Radiologist shortages, months-long credentialing, and rising burnout leave your teams stretched and imaging backlogs unresolved. That delay hits your patient care directly, whether it’s a late stroke read or a CT scan waiting for review.
The truth is, your current model wasn’t built for the growth in imaging demand. Teleradiology changes that by giving you access to credentialed specialists, faster reads, and cost models that align with your volume.
In this article, we’ll break down how hospitals like yours compare costs, benchmark turnaround times, and solve staffing gaps with real numbers.
Let’s start with what teleradiology means in practice.
What Is Teleradiology?
Teleradiology is the practice of having remote, credentialed specialists interpret radiological images such as X-rays, CT scans, MRI, ultrasound, and mammography. Instead of waiting for an on-site radiologist, your facility sends the studies through a secure digital network to a licensed reader who delivers a report back into your workflow.
That process connects you with subspecialists (whether it’s a pediatric or musculoskeletal case) without carrying the cost of a permanent hire. The need for this approach is growing rapidly. Imaging demand keeps rising while the supply of radiologists lags.
The numbers tell the story. According to Grand View Research, the global teleradiology market reached USD 15.6 billion in 2024 and is projected to hit USD 60.3 billion by 2030, expanding at a 25.7% CAGR from 2025 to 2030. This growth reflects the pressure you already face, which is faster turnaround expectations, higher case volumes, and shortages across subspecialties.
For your hospital, imaging center, or health system, teleradiology is about:
- Keeping reads consistent 24/7.
- Reducing burnout among your in-house staff.
- Making advanced diagnostic services available even in high-volume settings.
What Teleradiology Really Means for a Hospital CFO/COO
For hospital CFOs and COOs, teleradiology is less about technology and more about financial structure and risk control. Instead of carrying full-time salaries with benefits, you can shift to a variable model where costs are linked to each exam read.
That means your expenses move with volume rather than locking into fixed overhead. It also strengthens operational resilience because credentialed specialists are available without the delays tied to internal recruitment.
The demand curve makes this shift urgent. According to Wikipedia, imaging procedures are increasing at nearly 15% each year, but the radiologist workforce is growing by only 2%. That imbalance forces you to either absorb delays and lost revenue or reframe staffing with alternative models like teleradiology.
Compliance factors also matter. Providers that manage licensure, malpractice coverage, and HIPAA standards reduce liability for your hospital while keeping reads continuous.
Next, we’ll explore why so many hospitals and imaging centers have turned to teleradiology.
Why Hospitals and Imaging Centers Rely on Teleradiology
The pressure on your radiology services comes from a gap that continues to widen. Anderson Hospital reported that imaging use in the U.S. is rising by 3-4% each year, but the radiologist workforce is only growing about 1%. This imbalance means you face longer backlogs and more overtime costs if you rely solely on in-house staff.
The economics make the choice even clearer. eVisit reports that a full-time on-site radiologist typically starts at $1,500 per day, while teleradiology offers per-exam pricing as low as $8. For you, that turns fixed labor into a variable cost that scales with your case volume.
More importantly, the model directly affects throughput. A Healthcare Service Journal report shows that 73% of radiologists say teleradiology helps clear backlogs, while 72% note workload reductions. Another study found a 71% reduction in patient waiting time once teleradiology was implemented. All of this is proof that response speed improves dramatically.

Quality gains are also measurable. According to EMResident, initiatives tied to teleradiology delivered:
- Mean ED radiograph turnaround time dropped from 23.9 minutes to 14.6 minutes.
- The percentage of radiographs read within 35 minutes rose from 82.2% to 92.9%.
- Doctor-to-disposition time decreased from 88.7 minutes to 79.8 minutes.
These gains keep scanners productive, shorten ER stays, and provide consistent access to subspecialists without hiring them full-time.
Business Case for Hospital Executives
For hospital leaders, teleradiology is a decision that changes how you manage fixed costs, staffing gaps, compliance exposure, and operational resilience.
These are the levers that matter most to your financial and strategic outcomes.
Cost Efficiency and ROI
Teleradiology allows you to convert fixed labor into variable costs. A full-time on-site radiologist with salary and benefits locks you into a daily spend regardless of volume. In contrast, per-exam billing aligns costs directly to workload.
Yes, we’ve already noted that rates can be as low as $8 per exam compared to $1,500 per day for an FTE, but here’s how it looks across a year. At 100 studies per day, your spend through teleradiology is $800 versus $1,500 for a single on-site hire. That’s a difference of more than $250,000 annually.
This efficiency also supports budget lines. A study at a rural hospital showed that the mean turnaround time for teleradiology consults was just 1.3 hours. More importantly, those reads changed initial diagnoses 30% of the time and shifted treatments 26% of the time.
Faster reads drove quicker clinical action, which directly improved throughput and preserved revenue by reducing delays in admissions and bed turnover.
Workforce Scalability
Teleradiology also gives you the ability to scale coverage up or down based on volume surges. ER spikes, trauma nights, or flu season can strain your internal staff.
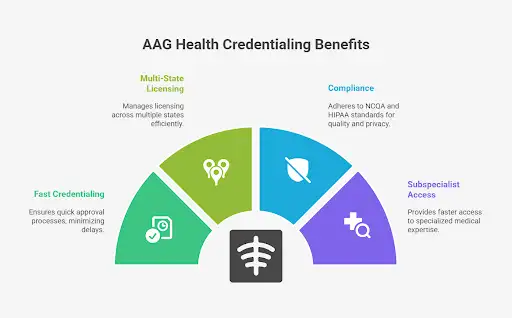
Credentialing new hires can take months, but experts like AAG Health place board-certified radiologists within days. That agility prevents costly ER diversion, protects imaging revenue, and lowers overtime expenses for your in-house team.
Instead of adding permanent staff for short-term surges, you could use teleradiology to absorb seasonal increases in imaging load. That means avoiding delays in diagnostic imaging turnaround and keeping scanners productive during peak hours without overextending your budget.
Risk Mitigation and Compliance
The compliance burden falls heavy when you expand coverage. With teleradiology, that work is carried out by the provider. Multi-state licensing, malpractice insurance, and HIPAA security standards are maintained without tying up your internal resources.
Key protections include:
- Encrypted transmission networks that protect medical images and patient data.
- Peer review and audit processes that strengthen quality assurance.
- Malpractice coverage that reduces direct liability risk to your organization.
When you outsource compliance tasks such as cross-state licensing and credentialing, you remove a major bottleneck in expanding coverage. This support allows you to add subspecialty reads, like stroke coverage on computed tomography scans, without waiting months for internal approvals.
The result can be earlier diagnoses, shorter ER boarding times, and more available beds for other admissions.
Next, let’s see how these financial and compliance levers impact day-to-day operations inside the radiology department.
Operational Impact for Radiology Directors
The question isn’t whether teleradiology works. It’s whether it can deliver subspecialist accuracy, turnaround consistency, and audit-ready quality on par with your in-house team. These are the operational factors that matter most.
Subspecialty Access Without Full-Time Hiring
With teleradiology, you can route cases directly to fellowship-trained subspecialists (neuro, breast, MSK, or pediatrics) without adding permanent FTEs. This matters because studies show that discrepancy rates rise when generalists read outside their training.
Aligning reads to subspecialists allows you to reduce repeat scans, cut delays, and prevent bottlenecks in bed flow.
Think about your stroke program. National guidance sets targets of ≤25 minutes from ED arrival to imaging and ≤60 minutes door-to-needle for thrombolysis. Remote neuroradiology support helps you meet those benchmarks even if your on-site staff is off-shift.
For radiology directors, that translates into fewer boarded patients in the ED, faster bed turnover, and smoother throughput across the hospital.
Turnaround Benchmarks
Benchmarks are clear. A JACR analysis of on-call networks found a mean turnaround time (TAT) of 12.2 minutes, with 93% of cases finalized in ≤30 minutes and 99% in ≤60 minutes. Even for routine studies, you can expect reports within a few hours.
The operational impact is direct:
- Faster reads reduce ER diversion.
- Scanners like CT and MRI stay fully utilized during peak demand.
- Scheduled outpatient imaging is preserved even in high-volume periods.
During respiratory virus season, for example, an ED can sustain <30-minute CT head reads via teleradiology while outpatient digital imaging studies are finalized within hours. That balance keeps both emergency throughput and scheduled revenue intact.
Quality Assurance
Skepticism about teleradiology quality is common. But published data show strong results. ACR RADPEER reviews report disagreement rates of about 3%, while large outsourced programs report discordance closer to 1%. In other words, structured remote workflows can match or exceed in-house performance.
Audit integration strengthens quality further. Studies report that around 3.3% of CT, MRI, and ultrasound studies are formally peer-reviewed, with departments reaching 50%+ compliance on scheduled peer-learning programs as they mature. RADPEER remains the national standard, which gives you a benchmarked, auditable trail.
Security also matters. HIPAA rules need strict protections (access controls, encryption, and log monitoring). Many teleradiology providers go further with end-to-end virtual private network segmentation, incident response drills, and structured audit trails. These measures protect radiological patient images and keep your department compliant with federal expectations.
Solving Imaging Center Bottlenecks
Backlogs build fast when a radiologist calls out or volume spikes unexpectedly. Every hour lost means scanners sit idle, studies pile up, and your staff faces mounting pressure. Teleradiology prevents those stalls by routing digital images through secure Picture Archiving and Communication Systems (PACS) to credentialed readers who can step in within hours.
With AAG Health, teleradiology credentialing is handled in days and not months like with other recruitment firms. That speed matters when a sudden shortage threatens throughput in a busy healthcare facility or in rural areas where coverage options are already thin. You don’t have to choose between delaying reads and overloading your in-house team.
Flexibility is built into the model. You can scale with locum tenens, part-time coverage, or per-exam billing. That way, if your center handles an influx of MRIs one week and lighter volume the next, you’re not locked into fixed staffing. Instead, you pay for exactly what you use while protecting both revenue and patient outcomes.
HR and Recruitment Perspective
Recruiting radiologists through internal channels is slow and expensive. Median time-to-hire across physician specialties runs 77 - 228 days, with radiology averaging around 130 days.
During that vacancy window, hospitals face revenue loss from idle scanners, ER diversions, and delayed image interpretation. Every 30 days shaved off time-to-hire accelerates bed turnover and protects imaging revenue that otherwise slips away.
Credentialing is another choke point. Standard hospital processes take 90-120 days, sometimes even more. By contrast, vendor-assisted models like AAG Health shorten that window to under 90 days with pre-verified credentialing packets, which is significantly faster than the norm.
This means subspecialist coverage can come online within weeks rather than months. It can help you avoid prolonged gaps in important services such as neuroradiology or magnetic resonance imaging.
Cost is also part of the equation. In-house physician recruiter compensation averages $109,241, while total recruitment costs per hire usually range from $180,000 to $250,000, when you factor in relocation, incentives, and onboarding.
Outsourced teleradiology shifts this fixed overhead to a per-exam model. This helps you align spend with demand and avoid vacancy-driven revenue losses.
At the same time, remote coverage reduces the after-hours burden on your in-house team. We previously noted that teleradiology helps clear backlogs and reduces workload. That relief directly supports retention by easing night call and lowering burnout risk among your staff.
Scaling Across Multi-Site Health Systems
For large healthcare organizations, the challenge is not access to radiologists at one site. It’s keeping quality and turnaround consistent across 10 or more hospitals and imaging centers.
Teleradiology makes this possible by applying uniform audit and peer-review processes across all facilities. That way, your board-certified consultant radiologists use the same quality framework whether they are reading for a suburban hospital or for urgent care centers in less common areas.
Technology closes the loop, and that’s where integration becomes critical. Linking radiology information systems, electronic medical records, and Intelerad PACS helps you create a consistent reporting framework across the network.
At the same time, secure VPNs combined with advanced cloud computing platforms protect patient records while also giving every radiologist equal access to tools.
Instead of building subspecialty coverage at each site, you can centralize. For example, neuro studies can be routed directly to an MRI radiologist, or pediatrics to a pediatric radiologist, without hiring them at every facility. Centralization reduces discrepancies, speeds reads, and avoids the inefficiency of duplicating staff across the system.
The result is consistency at scale, which means better diagnostic imaging procedures, faster throughput, and quality benchmarks applied equally across the enterprise.
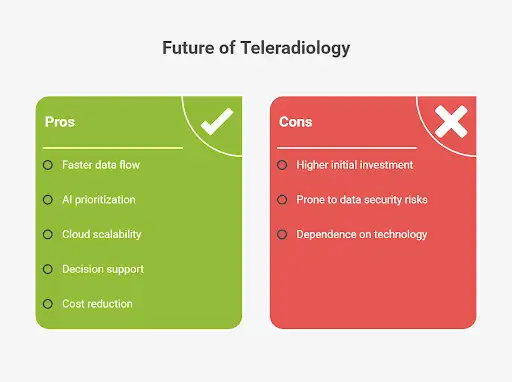
What Are the Disadvantages of Teleradiology?
No solution is without challenges, and teleradiology is no exception. The key is recognizing where risks exist and how they can be managed through structured systems and planning.
The most common drawbacks include:
- Technology reliance: Network downtime or PACS integration delays can stall reads. Because remote imaging depends on connectivity, even brief interruptions can slow radiology interpretation. Redundant hospital information systems and backup connections might mitigate this risk.
- Communication gaps: Without a radiologist on-site, there’s potential for miscommunication between clinicians and readers. Structured workflows, secure messaging, and embedded DICOM viewers within PACS minimize these gaps.
- Licensing delays: State-specific credentialing can take months. Working with a provider that handles cross-state licensing reduces the wait, so subspecialists like a musculoskeletal radiologist or experts in nuclear medicine can come online faster.
- Integration hurdles: Bringing teleradiology into your systems may require upgrades. Modern platforms use artificial intelligence and machine learning to automate routing, improve audit accuracy, and shorten turnaround times.
The truth is, these disadvantages don’t have to derail your strategy. With redundancy planning, credentialing-by-proxy, and integrated communication systems, you can turn potential risks into manageable variables. The right vendor shows you where the risks are and how to resolve them before they affect throughput.
Future of Teleradiology
The next stage of teleradiology will be defined by speed, automation, and seamless integration. AI-assistance in teleradiology already helps prioritize stroke and trauma cases, which pushes critical scans to the top of the queue so treatment decisions aren’t delayed.
Cloud-based platforms give you scalability, while 5G networks and predictive analytics bring faster and more reliable data flow across every facility.
These teleradiology trends directly connect to your concerns about throughput, revenue protection, and consistency. Healthcare professionals will gain stronger decision support through tools like automated voice recognition for reports and structured alerts on incidental findings.
For hospital executives, this means fewer bottlenecks, reduced costs, and uniform standards across multiple-site systems. AAG Health is a forward-looking partner in teleradiology. We offer AI-driven exam prioritization, cloud-based scalability, and fast staffing and credentialing.
Scale Your Radiology Team With AAG/H Proven Recruitment Services
Teleradiology has moved from an optional add-on to a core part of hospital and imaging strategy. It gives you cost control by replacing fixed salaries with per-study billing, speeds diagnoses with turnaround times measured in minutes, and expands subspecialty access without the weight of full-time hiring.
These advantages can help you protect revenue, reduce burnout, and keep patient flow moving across your system. And the fact is, scaling care without teleradiology will be harder each year.
To secure consistent coverage, fast credentialing, and reliable specialists, partner with AAG Health for proven teleradiology recruitment services.
FAQs
How does liability coverage work for outsourced radiologists?
Outsourced radiologists are covered under the malpractice insurance carried by the teleradiology provider. This means liability shifts away from your hospital, and the provider assumes responsibility for errors within their scope of service.
How does teleradiology integrate with PACS/EHR systems across facilities?
Integration is handled through secure connections that link your PACS and EHR directly to the teleradiology platform. Reads and reports flow back into your existing systems so your staff can view them without adding new steps.
What is the difference between radiology and teleradiology?
Radiology involves onsite specialists interpreting studies within your hospital or imaging center. Whereas teleradiology extends that capability remotely. It allows credentialed radiologists to interpret studies from other locations using secure digital systems.
What is an example of teleradiology?
A common example is emergency stroke care. A CT scan can be transmitted digitally to a remote neuroradiologist who interprets it in under 30 minutes. The report goes back into your system quickly and allows physicians in the ED to decide on thrombolysis without delay.

