Artificial intelligence (AI) is making big splashes in healthcare, and radiology is one area where its impact is the most visible. From stroke detection to cancer screening, AI tools are being integrated into imaging workflows across hospitals and research centers.
The pitch is simple: faster diagnoses, fewer errors, and better outcomes. But there’s a harder question underneath it all: if AI can read medical images, will AI replace radiologists?
This debate matters, not just for radiologists, but for the entire healthcare system. Diagnostic imaging is foundational to modern medicine. If AI disrupts this space, it reshapes everything from workforce planning to medical training to patient safety.
This article outlines where AI stands today, how it compares to radiologists in accuracy and reliability, and what it can (and can’t) do within clinical practice.
TL;DR
If you’re short on time, here’s the quick summary:
- AI is already playing a role in radiology, especially in high-volume tasks like flagging abnormalities or prioritizing urgent scans.
- Over 400 AI algorithms for radiology have FDA clearance, with most approved in the last five years.
- In controlled studies, AI can match or exceed radiologists in detection speed for some conditions, but not in complex diagnoses or contextual interpretation.
- AI tools are assistive, not autonomous. They don’t replace radiologists; they support them.
- Legal, ethical, and clinical responsibilities still fall on physicians.
- As AI takes over simpler, high-volume tasks, radiologists may move toward more analytical, procedural, and patient-facing roles.
What Is AI’s Role in Radiology Today?
AI in radiology has moved beyond speculation and is now part of everyday practice.
Right now, AI supports key stages of the imaging workflow, from scan acquisition to final reporting.
Most applications fall under computer-aided detection (CADe) and computer-aided diagnosis (CADx), where algorithms identify and classify anomalies in imaging studies.
These systems use machine learning and deep learning (especially convolutional neural networks (CNNs) to process large volumes of data with high consistency.
Their goal of using AI is to improve speed, reduce human error, and optimize clinical workflow in both radiology and teleradiology.
Real-World Use Cases of AI in Hospitals and Research
AI tools are already embedded in emergency settings. Hospitals use them to detect strokes or lung nodules in CT scans, which helps reduce time to diagnosis.
Academic research is also driving progress. AI is being trained on massive imaging datasets to uncover subtle patterns linked to disease. In cancer screening, especially for breast cancer, early results are promising.
For instance, a Swedish study of 80,000 mammograms showed AI-supported screening detected 20% more cancers compared to double-reading by two radiologists. It also cut the human workload by 44%.
Lead author Dr Kristina Lång from Lund University in Sweden stated that she was surprised by the initial results of the study. This was because they had exceeded the researchers' expectations:
"We found that we could detect more cancers when we screened with the support of AI. But at the same time, it did not increase false positives, and we can reduce the screen reading workload for radiologists by almost half."
Out in the real world, AI has already made it into a wide range of medical devices that are used in healthcare facilities across the country. As of Fall 2025, 1,000 AI-enabled medical devices have FDA clearance, many of which are used in radiology. These numbers show the expanding adoption of AI in medical practice.
How Accurate Is AI Compared to Radiologists?
Performance comparisons between AI and radiologists are nuanced and complex. In specific tasks, such as identifying lung nodules or classifying mammograms, AI can match or surpass human speed and sensitivity. But that advantage also comes with limitations.
Where AI excels
- Speed and scalability: AI can analyze thousands of images rapidly, which is critical for high-volume screenings.
- Pattern recognition: Algorithms trained on annotated data can identify micro-patterns invisible to the human eye.
- Consistency: AI doesn't experience fatigue or distraction, which helps reduce diagnostic variance.
Research backs this up. In a Philips study, radiologists using AI identified lesions 26% faster, and AI flagged 29% of lesions the clinicians had initially missed.
Another study at Union Hospital, affiliated with Tongji Medical College of Huazhong University of Science and Technology (HUST) in China, validated the Janus-Pro-CXR (1B), a chest X-ray interpretation system.
The researchers found that AI assistance significantly improved report quality scores (4.37 vs. 4.11, p < 0.001). It also reduced interpretation time by 18.5%.
Where AI still falls short
- Clinical complexity: AI tools struggle with rare conditions or overlapping pathologies that require integrative reasoning.
- Bias in training data: If the data lacks diversity, AI may underperform in underrepresented populations.
- Lack of context: AI doesn’t incorporate patient history, symptoms, or lab results, factors radiologists routinely weigh.
Importantly, human oversight remains non-negotiable. A study by Harvard Medical School found that while well-trained AI improved diagnostic accuracy, poorly performing tools reduced it.
In other words, AI is only as useful as its implementation and the radiologist overseeing it. It’s safe to say that it’s highly accurate, but not always.
What Can Radiologists Do That AI Can’t?
Despite AI’s technical progress, there are critical areas where it falls short, particularly in responsibilities that extend beyond image analysis.
Radiologists operate within a broader clinical, ethical, and interpersonal context that AI cannot replicate or replace.
Ethical and Legal Accountability
AI tools cannot assume legal responsibility for a diagnostic report. Regulations across healthcare systems mandate that only licensed professionals can issue official interpretations, particularly in high-stakes cases like cancer diagnosis or trauma evaluation.
This isn’t just a formality. When a diagnosis leads to treatment (or impacts a patient’s life expectancy), the physician bears legal and ethical responsibility.
If an AI tool makes an error, the accountability still falls on the human clinician who signed the report. That’s why oversight isn’t optional. Even when AI assists with image triage or detection, final approval must come from a radiologist.
According to a survey published in Insights into Imaging, 45% of healthcare professionals believe radiologists should be solely responsible for AI outputs. Meanwhile, 37% support shared responsibility. This highlights the ongoing debate around accountability in AI-driven healthcare.
.webp)
Communication and Patient Care
Radiologists do more than interpret scans. They explain complex findings to both patients and physicians, often in time-sensitive or emotionally charged situations.
From walking a patient through a cancer diagnosis to advising a surgeon on intraoperative imaging, radiologists bridge clinical data and human decision-making.
Empathy and reassurance are part of the job.
Especially in oncology, pediatrics, or cases involving rare diseases, delivering information clearly and compassionately is necessary. The way results are communicated can greatly influence how patients understand their condition and make treatment decisions.
AI may not have that capacity. It can flag a lesion, but it can’t explain what that means in the context of a patient’s history, or help families process what comes next.
In other words, radiology still depends on human judgment and communication.
Will AI Reduce the Demand for Radiologists?
AI may reduce the demand for radiologists as it takes on the traditional duties like interpreting images and diagnosing diseases, but it won’t make their role obsolete. In fact, in the light of AI tools’ increasing use in radiology, the nature of the role of a radiologist will change.
But let’s get deeper:
Shift in Demand, Not Disappearance
AI automates repetitive, high-volume work, such as identifying normal scans or flagging common pathologies.
That reduces the need for radiologists focused solely on screening, especially amid the broader radiologist shortage, which hospitals are scrambling to address. But it also increases the need for specialists who can supervise AI workflows, validate outputs, and handle complex or ambiguous cases.
Radiologists who adapt are essential and will remain relevant. Clinical strategy, interventional procedures, and advanced diagnostic interpretation can’t be outsourced to algorithms.
In fact, as AI handles more volume, radiologists are freed up to take on higher-value roles in multidisciplinary teams and direct patient care.
Pro Tip: Adopting AI is only part of the equation; hospitals also need the right people. Our radiologist recruiting services can help you build a team ready for the future.
Implications for the Workforce
Job market trends are already shifting. Some training programs are adjusting curricula to include AI literacy, workflow design, and quality control.
According to a survey of Society of Chairs of Academic Radiology Departments members, 100% said they plan to implement AI to improve quality and efficiency. In addition, 95% reported they would use it to reduce clinician burnout.
However, early-career radiologists and trainees are expressing more uncertainty. While most experienced radiologists feel confident integrating AI into practice, only 72% of surveyed trainees shared that optimism.
This highlights the need for formal education in AI systems, not just on how to use them, but how to critically evaluate them.
Workforce shifts also come with financial implications. Our recent analysis of radiologist salaries in 2025 provides insights into budgeting for this evolving role.
What Are the Benefits of AI for Radiology and Patients?
AI’s value in radiology comes from its ability to streamline workflows and support clinicians in ways that directly impact patients.
The strongest case for adoption lies in how these tools optimize clinical workflows while improving diagnostic accuracy and outcomes.
A “hybrid” artificial intelligence strategy (using a combination of radiologist readers and standalone AI interpretation of cases) can cut radiography workloads by nearly 40%.
But let’s see what more benefits this implementation brings:
Faster Prioritization
AI systems can automatically sort imaging studies by urgency. Critical findings (such as suspected stroke, pulmonary embolism, or acute bleeding) are flagged and placed at the top of the queue.
For radiologists in emergency departments, this ensures the most time-sensitive cases are handled first.
In acute care, every minute matters. Rapid prioritization allows clinicians to start life-saving interventions sooner, like thrombolytic therapy for a stroke or surgery for internal bleeding.
Early pilots of AI triage tools in hospitals report measurable reductions in reporting delays, translating directly into better patient outcomes.
However, prioritization systems must be carefully calibrated. Too many false alerts can lead to “alarm fatigue,” which lessens the trust in the technology.
The challenge is balance: fast enough to help, precise enough to be trusted.
Improved Diagnostic Confidence
Radiologists often describe AI as a reliable “second set of eyes.” Algorithms highlight suspicious regions on scans, making subtle abnormalities less likely to be overlooked.
This is particularly valuable in early-stage disease detection, where visual cues can be faint or ambiguous.
AI enhances trust in the final report through its ability to confirm or flag a clinician’s interpretation.
In teaching hospitals, it also acts as a learning tool and shows trainees how experienced radiologists approach scans and why.
Still, confidence must not turn into overreliance. The most effective use is as a supportive cross-check, not a replacement for clinical judgment.
Better Patient Experience
AI not only supports radiologists but also delivers direct benefits to patients.
Faster reporting means less time waiting in uncertainty and earlier treatment decisions. That, in turn, reduces both anxiety and the risk of disease progression.
Equally important, AI frees radiologists from repetitive, high-volume reviews, giving them more time for patient and physician interaction. In fact, AI is also a big trend in teleradiology, which helps address radiologist shortages in remote or underserved regions.
Explaining results, answering questions, and guiding treatment options are areas where the human element remains irreplaceable.
For patients, AI translates into less waiting, more clarity, and care that doesn’t lose its human touch.
What Are the Risks and Challenges of Relying on AI in Radiology?
AI integration brings clear benefits, but it also introduces challenges that healthcare organizations must manage carefully.
These challenges are not hypothetical but have been documented in early adoption studies.
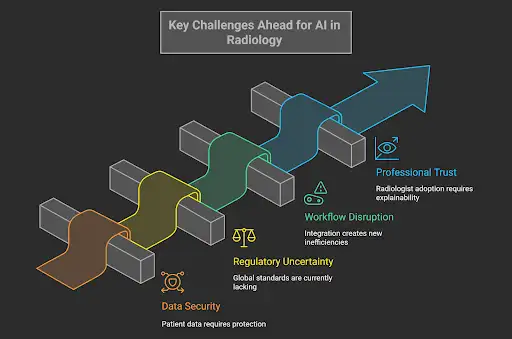
Data Security and Privacy
Medical imaging involves highly sensitive patient data. Training and running AI models require massive datasets, often pooled across hospitals and even countries. This raises concerns about how data is stored, shared, and protected.
A breach in imaging datasets would go beyond technical failure. It could undermine patient trust and expose institutions to legal risk.
Healthcare systems must strike a balance between innovation and strict compliance with privacy frameworks, such as HIPAA in the U.S. or GDPR in Europe.
Regulatory Uncertainty
The use of AI in healthcare is increasing faster than regulations are changing. While nearly 400 radiology tools have FDA clearance, there’s no unified global standard for validation, safety monitoring, or post-market surveillance.
The result is uneven accountability. One algorithm may perform well in a U.S. hospital with oversight but struggle in a smaller, less resourced institution abroad.
Without international alignment, performance can vary widely, leaving patients exposed to inconsistent care.
Workflow Disruption
Implementing AI is not as simple as switching it on. Hospitals must reconfigure their workflows, retrain staff, and integrate new systems with their existing legacy infrastructure.
If implementation is rushed or poorly coordinated, AI can create friction rather than efficiency.
For example, if an AI system generates alerts that aren’t prioritized properly, radiologists may face “alarm fatigue.” They end up spending extra time verifying false positives instead of focusing on urgent cases.
Professional Trust
Clinician confidence is central to adoption. If an algorithm produces outputs without explainability (or worse, inconsistent results), radiologists hesitate to use it in clinical decision-making.
Explainable AI is still in its early stages, but its importance is critical.
Radiologists need transparency about how a model reached its conclusion, not just the conclusion itself. Until then, skepticism will slow adoption.
These challenges don’t negate AI’s value. But they demand careful governance, training, and validation before widespread deployment.
What Does the Future of Radiology Look Like with AI?
The trajectory of radiology points to collaboration rather than replacement. Its future is best seen as a hybrid profession, where radiologists and AI systems work together to improve accuracy, efficiency, and patient outcomes.
Training the Next Generation
Residency programs are beginning to integrate AI literacy into curricula.
Tomorrow’s radiologists won’t just interpret scans. They’ll also evaluate AI outputs, monitor algorithm performance, and understand the limitations of machine learning in clinical practice.
Maintaining diagnostic accuracy and patient safety will depend on this dual expertise.
AI as a Clinical Partner
AI has the potential to serve as a cornerstone of precision medicine in the future.
Through the integration of imaging, genetic, laboratory, and historical data, multimodal AI systems could offer truly personalized insights.
Radiologists, with their clinical expertise, will remain the gatekeepers of how those insights inform patient care.
The Vision and Timeline of AI Adoption
Looking toward the future of radiology, the vision ahead is both exciting and complex.
Interestingly, Matt Covington, MD, put it directly in a conversation with ChatGPT about AI in radiology:
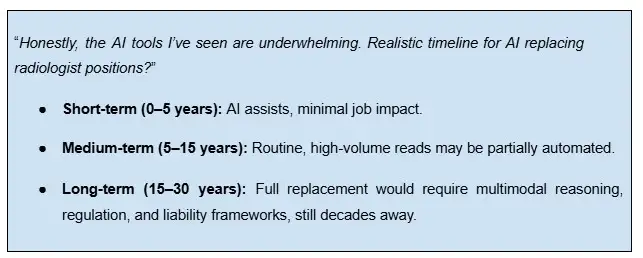
However, rather than shrinking, the profession is expanding into new areas, including interventional procedures, patient-facing communication, and advanced diagnostic strategies.
AI handles the volume, while radiologists handle the complexity. The partnership is where the future of radiology lies.
AI is Reshaping Radiology, But It Won’t Replace Radiologists
Radiology is already being reshaped by AI, though not through replacing its specialists. Instead, it is redefining the scope of the profession. The evidence indicates evolution rather than elimination.
Radiologists will shift toward higher-level roles, integrating clinical data, guiding treatment strategies, and delivering the human communication that patients need most.
AI will remain an essential partner, but never the final decision-maker.
For healthcare leaders, the takeaway is clear. Successful AI adoption in radiology requires investment in technology, training, and oversight.
The goal is not to replace clinicians, but to build a system where both radiologists and AI contribute to safer, faster, and more effective patient care.
At AAG Health, we combine innovation with people. Through our radiologist staffing services, we help hospitals and clinics build the right teams to thrive in an AI-enabled future.
If your team is evaluating how to integrate AI without losing the human touch, get in touch.
FAQs
Can AI Replace Radiologists?
No. While AI can read and flag medical images, it can’t assume legal responsibility for diagnosis, interpret results in a clinical context, or communicate findings to patients. Experts agree that full replacement is not realistic in the near future.
How Does AI Help Radiologists?
AI supports radiologists by triaging urgent cases, tagging potential abnormalities, and reducing time spent on high-volume routine reads. This allows clinicians to focus on complex analysis, interventional work, and direct patient care.
How are Radiologists Learning to Use AI Tools?
Training programs are starting to integrate AI literacy into the curriculum. Radiologists are getting trained to use and understand algorithms while also evaluating their performance, recognizing limitations, and ensuring outputs are clinically safe.
Why Can’t AI Replace Radiologists Completely?
AI lacks clinical reasoning, patient history integration, and the ability to deliver results with empathy. Also, it can’t take legal accountability for medical reports. These responsibilities require licensed professionals.
What Are the Risks of Using AI in Radiology?
Key risks include bias in training data, data privacy concerns, regulatory uncertainty, and over-reliance on algorithm outputs. Poorly performing AI tools can actually lower diagnostic accuracy when used without proper oversight.
What Legal and Ethical Problems Come with Using AI in Radiology?
Responsibility remains a gray area in the use of AI in radiology. Surveys show most professionals believe radiologists should remain legally accountable for AI-assisted diagnosis. Until regulations change, liability continues to rest on the physician signing of, not the algorithm.

