Let suppose your facility hires a radiologist and sets a start date, but credentialing drags on. Weeks and then months pass before they’re actually allowed to see patients. In the meantime, your imaging rooms are idle, workflows stumble, and revenue slips through the cracks.
Delays like that happen all the time in the real world, and they hurt the bottom line as well as your ability to deliver care.
According to HealthStream’s 2023 report, only 44.5% of organizations are able to quantify their provider onboarding time. This shows that many of them lack full visibility over how long credentialing really takes.
Radiology credentialing often takes longer than other specialties because of multiple verification layers, subspecialty training, and complex payer networks. For HR leaders, medical staff offices, and operations executives, understanding this timeline is essential to keep staffing and revenue on track.
In this article, we’ll cover:
- What a typical radiology credentialing timeline looks like and how long it usually takes
- The key stages you’ll manage (and where bottlenecks often show up)
- Common risks and delay factors
- Smart tactics to speed up the process while staying compliant
- Ways to handle emergencies (locums, provisional privileges)
- The compliance and legal safeguards you can’t skip
P.S. If staffing gaps or slow credentialing keep holding your department back, check out our guide on the 10 Best Teleradiology Staffing Companies. It shares trusted partners that can help you maintain diagnostic coverage while you complete full credentialing.
What Is Radiology Credentialing?
Radiology credentialing is basically the process that greenlights a radiologist to work at your facility. It’s how you officially make sure that a provider is who they say they are, has the right qualifications, and is legally and clinically safe to treat patients. This is especially important when those patients are depending on accurate, high-stakes imaging reads.
It’s more than just checking a license. Credentialing pulls together a full picture of the provider’s:
- Education and training
- Board certifications
- Licenses (state and federal)
- Work history
- Peer references
- Malpractice claims history
- DEA registration, if applicable
- Background checks and sanction lists
In short, it’s a deep dive into a radiologist’s professional life to make sure they meet your facility’s standards and all relevant regulatory ones, too.
How is Credentialing Different from Privileging and Licensing?
This part can trip people up, so here's a quick breakdown:
- Licensing = State-level permission or authorization to practice medicine.
- Credentialing = Your facility’s verification process confirming the provider’s qualifications and background.
- Privileging = Granting the provider permission to perform specific procedures (e.g., reading MRIs, doing interventional work)
Each step plays a critical role in compliance and patient safety. Credentialing, however, is typically the most detailed and time-consuming phase. And the one most affected by administrative delays or incomplete documentation.

Typical Radiology Credentialing Timeline (Start to Finish)
So, how long does radiology credentialing usually take? The honest answer: it varies but most organizations should plan for 60 to 120 days from start to finish.
That range covers the full journey, from initial paperwork to final approvals. In some cases, things move faster (around 30–45 days), but that’s the exception, not the rule. Particularly, if your facility doesn’t have automated systems or if the provider’s paperwork isn’t 100% ready to go.
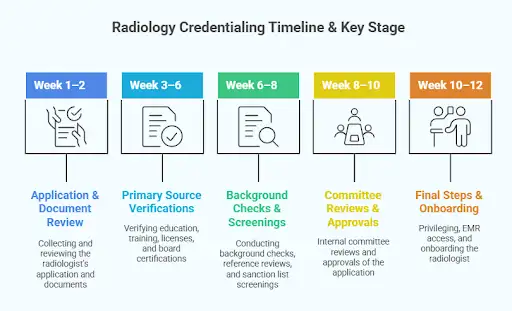
Here’s a general timeline breakdown:
- Week 1–2: Collecting and reviewing the radiologist’s application and documents
- Week 3–6: Primary source verifications (education, training, licenses, and board certifications)
- Week 6–8: Background checks, reference reviews, and sanction list screenings
- Week 8–10: Internal committee reviews and approvals
- Week 10–12: Final steps such as privileging (if needed), EMR access, and onboarding
Of course, these stages can overlap or pause depending on provider responsiveness, payer coordination, and your facility’s credentialing infrastructure.
Key Stages in the Radiology Credentialing Process
Let’s take a deeper look at each major step in the process, what you need to watch out for, and where delays often begin.
1. Application & Documentation Collection
This first stage sets the tone for everything that follows. The goal is to collect complete, accurate, and verified information from the radiologist before credentialing moves forward.
Key documents typically include:
- Educational transcripts, diplomas
- Residency and fellowship records
- State medical licenses
- Board certifications
- Employment history and references
- Malpractice history and claims
- DEA or controlled substance registration (if applicable)
- Identity proof, background clearance, etc.
Common pitfalls:
- Incomplete or inconsistent documentation from the provider
- Missing verification details (e.g., outdated license copies or expired board certificates)
- No standardized checklist across departments
Even minor gaps here can cascade into weeks of delay later in the verification or committee review stages.
2. Primary Source Verification
This stage involves contacting the original issuers of a provider’s credentials, like medical schools, licensing boards, and certification bodies, to confirm authenticity.
Many accrediting bodies (Joint Commission, NCQA, URAC) require primary source verification (PSV) as the gold standard.
However, this step is often the most time-intensive part of the credentialing cycle. Institutions vary widely in their response times, documentation formats, and administrative efficiency. These inconsistencies can easily stretch your overall timeline.
According to Medallion’s 2024 State of Payer Enrollment & Credentialing Report, around 60% of respondents said they spend more than half a business day (i.e. 4+ hours) just on primary source verifications for a single provider. Also, 52% of respondents still rely on entirely manual credentialing workflows, which compounds delays in verification steps.
Watch for:
- Slow or incomplete responses from verification sources
- Manual follow-ups that consume staff time
- Missing automation or tracking systems that delay updates
3. Background Checks & Sanctions Review
After credentials are verified, the process moves into risk and compliance screening. The goal here is to ensure the radiologist meets all federal, state, and institutional standards for safe practice.
This step typically includes:
- NPDB (National Practitioner Data Bank) queries
- State and federal sanctions or exclusion lists (e.g., OIG, GSA)
- Criminal background and fingerprint checks
- Verification of malpractice history and insurance coverage
- Review of any disciplinary actions or prior investigations
This stage often turns into a waiting period, as responses from government databases and external agencies can be delayed or require formal documentation requests.
Watch for:
- Slow NPDB or OIG response times
- Missing or inconsistent malpractice details
- Delays in fingerprint or background clearance processing
4. Committee Review & Approval
At this stage, internal governance takes over. The radiologist’s complete credentialing file goes through formal review and approval by designated bodies such as the Medical Staff Office or Credentialing Committee.
This step typically involves:
- Committee or department review of the credentialing file
- Peer review or clinical department input
- Votes or formal approval steps
- Possibly follow-up questions or “exceptions” that need extra documentation
Potential bottlenecks:
- Committees that meet infrequently or postpone reviews
- Competing agenda items delaying credentialing discussions
- Lack of digital systems to circulate files or collect votes
Streamlining this step with scheduled review cycles and electronic approval workflows can significantly shorten turnaround times.
5. Privileging (When Applicable)
For radiologists, privileging is a critical final step. It determines the specific procedures, imaging modalities, and subspecialties the provider is authorized to perform at your facility.
This stage typically includes:
- Reviewing prior experience, case logs or procedural history
- Assessing competency for specific modalities and interventional work
- Defining the scope of privileges for reading, interpretation, or hands-on procedures
If privileging is left until the end of the credentialing process, it can create last-minute delays or require rework, especially if additional documentation or peer evaluations are required.
Watch for:
- Missing case logs or incomplete competency documentation
- Delayed committee approval for new or advanced procedures
- Misalignment between the requested and approved privilege scopes
6. Final Onboarding & System Access
Once credentialing and privileging are approved, the process moves to final onboarding and system setup, the last step before clinical work begins.
This stage typically includes:
- Granting EMR, PACS, and RIS access
- Scheduling and billing system setup
- Completing orientation and compliance training
- Issuing staff badge, network IDs, and building access
Even though these tasks seem routine, delays here can become a problem. If IT or administrative teams are backlogged, the radiologist might be fully cleared but unable to begin seeing patients, which can cause unnecessary downtime and workflow disruption.
Why Radiology Credentialing Is Worth Planning Ahead
Delays in credentialing can quietly drain revenue and disrupt patient flow. In fact, McKinsey’s report on “Administrative simplification: How to save a quarter‑trillion dollars in US healthcare” estimates that inefficient administrative processes cost the U.S. healthcare system $265 billion annually, about 28% of administrative spending overall.
The financial impact runs deeper at the facility level. A study by Merritt Hawkins found that credentialing delays can cost healthcare organizations roughly $9,000 per provider per day in lost revenue, driven by extended wait times that disrupt the revenue cycle.
That’s why proactive planning matters. Build buffer time into your staffing plans, particularly for radiologists. Their subspecialty verifications and payer enrollments often require extra documentation and multi-step reviews. Factoring that in upfront helps avoid idle imaging suites and scheduling backlogs later.
Factors That Can Delay Radiology Credentialing
Even with careful planning, certain variables can throw off your credentialing timeline. Below are the most common culprits and ways to anticipate or mitigate them.

1. Incomplete or Inaccurate Applications/Missing Documents
If a radiologist submits a credentialing packet with missing items (e.g., missing reference letters, expired licenses, incomplete work history), the process can stall while back‑and‑forth communication happens.
This is one of the easiest “delay triggers,” because it often forces repeated checks or restarts.
2. Manual, Fragmented, or Legacy Workflows
As we learned previously, a lot of credentialing work, like data collection, verifications, and approvals, is still done largely by hand. This means delays, a higher risk of error, and needless extra work for busy staff.
3. Slow Responses from Primary Sources
When you reach out to universities, licensing boards, certification bodies, or hospitals to verify credentials, response times can vary widely. Some institutions take weeks to respond (particularly for older credentials or if records are archived).
International verifications can be even slower if the issuing body may no longer exist or may require special processes. These delays can easily ripple through the entire credentialing timeline.
4. Staffing Turnover, Resource Constraints, or Capacity Issues
Credentialing teams often operate with small teams, which means turnover or “key person risk” is real. If the main coordinator leaves or is out, backlogs can accumulate.
In the Medallion survey we looked at earlier, 57% of organizations reported turnover or staffing challenges in their credentialing or enrollment teams over the past year, which directly contributes to delays. When staff are stretched thin, even small deviations or extra follow-ups get deprioritized.
5. Committee Scheduling & Approval Bottlenecks
Even if all verifications are done, many facilities require review and approval by credentialing or medical staff committees. If these committees meet infrequently (say, monthly), you may wait days or weeks for a slot on the agenda.
Sometimes committees request additional documentation, which sends things back to earlier stages. This adds more time to an already lengthy process.
6. Privileging Complexity, Especially in Subspecialties
Radiology has many subspecialties like interventional, neuroradiology, remote radiology, teleradiology and breast imaging and more. Granting proper privileges requires reviewing prior case logs, subspecialty experience, and procedural volume.
Delay can creep in if the privileging scope wasn’t well defined early, or if reviewers push for more evidence of competence. Remember, the more specialized the role, the more documentation and peer input are required.
7. Delays in IT, Systems Access, and Onboarding Steps
Even after credentialing and privileging are approved, IT-related bottlenecks can still stall activation. If EMR/PACS access, scheduling systems, or network credentials are delayed, the radiologist may be cleared but unable to see patients.
Legacy IT systems, delays in provisioning accounts, or coordination across departments (IT, security, clinical informatics) can all lead to major slowdowns.
8. Payer or Insurance Panel Delays
Credentialing doesn’t end at the facility level. Providers must often be approved by individual payers or insurance networks before billing can begin. And each payer maintains unique documentation requirements and processing timelines.
If a payer delays its review, the radiologist may be ready clinically but unable to generate revenue under that payer’s contract.
9. Regulatory or Compliance Changes and Audits
New rules, changes in credentialing standards, or fresh regulatory scrutiny may require additional reviews or adjustments mid‑stream. If the facility is under audit or reviewing compliance practices, credentialing workflows might slow down while procedures are vetted.
How to Shorten and Streamline the Radiology Credentialing Process
Credentialing doesn’t have to be a drawn-out, paper-chasing marathon. The difference between a smooth, 60-day process and a 120-day mess usually comes down to preparation, coordination, and the right tools.
Here’s how the most efficient teams keep things moving.
Start before you think you need to
Kick off credentialing at least three months before your radiologist’s expected start date. This buffer absorbs delays from licensing boards, committees, or missing documentation before they snowball.
Get everyone on the same (digital) page
Whether you’re credentialing one radiologist or ten, a centralized, up-to-date checklist keeps you from scrambling to find missing documentation or rechecking details. Better yet, go digital. Credentialing platforms that track tasks, send alerts, and auto-verify credentials can shave serious time off the process.
Don’t wait for one step to finish before starting another
Credentialing doesn’t have to be a linear process. While you’re waiting on state license verification, for example, you can push background checks forward, prep the privileging paperwork, or get IT started on system access. The more you overlap tasks, the shorter the total timeline.
Keep communication flowing, especially with your provider
Your credentialing process is only as fast as its slowest response. That’s often the provider, especially if they’re not sure what’s expected. Regular check-ins, status updates, and clearly defined next steps make it easier for the radiologist to stay on top of their part.
Anticipate your internal choke points
Committee only meet once a month? Are IT teams always backlogged? Know where the common slowdowns are and plan around them. Some organizations hold standing meetings specifically for onboarding or use expedited review tracks to avoid unnecessary holdups.
And finally, track what’s working (and what isn’t)
You don’t need a full breakdown, but after each onboarding, take 10 minutes to ask:
- What caused delays?
- What could’ve been caught earlier?
- What systems or steps felt redundant?
Those small process improvements add up over time and make life easier for your next hire.
The Role of Locum Tenens and Temporary Privileges
Sometimes you don’t have 90-120 days. A radiologist might leave unexpectedly, volumes spike, or a new service line launches faster than you planned. That’s when locum tenens coverage and temporary privileges become your lifeline.
Locum Tenens Radiologists: Fast Relief, But at a Cost
Locum tenens radiologists can step in while you’re still credentialing a permanent hire. They’re credentialed through the locum agency and can usually be placed quickly.
The trade-off here is higher hourly/daily rates and less continuity of care. Still, they keep imaging services running and revenue flowing while you buy time for full credentialing.
AMN Healthcare found that 88% of healthcare facilities used locum tenens physicians in 2022 to fill staffing gaps.
Need fast, reliable locum tenens radiologists? AAG Health connects hospitals and imaging centres with board-certified tele-radiology locum tenens professionals who integrate quickly into your workflows.
Our team manages licensing, privileging, and payer coordination across all 50 states, so your diagnostic coverage stays uninterrupted while full credentialing continues.
Temporary or Provisional Privileges
Most facilities have a process for short-term or “expedited” privileges when the need is urgent. These privileges are typically granted under:
- Verified core credentials (medical license, DEA, board certification)
- Proof of no disciplinary history or sanctions
- Pending completion of the full credentialing file
Important note: Regulations vary. The Joint Commission allows for temporary privileges in specific circumstances (urgent patient need, or while awaiting governing body approval), but compliance must be airtight to avoid risk.
Remember, locums and temporary privileges are valuable tools, but they’re not a substitute for full credentialing. They should be seen as a bridge, a way to maintain service without compromising care.
Use them strategically for emergencies, seasonal spikes, or while waiting on slow credentialing verifications.
Compliance, Accreditation, and Legal Considerations
Credentialing is a legal and regulatory safeguard that keeps your organization compliant, accredited, and protected from serious financial risk. When it’s not done right, the fallout can include denied reimbursements, accreditation loss, or even federal penalties.
For starters, the Centers for Medicare & Medicaid Services (CMS) requires that all providers be fully credentialed and privileged before treating Medicare or Medicaid patients or submitting claims.
This rule sits at the core of CMS’s provider enrollment framework, and it’s non-negotiable. Section 135(a) of the Medicare Improvements for Patients and Providers Act (MIPPA) mandates that advanced diagnostic imaging suppliers, which include most radiology practices, maintain accreditation from an approved body to receive Medicare reimbursement.
Federal oversight also extends to compliance enforcement. The U.S. Department of Health & Human Services Office of Inspector General (OIG) continues to make healthcare fraud a top enforcement priority.
In its latest report, the government recovered more than $1.8 billion in civil healthcare fraud settlements and judgments under the False Claims Act. That figure covers a wide range of violations, not credentialing alone, but it’s a reminder of how costly compliance lapses can become.
To stay aligned, healthcare organizations must follow structured recredentialing cycles and maintain airtight documentation. Medicare Advantage regulations, for example, require recredentialing at least every three years to confirm licensure, board certification, disciplinary history, and performance metrics.
Likewise, credentialing teams must check providers against national sanction and exclusion databases, such as the National Practitioner Data Bank (NPDB) and the OIG Exclusions List, to make sure no one on staff is barred from participating in federal healthcare programs.
Thorough credentialing is your best compliance defense. Do everything you can to maintain a clear audit trail of every verification, approval, and privilege granted. If an audit or legal challenge ever comes your way, that documentation is your proof that your organization met every regulatory and accreditation standard that matters.
Partner With AAG Health for Reliable Radiology Staffing Support
Radiology credentialing doesn’t have to stall patient care or revenue. With the right planning, technology, and coordination, you can turn a 120-day process into a 60-day success story.
Building efficient workflows, tracking performance, and addressing bottlenecks early helps your imaging department stay compliant, fully staffed, and patient-focused year-round.
And when credentialing timelines stretch or unexpected staffing gaps appear, AAG Health has your back. We provide board-certified, fully credentialed radiologists, including tele-radiology locum tenens and permanent placements, to ensure uninterrupted coverage, faster turnaround times, and consistent diagnostic quality.
Contact us today to keep your radiology operations running seamlessly.
FAQs
1. How long does the radiology credentialing process usually take?
The radiology credentialing timeline typically runs between 60 and 120 days, depending on the complexity of the credentialing applications, the responsiveness of verification sources, and how organized your internal review is. Facilities that use automated credentialing software or centralized data management often see faster turnarounds.
2. Why is credentialing so important for radiology departments?
Credentialing is a way of making sure that every radiologist providing radiological services meets the standards for training, ethics, and regulatory compliance. It protects both patients and healthcare facilities, confirming that radiologists are licensed, qualified, and trained to interpret medical images like CT scans, MRIs, or Fusion imaging studies accurately.
3. What types of credentials do radiologists need to practice?
Radiologists must be certified by the American Board of Radiology (ABR) in diagnostic radiology, radiation therapy, or nuclear radiology. Many also pursue subspecialty certifications in fields like interventional radiology, neuroradiology, or pediatric imaging to validate advanced clinical expertise.
4. How do education and training fit into credentialing?
Education and residency training form the foundation of radiology credentialing. Radiologists must complete accredited programs, pass board exams, and maintain continuing education (CE) credits to stay current with evolving imaging technologies and clinical standards.
5. What role does communication play in successful credentialing?
Strong communication skills are often underestimated in credentialing management. Smooth coordination between healthcare providers, credentialing staff, and insurance payers helps ensure that credentialing applications move quickly through each step.
6. How can hospitals or clinics streamline radiology credentialing?
Hospitals can streamline credentialing by using digital tools that automate verifications, track deadlines, and store credentials securely. Running tasks in parallel and keeping clear communication with providers helps too. Or partnering with experts like AAG Health, who handle radiology licensing and privileging daily, can make the process faster and more reliable.
7. What happens if a radiologist isn’t credentialed on time?
If credentialing delays push past a start date, a facility may need to rely on locum tenens or temporary privileges to maintain service. However, radiologists who aren’t yet fully credentialed generally can’t bill insurance payers or work independently. This can disrupt patient scheduling and delay essential patient care services.
8. What’s the long-term benefit of investing in better credentialing systems?
An efficient provider credentialing program keeps your organization audit-ready, improves regulatory compliance, and supports faster onboarding of radiologists, which means your radiological services stay fully staffed.

