Many healthcare leaders still treat “telehealth” and “telemedicine” as interchangeable terms. In patient-facing conversations, that might not matter. But when you’re hiring, the distinction is critical.
The global telehealth market was valued at $123.26 billion in 2024 and is projected to reach $455.27 billion by 2030, growing at a nearly 25% CAGR. That growth is fueling demand for talent.
This article breaks down the telehealth vs. telemedicine recruiting and what sets these two paths apart. Knowing where the lines are drawn helps you hire smarter and build a stronger remote care team.
No matter if you're scaling virtual services or filling in your first remote role, this breakdown will give you the insights you need to ace the hiring process.
TL;DR
Hiring for virtual care but short on time to read? These are the key takeaways:
- Telemedicine focuses on providing clinical treatment, such as virtual doctor visits, e-prescriptions, and diagnostics.
- Telehealth is broader. It covers both clinical and non-clinical support, like wellness coaching, care coordination, and remote monitoring.
- Each side of the spectrum needs different skills, licenses, and recruiting strategies.
- Telehealth recruiters face rising demand, multi-state licensure hurdles, and compliance risks. In-house hiring teams may not be equipped to navigate this.
- Partnering with a niche recruiter like AAG/H can save time, reduce turnover, and improve quality of care, especially for high-skill or multistate roles.
What’s the Difference Between Telehealth and Telemedicine?
"Telehealth" and "telemedicine" are sometimes used interchangeably. But in recruiting, that shortcut creates problems.
Let’s be clear: Telemedicine is a subset of telehealth. All telemedicine is telehealth, but not all telehealth is telemedicine.
Let’s get deeper into the differences:
What is Telehealth?
Telehealth refers to the full range of remote healthcare services delivered via technology. This includes both clinical care and non-clinical activities that support patient well-being.
Key examples include:
- Health coaching for chronic condition management.
- Remote patient monitoring using wearable devices.
- Wellness apps that track sleep, nutrition, or mental health.
- Virtual group education sessions or administrative meetings.
- Provider training and continuing medical education.
According to the Health Resources & Services Administration (HRSA), telehealth encompasses provider training, administrative meetings, and continuing medical education, in addition to clinical services.
That distinction matters when hiring for operations, IT support, or patient outreach roles.
Also, adoption is widespread. In 2024, 95% of HRSA-funded health centers used telehealth to deliver primary care. This level of adoption shows that telehealth is now a core part of healthcare delivery.
What is Telemedicine?
Telemedicine refers strictly to remote clinical services delivered by licensed professionals. It’s patient care at a distance.
Common formats include:
- Real-time virtual visits with physicians, therapists, or nurse practitioners.
- E-prescribing and remote medication management.
- Remote diagnostic evaluations and follow-up visits.
- Clinical video telehealth consultations in specialties like dermatology or psychiatry.
It’s not just a trend that came about during the COVID-19 pandemic. It’s becoming the norm in the industry, and for good reason. According to the Doximity State of Telemedicine Report:
- 88% of physicians say telemedicine increases patient access.
- 87% of physicians believe telemedicine allows them to provide care to patients who may be unable to visit in person (presumably leading to greater patient satisfaction).
- 70% are more likely to seek help for non-emergency issues if telemedicine is an option.
Obviously, the appeal is there. Patients get faster care without travel, and providers can work more flexibly. But that flexibility doesn’t reduce the need for strict compliance, credentialing, and strong clinical skills, which is where many hiring efforts fall short.
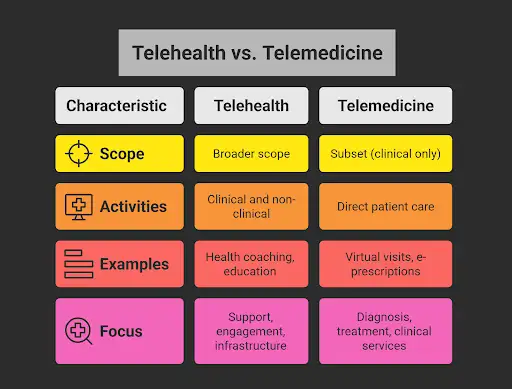
Side note: Still unsure where one ends and the other begins? Our breakdown on the differences between telemedicine and telehealth clarifies what sets them apart.
Telehealth vs. Telemedicine: Why Does This Difference Matter in Recruiting?
Knowing the terminology is only part of the equation. What really matters is hiring the right people with the right qualifications for the right roles.
Confusing telehealth and telemedicine in recruiting can lead to mismatched hires, compliance risks, and wasted time. Here's why telemedicine and telehealth recruiting are different:
Different Roles Require Different Talent
Recruiting for virtual care means understanding who does what, and what each role actually requires.
Telemedicine roles are clinical. They demand licensed professionals who can diagnose, treat, and prescribe remotely. For example, you may want to hire the following healthcare practitioners for telemedicine jobs:
- Physicians (MDs, DOs).
- Nurse Practitioners (NPs).
- Physician Assistants (PAs).
- Therapists (PT, OT, SLP).
- Mental health professionals (psychiatrists, psychologists).
These professionals need experience in remote consultations, a strong grasp of digital documentation, and up-to-date licensure across state lines.
Telehealth roles, on the other hand, may be clinical or non-clinical. Many support the care delivery system without offering direct treatment.
Most common roles include:
- Health coaches and care coordinators.
- Remote patient monitoring technicians.
- Behavioral health support staff.
- Telehealth coordinators.
- Medical scribes.
- IT support for telehealth platforms.
These roles focus on engagement, compliance, workflow, and infrastructure. They typically require strong communication, tech proficiency, and healthcare system knowledge, but not always clinical credentials.
Legal & Compliance Considerations
Regulatory complexity is a major friction point in recruiting for virtual care.
Licensing laws vary by state, and telemedicine providers sometimes need multiple state licenses to treat patients across state borders legally. This creates a moving target for in-house hiring teams.
Industry data backs this up. An MRINetwork brief highlights how licensing and credentialing remain persistent hurdles in telehealth recruitment.
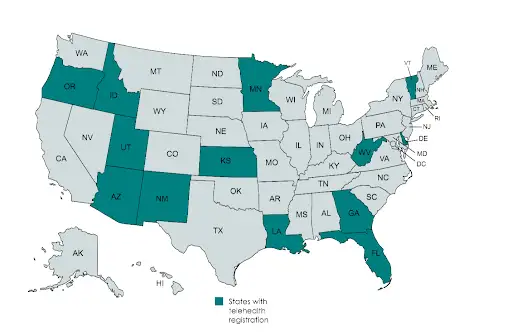
Hiring the wrong candidate (or missing a licensing detail) can lead to delays, legal risk, or even halted services.
Then, add to that the following:
- Varying reimbursement policies by payer and region.
- Data privacy regulations (HIPAA, HITECH).
- Malpractice insurance concerns cross state lines.
Finding a provider is only half the job. The key is choosing one who’s qualified to deliver care legally, safely, and effectively in your particular setting.
What Makes Telehealth and Telemedicine Recruiting Challenging (And Why Work With a Recruiting Agency)
Virtual care is scaling fast, but the recruiting systems behind it haven’t caught up.
Many hospitals, clinics, and health systems struggle to hire for these roles internally. They’re applying traditional recruiting models to a fundamentally different structure.
Here’s why that doesn’t work, and why niche recruiting partners are stepping in to fill the gap.
Key Challenges for In-House Teams
Recruiting for virtual care throws operational and regulatory complexities that many internal teams aren’t equipped to handle. They face so many hurdles, like:
- The roles aren’t clearly defined: Telehealth and telemedicine roles are distinct but may also overlap. Titles like "telehealth coordinator" or "virtual care nurse" mean different things across organizations.
- Screening for remote-readiness is tough: Communication style, tech comfort, self-motivation, and other soft skills are all the more important for virtual roles. However, these skills are rarely assessed well in standard interviews.
- Licensing and credentialing slow everything down: Multi-state practice is more common than ever (that’s kind of the whole point of telehealth). But without expertise in licensing laws, in-house teams hit bottlenecks and may even make non-compliant choices.
- Demand is high, and competition is fierce: With telehealth usage rising 6.13% nationally in the second half of 2024 alone, it’s clear more people are turning online for healthcare. Top virtual care professionals are in short supply.
- Retention is harder when teams are remote: Poor onboarding, unclear expectations, and a lack of connection lead to faster burnout and turnover. This risk increases when the team isn’t trained to manage remote workers.
Why Working With a Recruiter Makes a Difference
The margin for error in virtual care hiring is small. The roles are specialized, licensure varies by location, and the demand far outpaces supply.
That’s where a dedicated healthcare recruiter with telehealth and telemedicine expertise makes a measurable impact. Specialized recruiters bring clarity, speed, and precision to a hiring process that’s become increasingly complex and high-stakes.
Here’s what that looks like in practice:
- Role-specific knowledge: A recruiter who understands the difference between a telemedicine provider and a telehealth support role won’t waste your time (or theirs) on mismatched candidates. They know what each role requires and where to find qualified talent.
- Stronger job descriptions: Accurate, well-scoped job postings draw the right candidates and repel the wrong ones. Recruiters translate your needs into clear, targeted listings that reflect both the role and the regulatory context.
- Access to pre-vetted talent: Niche recruiters maintain networks of vetted professionals across clinical and non-clinical virtual care roles. That includes candidates already licensed in multiple states, which reduces and eliminates credentialing delays.
- Compliance is built into the process: Experienced recruiters manage the compliance side proactively, not reactively. They cover licensure requirements and telehealth-specifc malpractice coverage.
- Faster time-to-hire: With ready-to-go candidates and a streamlined vetting process, time-to-fill drops significantly, minimizing disruption to care delivery. For instance, at AAG/H, the average placement time ranges between 55 to 90 days, which is less than the industry average of 120 days.
- Retention strategies that work: Virtual teams require different onboarding, management, and communication practices. Recruiters who understand this can help place candidates who are more likely to succeed and stay in a remote care environment.
A recruiter’s job is not simply to place someone in a role. In fact, it’s to ensure the position is filled properly, in line with regulations, and with long-term success in mind.
Convinced to work with a recruiting agency? Explore AAG/H telehealth and telemedicine recruiting services to find the best talent for the specific roles, ready to get started.
What Should Recruiters Look for in Telehealth and Telemedicine Candidates?
Hiring for virtual care means looking beyond the résumé. Clinical expertise or tech proficiency is only part of the equation. The best candidates also need to be adaptable, autonomous, and fluent in remote workflows.
Here’s what to prioritize:
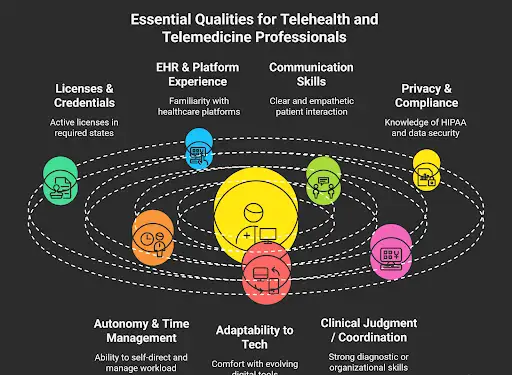
- Relevant licenses and credentials: For telemedicine roles, verify active clinical licenses in all applicable states. Delays in this area can stall onboarding, so multistate eligibility is a competitive advantage.
- Experience with EHR systems and telehealth platforms: Be it Epic, Teladoc, Zoom for Healthcare, or proprietary tools, familiarity with electronic health records and virtual care platforms ensures a faster ramp-up.
- Strong communication skills: Clear, compassionate communication is all the more important when care happens through a screen. This includes patient-facing clarity, as well as documentation precision.
- Data privacy and HIPAA compliance: Candidates should have awareness of data protection protocols, specifically those related to the healthcare industry, like HIPAA. They should also understand the importance of secure communication tools.
- Autonomy and time management: Remote care professionals need to self-direct, manage virtual schedules, and handle tech issues with minimal support.
- Adaptability to new tech: Virtual care tools are progressing quickly. Candidates who are open to learning and comfortable navigating new systems will adjust more easily to changing demands.
- Clinical judgment or care coordination expertise: Depending on the role, either clinical assessment skills (for telemedicine) or strong organizational abilities (for telehealth) will be essential.
These are not just added perks but essential competencies that improve patient outcomes, streamline operations, and ensure your virtual care model functions as it should.
A bad hire in healthcare hurts care quality and drains budgets. Take a look at the true cost of healthcare recruiting and retention to see why precision matters.
How to Recruit Talent for Telehealth and Telemedicine Roles
Recruiting for telehealth and telemedicine calls for a more targeted, strategic approach that considers regulatory risks, role definitions, and readiness for remote work.
Start with these core tactics:
- Customize job descriptions: Use precise role titles and outline specific tech, licenses, and communication requirements. Clearly distinguish between clinical and non-clinical expectations.
- Post in the right places: Go beyond job boards. Target associations, certification groups, and specialized healthcare platforms where remote-ready professionals are active.
- Train your hiring team: Ensure interviewers understand the key differences between telehealth and telemedicine roles, and how to screen for soft skills like virtual communication, autonomy, and adaptability.
- Evaluate platform fluency: Consider testing candidates on the tools they’ll actually use on the job. This makes onboarding smoother and fewer tech issues post-hire.
When to Work With a Healthcare Recruiting Agency
Managing recruitment internally works only up to a point. Once credentialing complexity, time pressure, or role clarity start to slip, partnering with a healthcare recruiting agency may be your best bet.
It can be particularly beneficial to work with a healthcare recruiter if:
- You’re expanding virtual care across multiple states.
- You need to fill niche clinical roles with multistate licenses.
- Your in-house team lacks experience with remote workforce screening.
- Compliance concerns are slowing down hiring.
- You need to reduce time-to-hire without sacrificing candidate quality.
Niche healthcare recruiters bring tested systems, regulatory expertise, and ready networks of qualified talent. For fast-scaling virtual care programs, that’s essential for staying competitive.
We’ve compiled a list of the best telemedicine recruiting companies to help healthcare leaders evaluate the best partners in the industry.
Build the Right Virtual Care Team
Telehealth and telemedicine are shaping the future of healthcare. Sadly, recruiting for these roles is still catching up.
The distinction between them has a real operational impact. It defines the skill sets, credentials, and compliance standards your workforce needs.
At AAG Health, we understand that the right hire isn’t just about filling a position. That’s why we help medical facilities recruit the right telehealth and telemedicine professionals.
As an American Staffing Association (ASA) member, compliance is second nature to us. We know how important it is to ensure telehealth and telemedicine hires meet and understand regulatory requirements.
Are your job descriptions precise? Are your teams trained to evaluate for remote-readiness? Do you have access to multistate-licensed candidates? If the answer isn’t a confident “yes,” it may be time to bring in a specialized partner.
Get in touch, and we’ll guide you through every step of the process.
FAQ
What’s the Difference Between Telehealth and Telemedicine Roles?
Telemedicine roles are strictly clinical and require licensed healthcare professionals who work through remote supervision and video visits. Telehealth is a broader industry, combining clinical and non-clinical roles such as coordinators, IT staff, and patient engagement teams.
Do Telemedicine Professionals Need Different Licenses than Traditional Healthcare Workers?
Yes, telemedicine providers must hold an active license in every state where their patients are located. This adds complexity to talent acquisition and makes multistate credentialing essential to avoid compliance delays, especially for medical centers serving multiple regions.
What Types of Non-clinical Roles are Included in Telehealth?
Telehealth staffing covers more than advanced practice clinicians. Roles include telehealth coordinators, patient data specialists, and IT support who manage video visits and phone consultations. These positions may not always be directly related to medical practice, but rather support it. They ensure smooth operations, protect patient information, maintain healthcare records, and support healthcare providers.
Should I Hire Telehealth and Telemedicine Candidates Through the Same Channels?
Not always. Telemedicine professionals, who manage direct medical consultation and medication administration, are best recruited through medical associations, licensing boards, or specialized recruiters. Telehealth roles can be sourced via digital health job boards, IT networks, or specialized telehealth staffing and recruitment services that know how to balance clinical and tech needs.
Should You Work with a Healthcare Staffing Agency?
Yes, particularly when building or scaling a telehealth team across states. Agencies specializing in virtual care can streamline credential checks, reduce compliance risks, and provide faster access to qualified professionals. Also, strong staff training programs offered by these agencies help teams adopt new telehealth technology smoothly and maintain high standards of care.
How Does Telehealth Hiring Affect Retention and Workforce Satisfaction?
When done well, telehealth hiring improves retention. Providers report more flexible schedules, reduced in-person visits, and fewer administrative burdens. But if digital fluency or communication skills are overlooked, turnover increases. Similarly, clinical history documentation can suffer, leading to gaps in continuity of care.
What Mistakes Should Organizations Avoid When Hiring for Virtual Care?
Common errors include mixing up telehealth and telemedicine roles, overlooking state licensing, and underestimating the need for digital readiness. Weak job descriptions or poor handling of patient information security can also create compliance risks due to mismatched hires.

