Vacancies in radiology hit operations hard. They reduce throughput, lower revenue, and strain staff. Hospitals facing shortages deal with backlogs, costly overtime, compliance risks, and rising patient complaints.
In fact, data shows that 22% to 36% of facilities report longer wait times, cancelled procedures, and declining satisfaction due to workforce gaps.
For a high-volume hospital, this means delayed diagnostic imaging and lost reimbursement. It also means patients leaving for competitors for outpatient imaging centers. The truth is that without a structured hiring approach, those gaps widen over time.
In this article, we’ll share how to hire a radiologist more effectively, shorten credentialing timelines, reduce turnover, and keep imaging services stable.
Let’s start with why the right radiologist makes such a difference.
Why Hiring the Right Radiologist Is Mission-Critical
Every executive in your system feels the strain when radiology roles remain unfilled. For CFOs, the costs mount fast. Daily spend on locum tenens coverage typically reaches $3,000 to $4,000 per physician, while missed scans translate into revenue lost to competitors.
CMOs and medical directors see the patient-facing risks, such as slower turnaround times, rising error exposure, and care teams pushed into burnout. At the board level, unresolved vacancies can trigger compliance penalties and reputational damage that extend far beyond one department.
The reality is that radiologist supply remains critically thin, with some regions having as few as 9 radiologists per 100,000 people. This creates pressure on patient access and increases compliance risk.
Subspecialty roles such as Interventional Radiology, Pediatric, Neuroradiology, and high-volume MRI/CT coverage make the challenge even greater. Broad recruitment won’t solve this. Hospitals need precise, evidence-driven hiring strategies to secure the right radiologists and protect patient access.
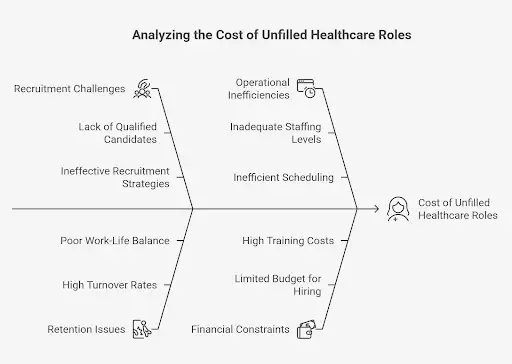
The Cost of Radiologist Vacancies for Hospitals
The operational and financial effects of a single vacancy reach far past basic scheduling gaps. Imaging bottlenecks create backlogs that slow emergency flow. Research has shown that even modest improvements, such as bundling just 10% of CT scans, can shorten emergency department stays.
Without adequate staff, hospitals absorb higher overtime costs for evening and weekend MRI and CT coverage. Compliance risks also rise, since accreditation bodies like the Joint Commission and ACR monitor turnaround standards closely. Financial leakage grows when patients leave for faster access at other nearby imaging centers, which weakens your market position.
One benchmark frames the scale. An unfilled healthcare role, including radiology, costs an average of $8,000 per day in lost productivity and revenue. For CFOs, that’s a direct hit to EBITDA, and for CEOs, it’s a persistent operational drag.
To address these gaps effectively, the first step is to define the exact role your facility needs.
Pro tip: If you want to see how hospitals are adapting to this shortage, we put together a guide on strategies to keep radiology departments running even under pressure.
Define the Role Based on Facility Needs
A vacancy in radiology is never just about filling hours on the schedule. The role you define will set the stage for cost, quality, and patient outcomes. Missteps at this stage create bigger issues later, from paying subspecialist rates for basic reads to losing patients because urgent cases wait too long.
These are the main areas you need to assess before hiring.
1. Assess Imaging Volume and Case Mix
Start with your actual demand. High-volume trauma hospitals see a different pattern than outpatient imaging centers that handle mostly routine exams. You should review daily MRI and computed tomography (CT) case loads, how frequently trauma patients need urgent reads, and whether weekend or evening coverage is needed.
If volumes are low at night, teleradiology can cover those hours. But if cases are high-acuity, in-house coverage is safer.
The truth is that defining volume incorrectly leads to waste like paying for subspecialty coverage you don’t need or worse, gaps in urgent care that delay treatment.
2. Decide on Subspecialty vs. General Radiologists
A generalist in Diagnostic Radiology can handle most standard cases. But some settings call for subspecialists. A children’s hospital may need dedicated Pediatric Radiology, while a trauma center typically depends on Neuroradiology or an Interventional Radiologist for urgent procedures.
Fellowship-trained subspecialists come with a higher cost, so you need to know when they are needed and when a generalist is enough. For example, an Interventional Radiologist averages $528,800 annually compared to $344,970 for General Radiology, which is about 35% lower.
Paying for advanced skills that don’t match your case mix strains margins without improving care. The right balance supports both patient safety and financial stability.
3. Establish Responsibilities and System Integration
The role of a radiologist goes far beyond producing radiology reports. You need someone who contributes to quality metrics, supports accreditation readiness, and engages in policy discussions that affect value-based contracts.
Active participation in quality assurance programs reduces malpractice risk and strengthens your compliance record. When radiologists are integrated into these efforts, they become strategic contributors to both care delivery and financial performance rather than just service providers.
Defining the role with this level of clarity creates a foundation for hiring success. Moving on, let’s look at the credentialing and compliance requirements that shape how quickly you can bring the right candidate on board.
Streamline Credentialing and Compliance Requirements
Credentialing isn’t a box to check. It’s the gatekeeper for revenue, compliance, and patient safety. Delays here slow service lines, stall reimbursements, and raise legal exposure. These are the areas you need to evaluate closely.
Certifications That Matter
The first step is validating certifications:
- ABR board certification for physicians.
- ARRT for technologists.
- Subspecialty CAQs in pediatric, interventional, or neuroradiology.
- CRA for administrators and ARDMS for ultrasound.
Each credential tells you something important about clinical readiness and legal compliance. The real risk is delay. The average credentialing window runs 60 to 90 days, but staffing support can reduce that to 30.
That difference usually means keeping an imaging service open or turning patients away. Faster onboarding protects revenue while keeping your facility compliant with accrediting bodies.
Verify State Licensure and Malpractice
State licensure checks sound routine, but lapses lead to lost reads and reimbursement delays. CFOs and CEOs know these aren’t minor issues because they can hit both margins and reputation.
Malpractice coverage is another layer of protection. Policies that include tail coverage limit exposure from past claims, and without it, the financial risk sits with your hospital or system.
Litigation costs and reputational damage typically fall directly under board oversight, so leaders need clear visibility into how malpractice is handled before a hire moves forward.
Front-load Background Checks and References
Employment verification, CME records, and disciplinary histories aren’t formalities. Overlooking them ties directly to revenue cycle risk. For example, a missed disciplinary action can later trigger reimbursement clawbacks, audits, or compliance violations.
The truth is that skipping due diligence upfront may save days, but it can cost months of financial loss once regulators step in. That’s why front-loading background checks is a financial strategy and not just an HR step.
Time-to-Credential and Revenue Impact
Every day of delay carries a real cost. A study by Merritt Hawkins found that delayed credentialing can cost around $9,000 per provider per day in lost revenue because of missed reimbursements and billing delays. If your credentialing window runs 90 days instead of 30, that’s more than $500,000 left on the table for one role.
AAG Health (Alpha Apex Group) reduces these windows by managing credential verification end-to-end, which turns credentialing speed into a direct lever for EBITDA and compliance. Tightening credentialing helps you protect both compliance and revenue.
Next, let’s discuss how to measure the technical and clinical competence that separates a good hire from a risky one.
Technical and Clinical Competence
Hiring a radiologist means securing someone who can meet the technical and clinical demands that drive both compliance and revenue.
Here’s what you should look at before moving forward.
Imaging Systems Expertise
Your radiologist has to be fluent in the systems that power daily operations. That means proven skill with PACS, RIS, and EHR integration across platforms such as Siemens, GE, and Philips.
When PACS is linked directly to the EMR, time to access a clinical note drops from 52 seconds to just 6 seconds. That’s a savings of 46 seconds per study, which translates into more than 8 hours saved per radiologist each year. Those hours can then be directed back to patient care, faster reporting, and shorter wait times.
Efficiency also comes from workflow design. Thanks to automation tools like “copy findings” and streamlined reporting templates, radiologists report an average of 68 minutes saved per day, with 95% confirming better efficiency. Over the span of a year, that’s weeks of work hours returned to your team.
Hospitals that adopt AI-enabled reporting see even stronger gains. Northwestern Medicine’s rollout of generative AI reduced report completion times by 15.5% on average, with some radiologists cutting as much as 40% off their turnaround without losing accuracy. Those gains reduce backlog and create a measurable lift in throughput.
Pro tip: If you want deeper insights into how AI is reshaping teleradiology and radiology reporting, read our full analysis on its impact and operational outcomes.
Assess Diagnostic Skills
Technical fluency means little without proven diagnostic accuracy. You need to evaluate candidates with practical case reviews tied to error rates and turnaround times. Peer-reviewed reports and emergency simulation exercises reveal strengths and weaknesses that affect malpractice risk.
Stronger diagnostic performance also feeds into value-based contracts, where scores in medical imaging quality directly influence reimbursement. When accuracy is high, both outcomes and margins improve.
Evaluate Communication and Teamwork
Radiologists also carry responsibility outside of reads. Presenting at tumor boards, participating in multidisciplinary rounds, and providing rapid consults all shape care coordination metrics.
This is where their communication skills matter most. You can use scenario-based interview questions to reveal how a candidate explains findings under pressure. Strong communication reduces delays in treatment planning, builds trust across clinical teams, and supports hospital-wide performance goals.

Why Technology Skills Are Non-Negotiable
The truth is that technology gaps create real costs. Fluency with PACS, RIS, and EHR means higher throughput and fewer bottlenecks. Also, familiarity with Siemens, Philips, or GE platforms prevents training delays and integration errors.
Radiologists who use AI-assisted tools safely can cut turnaround time without raising compliance risk. The wrong hire, by contrast, slows reimbursement cycles, adds to the backlog, and erodes ROI. In high-volume healthcare facilities, those delays are measured in millions.
The right mix of technical expertise, diagnostic accuracy, and teamwork gives you measurable financial and clinical returns.
Recruitment Strategies for Hospitals and Imaging Centers
Hiring the right radiologist takes more than posting a job ad. You face pressure from every side, such as compliance deadlines, CFO oversight, and patient backlog. To make progress, you need a clear framework for defining the role, sourcing candidates, and moving them through screening without delay.
These are the strategies that give you control over the process.
Craft the Right Job Description
A strong job description is your first filter against costly mis-hires. If you understate case complexity, you risk bringing in a generalist who can’t handle high-acuity imaging studies. But if you overstate, you end up paying subspecialist rates for work that doesn’t need that skill level.
The most effective descriptions include three anchors:
- Your daily imaging volume,
- Your mix of modalities, and
- Your compliance requirements.
When you put these in writing, you prevent misalignment that leads to unnecessary locum spend. Think of the description less as an HR formality and more as a contract with your finance and clinical teams on what you truly need.
Choose the Best Sourcing Channels
You have several options for sourcing talent, but each one carries tradeoffs:
- Professional associations like RSNA and ACR connect you to subspecialists, but the process is slow, and credentialing support is limited.
- Teleradiology and locum agencies cover immediate gaps, but costs are steep. Daily rates usually run in the thousands, and over a quarter, those expenses rival a full-time Radiologist's salary.
- Alumni networks and academic partnerships provide pipelines, but the flow is inconsistent and rarely supports urgent needs.
When you compare channels, you need to think in CFO terms. You need to ask yourself:
- How quickly does this source fill the seat?
- How much credentialing support is included?
- What are the retention outcomes?
A slow but cheap channel may cost you more in lost revenue than a fast one that comes with a fee.
Screening and Interviewing
Even when you source candidates, you can lose ground in screening. Generic interviews don’t surface the risks that lead to early turnover or compliance failures. Structured assessments give you measurable data.
For example, case reviews tied to turnaround times and accuracy rates tell you how a candidate will perform under pressure.
Also, peer interactions expose communication gaps that could stall multidisciplinary planning. The key is linking every step to retention and performance metrics. If you treat interviews as predictors of quality scores and compliance readiness, you avoid surprises months after hire.
Why Partner With a Healthcare Staffing Firm Like AAG Health
You can shorten these timelines even more by working with an experienced partner. AAG Health places board-certified radiologists, including subspecialists with subspecialty training, in as little as 72 hours.
Credentialing and licensing, which normally take months, are managed end-to-end. That reduces the window where you’re losing revenue on an open seat. Also, placement isn’t limited to generalists because you gain access to candidates aligned to your specific case mix, whether that’s trauma, pediatric, or advanced magnetic resonance imaging workloads.
The advantage is speed, but also alignment. By bridging the gap between sourcing and credentialing, a staffing partner like AAG Health addresses the three priorities every executive cares about: cost control, retention, and compliance.
Compensation, Benefits, and Retention
Compensation is a major driver of recruitment and retention. As you saw earlier, general diagnostic radiologists average about $345,000 annually, while interventional radiologists reach $528,800.
Across all radiologists, Medality data shows an average income of $437,000, but 10% of practitioners have reported pay declines due to market pressures. Geography matters as well, since some states fall far below the national mean while others compete at the top of the range.
Academic positions show a different picture. According to ZipRecruiter, salaries for faculty average about $344,970 per year, with most falling between $320,000 and $400,000.
That is close to $166 per hour and is far lower than compensation in private practice, where partners typically earn between $400,000 and $600,000, with senior partners exceeding those levels. The gap highlights why retaining talent in academic medical centers is such a challenge.

Compensation goes beyond base pay. A standard package usually includes CME allowances, malpractice insurance, health benefits, relocation support, sign-on bonuses, PTO, and retirement plans.
Private groups frequently take this further by offering 10 to 12 weeks of vacation, paid malpractice coverage, and maxed retirement contributions. For many physicians, these benefits weigh as heavily in their decisions as salary.
Retaining Radiologists in a High-Burnout Field
Retention is where the financial impact becomes most visible. Replacing one radiologist can cost you more than $250,000 when you factor in recruiting expenses and locum coverage during the gap.
There are options that can help you with this. For example, flexible scheduling (including per diem or teleradiology) helps prevent burnout and extends career longevity. Professional development, mentorship programs, and ongoing training in advanced imaging technology strengthen engagement while aligning staff with your modernization plans.
Tying compensation and benefits directly to retention strategies allows you to lower turnover risk and protect EBITDA. The cost of losing one radiologist is steep, but the value of keeping them engaged, supported, and committed is far greater.
Secure Top Radiology Talent with AAG/H
Hiring a radiologist is a financial, clinical, and compliance decision all at once. You’ve seen how misaligned job definitions, credentialing delays, and weak retention strategies can drain resources and weaken outcomes. In contrast, structured hiring, clear role design, and strong retention planning protect both EBITDA and care delivery.
In a market where radiologists are in short supply, you can’t afford to take risks with open roles. AAG Health gives you direct access to board-certified radiologists and the systems to move them into place quickly.
Contact AAG Health today to secure the radiology coverage your facility needs.
FAQs
How fast can I realistically fill a radiologist vacancy?
Filling a radiologist vacancy usually takes three to six months using traditional hiring methods. During that time, you face lost revenue and patient backlogs. However, with AAG Health, placements can happen in as little as 72 hours because credentialing support, background checks, and role alignment are handled in parallel.
What’s the cost difference between locum and permanent hires?
Locum radiologists can cost $3,000 to $4,000 per day, which quickly surpasses the annual salary of a permanent hire. Permanent physicians average $345,000 to $437,000 depending on subspecialty, region, and practice type. When you compare those numbers, using locums for months at a time places significant strain on margins.
What are the key performance indicators for the radiology department?
You should track turnaround times for medical imaging procedures, accuracy of radiology reading services, compliance with accreditation standards, and impact on patient throughput. Financial KPIs include revenue per imaging modality, overtime spending, and the contribution margin of each radiologist.
How can a staffing firm cut credentialing delays?
Credentialing delays typically stretch 60 to 90 days, which costs you missed billing and compliance risk. AAG Health reduces this window by managing medical licensure, certification verification, and radiologist profiles through a centralized process. That approach shortens the credentialing timeline to about 30 days, protects reimbursements, and gets radiologists in place faster.

