The radiologist shortage is no longer a warning call. It’s happening now, and many imaging departments are already feeling the strain. And current trends show it will not improve over the next three decades without deliberate action.
According to the Harvey L. Neiman Health Policy Institute, the radiologist workforce may grow 25.7% between 2023 and 2055, but imaging demand is expected to rise 16.9% to 26.9% depending on modality, and even higher in high-growth regions. This means the gap will remain unless organizations tackle systemic causes.
As workloads grow faster than staffing pipelines, burnout, turnover, and workflow delays increase. HR teams, recruiters, and facility leaders are left balancing patient volume with radiologists' well-being.
This article breaks down what’s driving the shortage, why burnout continues to rise, and what facilities can do to support and retain their radiologists. It also shows how AAG Health can help through flexible locum-tenens coverage and teleradiology support when traditional hiring isn’t enough.
The Radiologist Shortage and Its Impact
What do we really mean by “radiologist shortage”? It refers to the growing gap between how many radiologists are available to read imaging studies (like CTs, MRIs, X‑rays, and nuclear‑medicine scans) and the rising demand for those studies.
When supply doesn’t keep pace with demand, facilities end up with long wait times, backlogs, and mounting pressure on the radiologists who remain, and that’s exactly what’s happening now.
Current trends show that demand is climbing much faster than the workforce can grow. Imaging use continues to rise because of population aging, higher chronic-disease rates, and broader reliance on diagnostic imaging across specialties.
At the same time, the workforce is aging, and 53% of radiologists are now over 55, which means retirements will add even more strain over the next decade.
As a result, radiologists are reading more studies per day, meeting tighter turnaround expectations, and working with little recovery time between cases.
The downstream effects show up across the care continuum. Patients experience delayed diagnostics, clinicians wait longer for reports, and facilities struggle with growing imaging backlogs.
These pressures also increase the risk of fatigue-related errors. According to the Global Radiologist Report 2025 by EverlightRadiology, 53% of radiology professionals identified burnout as their top concern for the field's future.
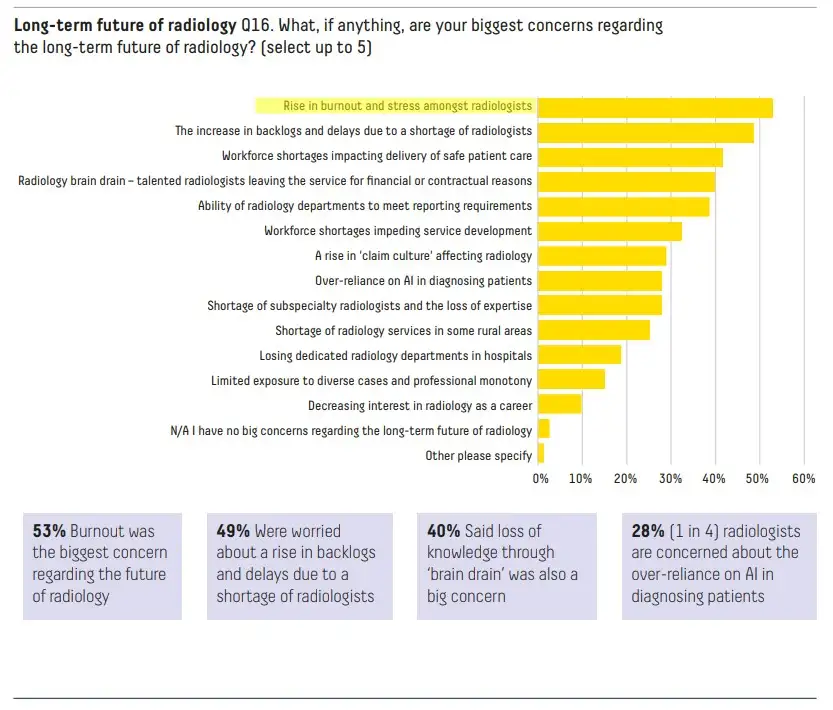
“There was broad agreement that the radiology profession faces significant challenges, including radiologist burnout, workforce shortages, brain drain, and the impact of overnight shifts on radiologists’ wellbeing and patient safety.” - Dr Dan Rose, Medical Leadership Council, EverlightRadiology
Burnout in Radiologists: Why It’s Happening and Why It Matters
Burnout among radiologists is a real syndrome, marked by emotional exhaustion, detachment, and a growing sense of professional ineffectiveness.
Studies show just how widespread the problem is: a 2023 meta‑analysis estimated that nearly half of radiology residents exhibit one or more of burnout’s core symptoms (emotional exhaustion, depersonalization, or low personal accomplishment).
Another recent study of practicing radiologists found rates as high as 46% showing clear signs of burnout.
So what’s driving this? Here are several factors specific to radiology that make burnout more likely:
- Heavy and growing volume of imaging studies, sometimes outpacing the growth of the radiologist supply
- Social and professional isolation. Many radiologists work alone in reading rooms or even remotely, often with minimal patient contact.
- High pressure to meet turnaround times, juggle complex modalities (CT, MRI, nuclear medicine, interventional studies, etc.), and handle frequent interruptions or admin tasks outside core reading duties.
- Work–life imbalance due to long hours, overnight calls, and unpredictable schedule demands, especially in subspecialties like interventional radiology
- Systemic pressures like unrealistic productivity targets, administrative burdens, and a lack of autonomy or control over scheduling or equipment
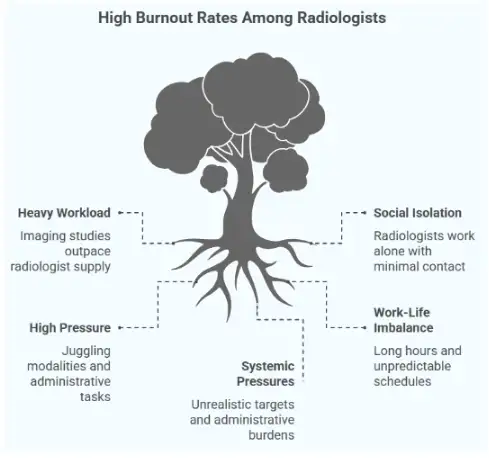
When radiology departments are understaffed, all these pressures ramp up. Fewer radiologists means each one needs to carry a heavier load, with less room for rest or recovery between cases. That combination dramatically increases burnout risk.
How to Support and Retain Radiologists Amidst a Shortage: 5 Effective Strategies
With burnout on the rise and radiologist shortages straining healthcare systems, keeping your current team supported is just as important as finding new talent.
The good news? There are several proven ways facilities can ease pressure, boost morale, and build a more resilient radiology workforce starting today.

1. Improve work design and workflow
One of the fastest ways to reduce burnout is by reshaping how radiologists work day to day. When case volumes feel endless, and systems don’t support efficient reading, frustration builds fast. But thoughtful changes to workflows, roles, and physical environments can make a big difference.
Balance workloads
- Track case volume trends regularly
- Adjust coverage based on high-volume days or subspecialty bottlenecks
- Set realistic turnaround expectations during peak hours
A major study found that while monthly diagnostic study counts stayed flat from 2009 to 2022, the number of images each radiologist reviewed jumped nearly 400%, which dramatically increased their workload even without a rise in case count. This shows how raw “case count” underestimates real burden, and underscores the need for smarter workflow design.
Offload repetitive and non-clinical tasks
Bring in support roles such as:
- Reading room assistants
- Communication liaisons
- Staff who manage protocol questions and calls
This frees radiologists to focus on interpretation and clinical decisions.
Use tools that prevent unnecessary volume
- Clinical Decision Support (CDS)
- Appropriate Use Criteria (AUC)
- Ordering guidance for referring providers
Cleaner imaging orders reduce low-value scans and cut unnecessary reading time.
Also, invest in ergonomic workstations to help prevent physical strain during long shifts. Long shifts demand:
- Adjustable monitors
- Comfortable seating
- Optimized lighting
- Reduced physical strain
Better ergonomics = fewer fatigue-related issues.
Image-sharing improvements can also help reduce redundant studies. Better access to prior scans and seamless PACS integration means there’s less need to reimage patients. This can ease volume without compromising care.
When done right, workflow optimization improves accuracy, job satisfaction, and patient safety.
2. Improve job satisfaction and flexibility
Burnout often grows in environments where radiologists feel undervalued, overworked, or boxed into rigid schedules. To keep your team engaged and committed, it’s essential to offer both recognition and flexibility, and to create room for meaningful, energizing work.
Here’s how:
- Stay competitive with compensation and benefits. Keep up with current market rates for salary, signing bonuses, CME allowances, and costs related to licensing or board certification.
- Offer flexible scheduling options. Part-time roles, remote reading days, job-sharing, or even four-day workweeks can improve work-life balance without hurting productivity. With teleradiology now common, you’ve got more room to design schedules that serve both staff and the facility.
- Clarify Relative Value Unit (RVU) expectations. RVUs measure physician productivity, but unclear or unrealistic targets are a major stressor. Align RVU goals with case complexity and resources, and avoid incentive structures that punish radiologists for slower reads on complex cases.
- Support professional development. Give radiologists time and support for subspecialty work, research, academic collaboration, or teaching. Variety keeps engagement high and makes the work feel more meaningful.
- Recognize and reward good work. Whether it’s peer shoutouts, leadership kudos, or annual awards, frequent recognition matters. Pair it with a culture that promotes mentorship, peer support, and open communication with leadership.
When radiologists feel heard, respected, and supported, they’re far more likely to stay and thrive.
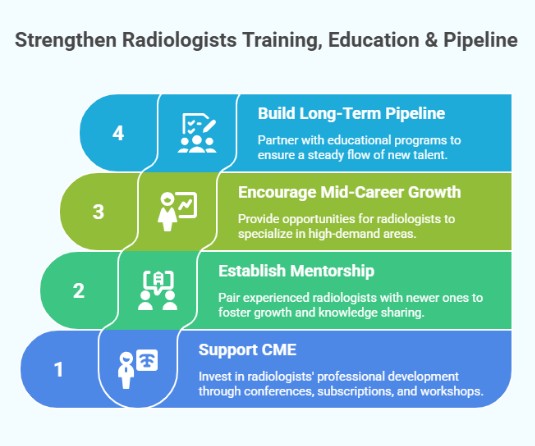
3. Strengthen Radiologists Training, Education & Pipeline
Tackling the radiologist shortage long-term means investing in the next generation of talent and giving your current team room to grow. Facilities that take training seriously build loyalty, increase clinical depth, and stay ahead of changing imaging needs.
Support Continuing Medical Education (CME). CME investment signals that leadership values radiologists beyond day-to-day workload. This can include:
- Reimbursement for conference registration
- Travel support for specialty meetings
- Journal subscriptions and online courses
- Internal workshops or protected learning time
During staffing strain, CME may feel optional, but it’s one of the clearest ways to show commitment to professional growth.
Set up structured mentorship programs that span across seniority levels. Pair newer radiologists or residents with experienced staff to build confidence and encourage knowledge-sharing.
A 2023-2024 review of mentorship ecosystems in healthcare found that mentoring and support programs are linked to increased job satisfaction, less burnout, and reduced turnover (i.e., better retention) among imaging and radiography professionals.
Encourage mid-career radiologists to grow, particularly in high-demand areas like breast imaging, interventional radiology, or nuclear medicine. You can support that by creating in-house learning pathways or partnering with educational institutions to offer discounted or flexible certification options.
Don't overlook the importance of long-term pipeline building. Pipeline strategies include:
- Partnering with residency and fellowship programs
- Supporting residency expansion when feasible
- Offering rotations, electives, and shadowing opportunities
- Exploring combined fellowship-residency models to streamline readiness
A strong pipeline also helps current staff. When radiologists see that help is on the horizon, that the team is growing, and the leadership is planning ahead, it reduces stress and builds confidence in the organization.
4. Expand Staffing Capacity With Flexible Models (Short-Term and Remote Options)
Because the radiologist shortage isn’t going away overnight, healthcare facilities need to get creative. Tapping into flexible staffing and remote options to keep up with demand while giving permanent staff some breathing room.
About 69% of radiologists in 2023 said their organization was understaffed (up from 67% the prior year), while only 23% felt their workplace was fully staffed. This gap is forcing departments to stretch existing radiologists thin, but flexible staffing models offer a way out.
Here are several approaches worth considering:
Short‑Term Workforce Boosters
- Use retired radiologists for per‑diem or seasonal shifts. Many retired docs are willing to do occasional reads, which makes them a valuable pool when staffing is tight.
- Encourage part-time radiologists to take on one extra monthly shift. Sometimes a small commitment can make a big difference.
- Use fellowship‑trained physicians who have completed residency but may not yet be in full-time roles
- Recruit international radiologists through alternate pathways (where credentialing allows), especially when local supply is tight
- Add seasonal or surge‑capacity workers during predictable high-demand periods (e.g., flu seasons, screening drives)
- Make use of radiology extenders like advanced sonographers or radiology‑trained assistants (RRAs) for non-interpretive or lower-complexity tasks (under radiologist supervision)
- Encourage internal or private-practice moonlighting arrangements to cover occasional gaps without long-term hire commitments
Remote and Flexible Coverage Models
- Use locum tenens radiologists for immediate coverage gaps. These could be due to leave, sudden departures, or peak volume periods.
- Implement teleradiology for nights, weekends, and high-volume periods. This allows radiologists to read from remote hubs, which reduces local staffing pressure and expands coverage hours.
- Offer remote reading options as part of regular schedule flexibility, which can help with burnout reduction and broaden the talent pool beyond geographical constraints.
- Use subspecialists outside your local market. This is especially useful for low-volume but high-complexity modalities like nuclear medicine, interventional radiology, and advanced CT/MRI, where local supply is scarce.
These flexible staffing solutions can relieve overtime pressure, reduce backlog, and keep diagnostic services running smoothly even when permanent staffing is strained.
That’s where partners like AAG Health come in. We offer rapid locum tenens and teleradiology support to help facilities manage peak demand, cover gaps, and reduce burnout risk while keeping imaging services running smoothly.
5. Create an integrated retention‑and‑recruitment plan
Solving the radiologist shortage is about aligning recruitment with retention so the people you bring in stay, thrive, and contribute long term. That requires coordination across HR, recruiting, leadership, and clinical operations.
Start by getting HR and recruiting teams fully aligned. Define clear roles and handoffs, from sourcing and interviewing to onboarding and support. Your onboarding process should immerse new radiologists in your culture, values, and support systems from day one.
Next, use data to monitor the health of your workforce. Track signals early so stress doesn’t turn into attrition. Helpful metrics include:
- Satisfaction and burnout-risk surveys
- Turnover patterns
- Sick-day spikes
- RVU or productivity shifts
- Reading error trends
These data points help leadership intervene before problems escalate.
Executive buy-in is critical. Department chairs and hospital leadership must understand that the radiologist shortage is a workforce crisis with direct patient care implications. That means dedicating real resources to retention, flexible staffing, and culture-building.
Finally, consider partnering with a staffing firm to serve as a shock absorber when internal resources are stretched thin. This gives you a scalable backup plan when coverage is urgently needed or when permanent hiring lags.
AAG Health fits naturally into this model. By combining advanced sourcing tools, national reach, and a consultative approach, we help you build more resilient radiology departments. Whether it’s short-term locums or a long-term recruitment strategy, we help clients reduce churn, protect continuity of care, and avoid burning out the team that’s already in place.
How to Support and Retain Radiologists Amidst a Shortage: Implementation Roadmap
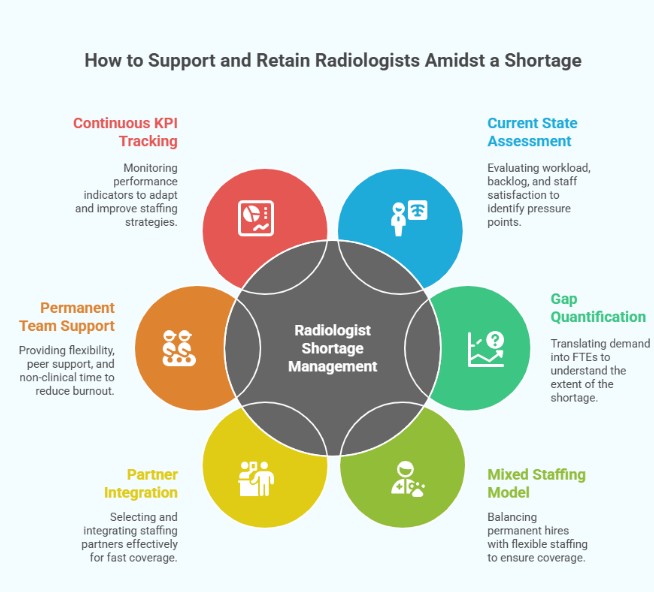
Here’s a practical, step‑by‑step roadmap your facility or health system can follow. It combines retention, smart staffing, and strategic partner support to manage a radiologist shortage sustainably.
Step 1: Assess the current state
Start with a baseline audit where you measure workload per radiologist:
- Cases/day or imaging volumes
- Backlog volumes
- Average turnaround times (TAT)
- Ongoing wait lists
- Staff sick‑leave
- Leave‑of‑absence rates
- Turnover history
- Job‑satisfaction or burnout indicators (via pulse‑surveys or check‑ins)
Then, document every pressure point. These are subspecialty gaps, peak demand times (nights, weekends, seasonal surges), and support‑staff shortages. This honest snapshot helps make the case to leadership, HR, and staffing partners about exactly how big your gap is.
Step 2: Quantify the gap
Translate the backlog and demand data into “full‑time equivalents” (FTEs) you’re short. For example, if the current workload requires 10 radiologists but you only have 7, you have a 3‑FTE gap.
Remember to factor in expected growth in the form of rising imaging orders, aging population, increased chronic‑disease burden, and any planned expansion of services or hours. Map out when and where demand peaks, for example, nights, weekends, subspecialty reads, and surge events, so you know exactly when coverage is most critical.
Step 3: Develop a mixed staffing model: permanent hires plus locum/teleradiology coverage
Use your gap analysis to determine how many permanent hires you need versus how many roles are better served by flexible staffing (locum, part‑time, and remote).
Design a hybrid model made up of a core team of permanent radiologists and a flex pool to cover coverage gaps, surges, leave, or unpredictable demand.
This mixed model balances stability (permanent staff) with flexibility (locum/teleradiology), which reduces burnout and avoids chronic overload.
Step 4: Choose the right partner and integrate them smartly
When you need fast coverage, recruit from a staffing firm that specializes in radiology. They should have a deep, responsive candidate pool and understand clinical requirements.
Make sure to define scope and roles clearly: on‑site vs remote, subspecialty vs general reads, scheduling, communication, quality oversight, and credentialing and onboarding protocols.
Maintain transparency with your permanent team and make it clear to them that flex staff are there to support the department, not replace it.
Step 5: Support your permanent team
Use schedule redesign (for example, rotating shifts, predictable on‑call patterns, remote reading days, and part‑time or job‑share options) to give radiologists more control over their workloads and work‑life balance.
Encourage peer support. This could mean regular team huddles, peer‑review sessions, mentorship, and even informal check‑ins. Building community reduces isolation and stress.
Offer non‑clinical time when possible, like protected time for education, research, subspecialty training, or administrative tasks, so radiologists don’t always feel on the treadmill of reading.
Step 6: Continuously track KPIs and iterate
Pay close attention to key performance indicators (KPIs) such as:
- Turnaround time (TAT)
- Backlog volume
- Number of unread studies
- Open shifts filled by locum/telestaff
- Staff turnover rate,
- Job‑satisfaction survey results
- Burnout metrics
Hold regular monthly or quarterly reviews to see how your mixed staffing model is working, where pressure points remain, and whether you need to adjust coverage, hiring, or workflows. Use feedback loops where you engage staff and leadership to adapt staffing strategy, improve onboarding, address bottlenecks, and maintain morale.
Strengthen Your Radiology Team with AAG Health
The radiologist shortage is a full-blown care crisis, and burnout is accelerating the breakdown. Facilities that want to stay ahead need a plan that supports their people and flexes with demand.
If you’re facing rising imaging backlogs, struggling to recruit subspecialists, or watching burnout spread across your team, AAG Health can help you steady the ship. We work with hospitals and imaging centers nationwide to strengthen coverage, fill critical gaps, and create staffing strategies that reduce pressure on your core team.
Whether you need temporary locum support, long-term recruitment, or a flexible hybrid model with teleradiology, we help build radiology departments that can withstand today’s challenges without compromising care.
Get in touch with us to take the pressure off your imaging team today.
FAQs
What is causing the radiologist shortage?
The radiologist shortage is fueled by a combination of rising imaging demand and an aging radiologist workforce. Even with advances in artificial intelligence, the current growth in diagnostic imaging far outpaces the available radiology workforce, especially in high-demand areas of diagnostic radiology.
How does radiologist burnout affect patient care and facility operations?
Burnout reduces productivity, slows turnaround times, and increases error risk, all of which directly impact patient care and operational flow. In the face of a radiology workforce shortage, facilities stretched too thin often see higher attrition rates and heavier reliance on overworked diagnostic radiologists, which artificial intelligence tools alone can’t solve.
What are locum tenens radiologists, and how do they differ from permanent radiologists?
Locum tenens radiologists are fully licensed medical professionals who provide short-term coverage during staffing gaps caused by the ongoing radiologist shortage. Unlike permanent radiologists, they offer flexible support across settings. This helps maintain continuity in diagnostic radiology services while healthcare systems navigate both workforce constraints and changing tools like artificial intelligence.
When should a healthcare facility consider teleradiology as part of its staffing strategy?
Teleradiology is ideal for covering night shifts, weekend backlogs, or subspecialty reads, especially when local talent is limited or burnout risk is rising.
What retention strategies are most effective for radiologists?
Flexible scheduling, fair RVU targets, recognition, growth opportunities, strong onboarding, and a supportive culture all contribute to higher retention.
How does AAG Health’s locum tenens service work for radiology departments?
AAG Health provides board-certified radiologists to cover short-term, long-term, or urgent staffing gaps. We handle sourcing, credentialing, licensing, scheduling, travel, malpractice coverage, and onboarding. Your team gets fully cleared radiologists who integrate quickly with your workflows, protocols, and systems, so patient care stays uninterrupted while your department stabilizes.
What types of radiologists can AAG Health help recruit?
We recruit a wide range of board-certified radiologists, including general diagnostic readers and subspecialists in neuroradiology, MSK, breast imaging, body imaging, emergency radiology, pediatric imaging, nuclear medicine, and interventional radiology. Our network includes onsite, hybrid, and tele-ready radiologists who can start within days based on your clinical needs.
How does AAG Health integrate locum/teleradiology coverage with a facility’s permanent staffing plan?
AAG Health builds coverage around your existing team rather than replacing it. We review your current staffing structure, volume trends, and subspecialty gaps, then layer in locum or teleradiology support where it adds stability. This approach reduces burnout, protects turnaround times, and provides flexible coverage while you continue recruiting for permanent roles.

