline. Greater specialization increases the likelihood of optimal outcomes.
Current Landscape and Emerging Challenges in Radiology
According to workforce studies, the number of radiologists is expected to grow by 25.7% between 2023 and 2055, reaching around 47,119 radiologists.
But there’s a catch: that projection assumes no growth in training programs, which means demand may still outpace supply.
In fact, many healthcare systems are already experiencing a shortage of radiologists, with staffing levels struggling to keep up with rising imaging volumes.
As Dr. Eric Christensen of the Neiman Institute stated:
“The present radiologist shortage is projected to persist unless steps are taken to grow the workforce and/or decrease per-person imaging utilization. In other words, the shortage is not projected to get worse, nor will it likely improve in the next three decades without effective action.”
That shortage makes subspecialty access even more valuable (and uneven) depending on location.
Especially in areas like cardiac imaging, nuclear medicine, and pediatrics, expanded fellowship opportunities could help close the gap.
To respond to these pressures, many hospitals are turning to technology as a force multiplier.
Artificial intelligence is beginning to ease the daily workload on radiology teams by highlighting urgent cases and pointing out patterns that might otherwise take longer to detect. This technology is meant to support physicians, helping them work more efficiently and devote more time to complex decisions and patient care.
These advances are not limited to on-site practice. As imaging volumes grow, AI in teleradiology is extending expertise beyond hospital walls, improving access in underserved areas, and helping providers deliver timely, around-the-clock care.
Pro Tip: Speaking of it, staying ahead of teleradiology trends is essential. What once served as a temporary solution is now shaping how imaging will be delivered and scaled in the years ahead.
Bottom Line: Radiology’s Value Is in Its Diversity
Radiology should be understood not as one specialty, but as a network of physicians offering highly specific expertise.
From neuroradiologists interpreting complex brain scans to interventional radiologists performing image-guided procedures, each subspecialty plays a distinct role. Together, they make diagnosis and treatment safer, faster, and more precise.
The numbers make it clear: demand for imaging continues to rise, while the radiologist workforce struggles to keep pace. This gap has consequences that extend far beyond the profession itself.
For patients, it can mean the difference between catching a disease early, avoiding unnecessary surgery, or accessing minimally invasive treatments with faster recovery. For healthcare systems, it translates into greater efficiency, lower costs, and improved outcomes.
At AAG Health, we recognize the role each radiology specialty plays in shaping modern care. If your organization is facing workforce challenges, see how our radiologist recruiting services can connect you with the talent you need to keep delivering high-quality care.
Contact us today to discuss how we can support your recruiting needs.
FAQs
What are the Main Types of Radiologists?
Radiologists are generally divided into two groups. Diagnostic radiologists interpret imaging such as X-rays, CT scans, MRIs, and ultrasounds to detect disease and guide treatment. Interventional radiologists use imaging in real time to perform minimally invasive procedures, often replacing the need for open surgery. Beyond these, radiology includes subspecialties such as neuroradiology, pediatric radiology, breast imaging, musculoskeletal, cardiothoracic, emergency radiology, nuclear medicine, head and neck, genitourinary, gastrointestinal, cardiovascular, and bone densitometry.
What’s the Difference Between a General Radiologist and a Subspecialist?
A general radiologist interprets imaging studies across multiple body systems and is often found in community hospitals or rural settings. A subspecialist, by contrast, completes additional fellowship training in a focused area such as pediatric imaging or cardiovascular radiology. This advanced training enables them to handle complex cases with greater precision—for example, detecting subtle tumor changes on brain scans or evaluating congenital heart disease.
Why are Subspecialized Radiologists Important for Patients?
Subspecialization enhances accuracy and efficiency in care. Radiologists trained in a single field can detect conditions earlier, respond faster in emergencies, and support tailored treatment plans.
Do all Radiologists Read the Same Types of Scans?
Not always. While diagnostic radiologists are trained to interpret a variety of imaging studies, subspecialists focus on complex or high-risk cases in their area. Sometimes radiologists work across different modalities to meet workforce needs.
Are Radiologists also Involved in Treating Patients, or Only Diagnosing?
While diagnostic radiologists primarily interpret scans and advise physicians, interventional radiologists actively perform treatments such as angioplasty, tumor ablation, and uterine fibroid embolization.
What Technologies do Subspecialized Radiologists Commonly Use?
Subspecialized radiologists employ advanced tools, including digital radiography, CT, MRI, ultrasound, PET scans, and digital mammography. Nuclear radiologists often rely on PET imaging and gamma-ray techniques for cancer and metabolic disorders. Interventional radiologists use real-time fluoroscopy or ultrasound during procedures.
Are Radiation Oncologists Considered Radiologists?
No. Radiation oncology is a distinct specialty focused on treating cancer with radiation therapy, using approaches like external beam therapy or brachytherapy. Radiation oncologists often collaborate with radiologists, who provide the diagnostic imaging that guides treatment.

