Hospitals everywhere are under pressure. Staffing shortages stretch teams thin, backlogs grow, and burnout becomes harder to ignore. And if that's not enough, imaging demand keeps rising, yet delays in credentialing slow access to specialists and directly affect patient care.
That’s why remote radiology is no longer optional for your organization. It’s a proven way to keep scans moving without cutting standards. So, in this article, you’ll see how remote radiology reshapes operations, protects compliance, and supports financial stability.
P.S. Many hospitals are already turning to outside support to handle credentialing bottlenecks and rising imaging demand. What if your team had the same backup? AAG Health's teleradiologist recruitment services help you clear credentialing delays in days, reduce repeat reads, and keep reporting steady.
What Is Remote Radiology?
Remote radiology is the interpretation of diagnostic imaging such as X-rays, CT scans, MRIs, ultrasounds, and mammography by radiologists working outside your facility.
This is not outsourcing but an extension of your in-house radiology departments, delivered through secure PACS systems, RIS, and cloud-based platforms. You can use it to cover after-hours reads, manage rising volumes, and access subspecialists instantly.
Apart from that, adoption is growing quickly because it reduces reporting delays and broadens reach for hospitals in rural or underserved areas. In fact, a 2024 PubMed survey reported that 91.8% of institutions offered remote work, and 73% of radiologists were already working remotely.
Next, let’s weigh the advantages, drawbacks, and challenges of this remote radiology model.
Pros, Cons, and Challenges of Remote Radiology
Remote radiology has shifted from a backup option to a critical part of modern healthcare systems. Here are the advantages, drawbacks, and challenges that matter most to you as decision-makers weighing this model.
Pros of Remote Radiology
The benefits of remote radiology are not theoretical. They show up measurable gains for hospitals and radiology departments. The main ones to consider are:
- Faster turnaround: When your team struggles with backlogs, every delay cascades into slower care decisions. Remote subspecialists trained in hospital protocols can reduce repeat reads and reporting errors.
- Geographic freedom: You are no longer bound by the availability of local staff. A work-from-home radiologist can be in another state yet still provide remote access to urgent reads in your facility. This flexibility expands your reach and helps you avoid gaps when rural or regional markets struggle to hire.
- Subspecialist access: Hospitals without on-site expertise can instantly bring in neuro, musculoskeletal, or women’s imaging specialists. A practical example of this would be a small emergency department that uploads a trauma CT, and a remote neuroradiologist reads it within minutes. This level of remote support reduces transfer rates and speeds intervention.
- Reduced commute costs and stress: Radiologists working remotely experience less stress and don't spend hours in traffic and overhead tied to on-site shifts. For hospitals, the benefit is reduced need for extra space, equipment, and IT maintenance tied to radiology systems.
- Flexibility and work-life balance: According to the 2024 PubMed study we mentioned above, radiologists cite flexibility as a top benefit of remote roles. This translates into stronger retention and recruitment for your organization since physicians see better alignment between work commitments and personal lives.
- Increased efficiency: With AI tools and structured workflows, remote teams can focus on higher-value reads rather than repetitive cases. That frees up capacity and improves operational efficiencies across the department.
- Lower burnout for on-site teams: When night and weekend shifts are shared across a network, your in-house staff avoid chronic fatigue. That improves retention and long-term clinical productivity, which also reduces turnover costs that usually hit $250,000 - $1 million per physician.
Cons of Remote Radiology
Even with measurable gains, remote radiology comes with some challenges that you must anticipate. These are the most pressing issues reported by radiologists and administrators:
- Professional isolation: Remote radiologists risk losing daily interaction with clinical teams, which can reduce collaboration and mentoring opportunities. Over time, this impacts how connected they feel to your hospital’s mission.
- Limited career advancement: Promotion typically depends on visibility. Fully remote staff may miss tumor boards, committee work, or informal networking that builds leadership credentials.
- Potential for overwork: Without clear shift boundaries, some remote staff face pressure to extend hours or respond to non-urgent requests after shifts. Without structure, this cancels out the promised work-life balance.
- Technology and connectivity challenges: A single MRI file can exceed hundreds of megabytes. Inadequate bandwidth or outdated PACS systems create lags that slow reads. Even with virtual private networks in place, disruptions can affect reporting reliability.
- Licensing hurdles: Each state requires its own medical license with fees, CME requirements, and varying timelines. For global coverage, GDPR and HIPAA add further layers of compliance.
For more info, you can watch Marla Sammer, MD, MHA, and Daniel Oppenheimer, MD. In this video, they share their point-counterpoint of remote radiology:
Challenges & Mitigation of Remote Radiology
You cannot avoid the risks of remote radiology, but you can mitigate them with structured programs. These are the practical steps many hospitals now adopt:
- Bandwidth failures → redundancy: Invest in redundant networks, backup servers, and 5G connectivity where available. This keeps your imaging services online even during outages.
- Quality variability → QA programs: You can establish quality assurance with blinded peer review of medical images and audits of image quality. This reduces re-reads and protects patient outcomes.
- Lack of collaboration → structured virtual tumor boards: Remote meetings using encrypted platforms allow subspecialists and in-house teams to review complex cases together. This supports mentoring, maintains collaboration, and reduces the professional isolation that usually accompanies remote work environments.
Why Is Remote Radiology in High Demand Right Now?
The pressure on your imaging services is clear. More than 80% of health systems report staffing challenges in their radiology departments. This leaves you with delayed reads, strained staff, and reduced coverage. Imaging demand continues to climb, but hiring and credentialing haven’t kept pace.
The truth is, credentialing alone creates a serious barrier. TechTarget reports that provider credentialing delays average 90 to 120 days, which means a radiologist you hire today might not be able to read for months.
With AAG Health, you don’t wait months. Credentialed radiologists are placed in days, so your turnaround times improve immediately, and your team regains control instead of falling further behind.
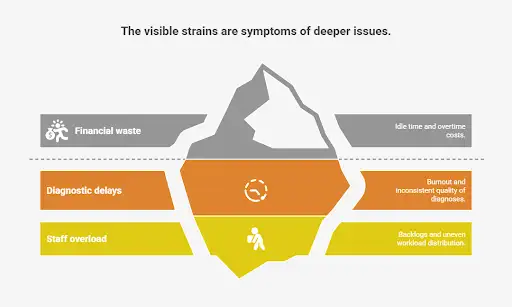
Without finding a solution to this issue, you feel the impact across leadership as well as clinical teams:
- CEOs/CFOs: Financial waste from idle time and costly overtime.
- CMOs/Directors: Diagnostic delays, burnout, and variable quality.
- Radiology staff: Overwhelmed by backlogs and uneven workload distribution.
Demand has peaked now because post-COVID hybrid models changed expectations, subspecialists remain in short supply, and rural hospitals increasingly rely on remote coverage to maintain standards. But let's be clear, you can’t wait for outdated processes to catch up.
How to Implement Remote Radiology in Your Organization
You can’t just switch on remote radiology and expect results. It takes planning across technology, staffing, and compliance. These are the steps that help you implement it in a way that supports your goals and avoids the common failures seen in other healthcare systems.
Step 1: Assess Imaging Needs and Gaps
The first step is to measure the pressure points in your radiology departments. Look at your current imaging volumes, backlog sizes, and where subspecialty shortages are most severe.
For example, an emergency department might see long delays in CT or MRI scanners at night, while outpatient clinics struggle with musculoskeletal reads. Burnout usually peaks during weekends or extended shifts, and that’s where backlogs grow fastest.
Tie this assessment directly to financial impact. Calculate the cost of overtime, delayed admissions, or transfer rates caused by gaps. If a trauma CT sits unread for hours, it delays surgery and increases risk.
Quantifying these outcomes gives you the justification for adopting a remote model that fills gaps quickly.
Step 2: Build the Right Technical Foundation
Once you know the demand, your next step is to make sure the infrastructure can support it. That means secure PACS/RIS integration, DICOM compliance, and sufficient bandwidth.
Downtime must be planned for with redundancy, because the question isn’t if the network will fail, but when. Solutions such as cloud PACS and remote viewing workstations allow radiologists to access studies across multiple facilities without delay.
IT leaders expect more than speed. You also need encryption, multifactor authentication, and alignment with HIPAA and GDPR. Hospitals that fall short here put themselves at risk of breaches and fines.
Cloud storage is extremely important for multi-site organizations. It provides instant access to prior studies and reduces the need for local servers by improving resource optimization.
Step 3: Credential and Onboard Radiologists
Credentialing is typically the single point of failure that slows new hires, so your process has to be tightly managed. Apart from collecting licenses and privileges, you need an organized system for verifying board certification, documenting subspecialty fellowship training, and aligning privileges across every facility you operate.
Onboarding is just as critical. Radiologists must be connected to your PACS and reporting systems from day one. They should also be trained on your local protocols and included in ongoing QA reviews.
This prevents the quality drift that happens when multiple rotating readers handle cases without oversight. Dedicated remote radiologists trained in your workflows build consistency, reduce re-reads, and stabilize reporting standards.
Step 4: Monitor, Evaluate, and Scale
Implementation doesn’t stop with deployment. You need continuous monitoring to prove ROI and maintain compliance. That’s why you should track KPIs such as turnaround, re-read rates, and staff satisfaction.
This means also pairing this with compliance audits for HIPAA and GDPR. In addition, remote workflows should be tested against ACR standards and your internal policies to confirm they meet clinical and regulatory expectations.
Scaling should then be gradual. Begin with after-hours or overflow coverage, and only once stable, expand to subspecialty reads or cross-network coverage. This staged approach gives you control while protecting collaboration.

Building the Right Technical Setup for Remote Radiology
Remote radiology only works if your technical setup is strong. These are the core components that support accuracy, compliance, and efficiency.
Core Equipment and Software Radiology Teams Depend On
The tools you choose shape outcomes. Each one has a direct impact on quality and workflow:
- Image acquisition devices: CT, MRI, and ultrasound machines must deliver clear inputs because poor capture cannot be fixed later. Accuracy at this stage prevents repeat scans and delays.
- PACS: This is the backbone for storing, retrieving, and sharing studies across devices. Without strong PACS integration, you lose speed and face reporting bottlenecks.
- DICOM standards: Standardization is important. Without DICOM compliance, images cannot move seamlessly across digital solutions, which risks reporting timelines and regulatory compliance.
- Radiology Information Systems (RIS): Cloud and web-based RIS give your staff access anywhere. Mobile and integrated options add flexibility but must sync with electronic health records to keep the workflow accurate.
How Images Are Transmitted and Stored Securely
Once captured, images need to move across systems without loss of detail or breach risk. These are the elements that matter:
- Data compression techniques: Lossless compression protects diagnostic accuracy, while lossy methods may corrupt data. Using the wrong approach leads to misreads and repeated scans.
- Secure network requirements: Encryption, penetration testing, and ongoing audits are needed to align with HIPAA and GDPR.
- Cloud storage solutions: Public clouds are cheaper, but hybrid or private models give you more control. For hospitals, a hybrid approach usually balances cost with security.
- Data security and encryption practices: Adopting SSDLC integrates security early and lowers the chance of system-wide failures later.
Telecommunication Tools That Enable Remote Radiology
Collaboration is only possible with reliable communication systems. These are the critical tools your team needs to use:
- Bandwidth and connectivity requirements: A 1 GB MRI file can stall reporting if the infrastructure is weak. Poor bandwidth increases the risk of delayed or missed diagnoses.
- Video conferencing tools: You can use built-in systems within PACS or external platforms. Encrypted third-party tools usually support subspecialist consults and tumor boards.
- Mobile technologies in radiology: Diagnostic apps on tablets and smartphones allow faster review in urgent cases. These tools support remote working while keeping clinicians engaged in decision-making.
Remote Radiology Cost Comparison: Per-Study Rates vs Fixed Hiring Costs
When you weigh the cost of in-house hiring against remote placement, the difference is striking.
An in-house radiologist carries a fixed cost model. The average salary is about $498,000 a year. And once you add benefits, malpractice insurance, and recruiting expenses, the real cost to you reaches around $808,000 annually (this reflects salary plus benefits using BLS ratios).
On top of that, credentialing delays of 90-120 days mean you’re paying without generating reads during that time. Depending on study volume, the per-study cost ranges anywhere from $101 at 8,000 studies a year to $40 at 20,000 (based on Medscape pay plus BLS benefit ratios divided by study volume). Unless your radiologist consistently handles the high end of that range, the per-study cost is steep.
Remote placement follows a per-read model. According to National Diagnostic Imaging, rates are around $12 for X-ray, $40 for CT, $25 for ultrasound, and $60 for MRI. There are no idle costs, and you only pay when studies are read, which matters when volume dips or shifts are uneven.
For a community hospital reading 10,000 studies annually, the cost is about $199,550, or roughly $20 per study. This is far below the $808,000 fixed spend of an in-house hire at the same volume.
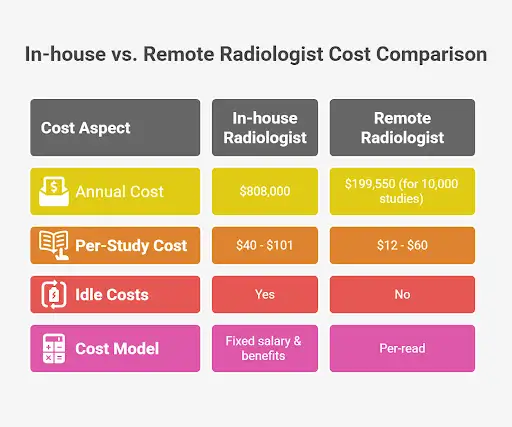
The truth is, an in-house radiologist's salary can be cost-effective at very high, steady volumes, especially in CT-heavy workflows. But for modest or unpredictable demand, the per-read model is cheaper and removes the hidden expenses of idle time, vacation backfill, or delayed onboarding.
That’s why many hospitals choose a hybrid approach, using teleradiology partners for nights, weekends, and overflow while keeping core staff on-site.
The Future of Remote Radiology
The financial and clinical pressures you face today suggest that you will increasingly rely on remote radiology in the years ahead. Market growth projections confirm this trend.
Grand View Research reported the sector was valued at USD 15.6 billion in 2024 and is forecast to reach USD 60.3 billion by 2030, with a CAGR of 25.7%. This pace reflects shortages of qualified radiologists and the growing demand for subspecialists in healthcare systems of all sizes.
New teleradiology trends will also shape adoption. A study of Aidoc’s AI triage for intracranial hemorrhage on head CTs found flagged outpatient scans were viewed 603.9 minutes faster, which cut delay by 89.6%, while inpatient delays dropped by 38 minutes. These gains prove how AI-assisted diagnostics can shorten wait times and reduce clinical risk.
Even so, the future won’t be fully remote. Hybrid models will dominate while blending onsite and remote reads to balance collaboration, compliance, and training needs.
Why AAG Health Is the Right Fit for Hospital Executives
With AAG Health, you stop waiting months for coverage. Our team manages licensing and credentialing across all 50 states, so qualified radiologists can begin reading in days.
That means you protect your workflow and avoid the costly backlog that comes with long credentialing cycles. This is where our teleradiology staffing services stand apart because we'll give you fast access to subspecialists without draining your internal resources.
Consistency also becomes the new standard. Instead of rotating readers who cause variability, you gain subspecialty-trained radiologists who stay aligned with your reporting protocols. The result is fewer re-reads, steadier turnaround, and higher confidence in every report delivered to your clinical teams.
From a financial standpoint, you only pay for completed reads and not idle overhead. For executives, that creates flexibility where you can scale from a single overnight shift to months-long coverage. We can adapt to your demand by letting you balance cost control with uninterrupted care.
Summing Up
Remote radiology has moved far beyond being a stopgap. It is now a central strategy for hospitals facing shortages, uneven coverage, and strict compliance demands.
AAG Health addresses the barriers that slow you down (long credentialing cycles, inconsistent reporting, and rising costs) by giving you access to credentialed subspecialists faster and more efficiently. That combination of speed, quality, and compliance helps your radiology departments protect patient care while avoiding the financial waste tied to idle staffing.
Contact AAG Health today to partner with a team that keeps your imaging precise, compliant, and uninterrupted.
FAQ
What does “remote” mean in radiology?
Remote radiology means radiologists interpret medical images like CT, MRI, or X-ray outside your hospital walls. They connect securely through PACS systems, RIS, and cloud platforms to access studies in real time. This setup expands your capacity without needing every specialist physically on-site.
How fast can a remote radiologist start work?
Industry averages show credentialing takes 80 to 120 days before a new hire can read. With AAG Health, credentialed radiologists can begin in far less time than that. That speed prevents bottlenecks and protects your turnaround times from slipping.
Is remote radiology secure and compliant?
Yes, if handled correctly. HIPAA and GDPR require encryption, audits, and strict access controls. ACR standards also guide how privileges, licensing, and malpractice coverage are managed across facilities.
Which radiology subspecialties can be covered remotely?
Coverage spans neuro, musculoskeletal, women’s imaging, and emergency reads. Subspecialists join your system virtually, using remote viewing workstations to stay aligned with your protocols. This allows you to fill gaps without delays or inconsistent reporting.

