Hiring a Physician Assistant means finding someone who can step in, sync with your team, and handle the real-life chaos of modern healthcare. With staffing shortages and burnout still hitting hard, you can’t afford a misfire.
The pressure is real. McKinsey reports that 84% of healthcare organizations are struggling with persistent clinical staffing gaps, especially in support roles like PAs and NPs. At the same time, demand for PAs keeps rising fast, with the field expected to grow nearly 28% by 2033.
So how do you hire a PA who doesn’t just look good on paper but actually sticks around, fits your culture, and improves the way your clinic or hospital runs?
That’s what this guide is for. Read on to learn:
- How to strike the right balance between autonomy and oversight
- Ways to actually test EMR fluency
- How to spot early signs that a PA might burn out in high-pressure or shift-heavy settings
- What to ask to uncover cultural fit, adaptability, and teamwork skills
- Why your org’s reputation might be turning great candidates away (and what to do about it)
Let’s get started.
10 Tips to Hire the Right PA
Without further ado, let’s move right into the physician recruiting tactics that will increase your team with the right PA.
1. Balance your physician assistant’s autonomy with oversight
Finding the right mix of autonomy and oversight is critical. A PA with too much independence may overstep clinical boundaries; too little, and they become a bottleneck. The ideal candidate works confidently within defined limits and knows when to escalate.
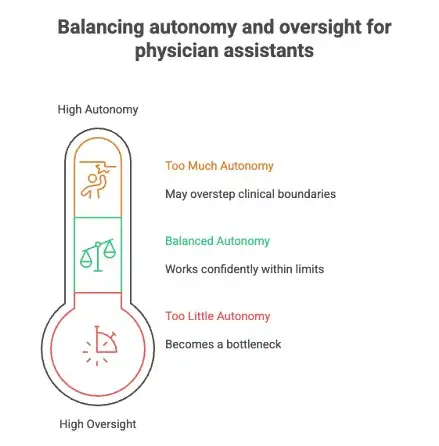
Why it matters: Rearch shows that experienced PAs spend less than 10% of their time consulting with physicians. In primary care, once PAs have over five years of experience, their need for supervision drops significantly, as they take on routine decision-making independently.
What to ask in interviews: Use real-world clinical scenarios. For example: “Describe a time when you handled a patient case without immediate physician oversight. How did you decide whether to manage it yourself or consult?” A strong candidate response demonstrates good judgment, awareness of their limitations, and respect for escalation protocols.
What to clarify during hiring: Clarify which tasks require physician sign-off and which can be performed independently. Set explicit escalation triggers. Establish how feedback and reflection will happen, for example, regular reviews of near‑miss decisions or consult cases.
The impact on your team: When handled correctly, autonomy improves workflow efficiency and provider satisfaction. It reduces role creep, supports retention (especially among experienced PAs), and helps prevent frustration on both sides. Remember that physicians want capable support, and PAs want trust and clarity.
2. Test your Physician Assistant for EMR fluency, not just comfort
Nearly every PA candidate claims they’re “good with EMRs.” But learning or switching to a clunky or legacy system is a different story. You’ll learn far more by testing their real-world ability upfront.
Why it's vital: Usability scores for Electronic Medical Records (EMR) systems remain disappointing across the board. One JAMA Network Open survey of over 2,000 family physicians found only about 27% were “very satisfied” with their EMR, while almost 10% were “very dissatisfied.” Higher usability scores were strongly linked to less burnout and higher job satisfaction.
Another study at Massachusetts General and Brigham and Women’s Hospital tracked 307 primary care physicians across 31 clinics and found a median EHR time of 36.2 minutes per visit, which included inbox management and after-hours charting. That’s over half an hour added on top of face-to-face care.
What to do in your hiring process: Ask candidates to walk through your EMR interface, or a close analog, during the interview. Give them a few typical tasks such as entering a note, searching for medication history, or handling an inbox message. Take note of how they navigate, how quickly they adapt, and whether they ask smart, clarifying questions.
What to communicate clearly: Explain the quirks of your EMR (billing workarounds, template navigation, flag-heavy alert systems). Let them know in advance how much time you expect documentation to take per patient and what efficiency tools (templates, scribes, voice dictation) are in place.
Why this matters for your team: PAs who can’t handle the EMR environment slow down workflows and contribute to documentation backlogs. But those who are fluent and proactive about optimization reduce physician burden, improve accuracy, and keep chart completion on track.
The image below highlights what’s at stake here:

3. Assess flexibility for odd hours and shift-based work
In urgent care or facilities that operate around the clock, hiring a PA who adapts to rotating shifts, weekend coverage, or lone-provider shifts is something you can’t avoid. Instead of asking generically, “Are you okay with evenings?” it's much more revealing to explore real experiences managing unpredictability.
Why it matters: Shift work isn’t just inconvenient; it carries proven risks. According to the U.S. National Institute for Occupational Safety and Health (NIOSH), the risk of accidents or injuries is roughly 18% higher during evening shifts and 30% higher during night shifts, compared to standard day shifts.
NIOSH also reports that working 10‑hour shifts increases injury risk by 13%, and 12‑hour shifts raise it by 28%, compared to traditional 8‑hour workdays.
Limiting the number of hours worked per week can be a worthwhile investment:
How to dive into this during hiring: Ask focused situational questions like: “Describe a time you worked weekends or nights. How did you manage fatigue, scheduling changes, or patient load when working solo?”
Look for candidates who demonstrate experience pacing themselves, prioritizing self-care, and maintaining attention under pressure.
What you should clarify in the hiring agreement: Define expectations up front: what constitutes evening, overnight, weekend, and holiday shifts? Are schedules rotating or fixed? How much notice will they receive? Will backup support (e.g., cross-coverage plan) be available? Outline any shift differential pay or wellness resources provided.
Why this matters for sustainability: Physician shortages affect the healthcare workforce. Finding PAs with genuine resilience and flexibility reduces burnout risks and ensures continuity for patients. Those who handle irregular hours well tend to integrate more quickly, maintain better performance under stress, and endure long-term in shift-heavy settings.
4. Watch for “bouncer syndrome” in high-volume clinics
When PAs work in high‑throughput settings, the tendency to "rush patients through" can mimic the fast-paced line management of a nightclub bouncer. That may increase volume, but it usually leads to clinical errors, burnout, and poor patient experience.
Why it matters: High workload and time pressure directly undermine care quality. A qualitative study of GPs in the UK found over‑burdened clinicians commonly rushed diagnoses and treatment decisions, increasing the risk of misdiagnosis and patient harm. Clinicians described how workload forced shortcuts, sometimes compromising safety and thoroughness.
Other systematic reviews show burnout among healthcare staff is associated with a 26.1-71.7% higher risk of adverse patient outcomes, due in part to fatigue and cognitive overload.
What to explore in interviews: Instead of asking general questions like “How do you handle pressure?” go deeper: “Describe a time you were under high patient volume. How did you ensure quality care without cutting corners?”
Look for candidates who can talk through their process: triaging appropriately, slowing down with complex patients, and reflecting afterward on what they could have done differently.
What to communicate during hiring: Make it clear how your clinic manages volume peaks. Share protocols around triage, documentation time per patient, and support systems, like floating staff or scheduled breaks, to prevent overload.
Why this matters for patient safety and provider health: When PAs automatically accelerate throughput at the expense of quality, both patients and providers suffer. But those who maintain discipline under stress by balancing efficiency with empathy help reduce error rates, lower burnout risk, and support strong patient satisfaction scores.
5. Check their comfort with diverse patient populations
Healthcare settings serve everyone, from trauma survivors and limited‑English‑proficiency patients to those facing systemic biases. The right PA is clinically sharp but also culturally aware and communicative.
Why it matters: A 2022 survey by the NHS Race and Health Observatory (UK) revealed that among ethnic minority primary care patients, 38% of Asian respondents and 49% of Black respondents reported experiences of discrimination that eroded trust and engagement with healthcare services. Research indicates dissatisfaction isn’t from patient factors but service-related shortcomings like ease of using the GP website and perceived care attitude.
Here’s an illustration of implicit bias in healthcare based on a real case study:
What to ask in interviews: Pose questions such as: “Tell me about working with diverse or underserved populations. How did you handle language barriers, cultural differences, or trauma-informed care?”
Look for responses that show empathy, cultural self-awareness, and concrete examples of using interpreters, adjusting communication style, or recognizing emotional context.
What to clarify during hiring:
Set expectations around:
- The types of populations they'll serve: immigrants, non‑English speakers, behavioral health, etc.
- Available resources like interpreter services, cultural competency training, or trauma-informed protocols.
- How the facility manages equity and inclusion in patient care.
Why this matters for patient experience and outcomes: Patients from minority groups consistently report lower satisfaction when care isn’t culturally or linguistically aligned, but this is a gap that provider competence can help close. PAs who can connect across cultures and empathize build trust, boost adherence, and improve both satisfaction and clinical outcomes.
Pro tip: Use a data-driven approach to healthcare hiring to make sure you get the right people onboard.
6. Clarify your expectations for role fluidity
In many healthcare settings, Physician Assistants juggle a mix of clinical duties, administrative tasks, and patient counseling… sometimes within the same hour.
Other facilities prefer rigid, discipline-specific schedules. It’s essential to be transparent about what a typical day really looks like at your facility and then assess whether a candidate’s past experience and expectations align.
Here are some of the roles and responsibilities that a PA can take:
Why it matters: Research highlights that PA deployment is rarely linear. In primary care, a study of PA integration in Canada found that roles are highly adaptable. PAs frequently change responsibilities based on clinical demand and workflow needs, indicating a need for flexibility on both sides.
A broader literature review commissioned by the UK Department of Health and Social Care noted considerable variation in PA roles across settings. In many cases, PAs take on extra administrative and care coordination tasks in response to local system needs—even when those aren’t part of their formal job description.
What to explore in interviews:
Ask questions like: “Can you walk me through a day where you switched between patient assessments, documentation, patient education, or administrative follow-ups?”
Look for candidates who:
- Demonstrate experience in pivoting between tasks seamlessly
- Talk confidently about triaging workload
- Know how to manage their priorities when the day shifts unexpectedly.
What to communicate during hiring:
Clearly define:
- The extent of non-clinical work (scheduling, charting, follow-ups)
- Whether procedural, administrative, and counseling duties are all part of the daily mix
- The expected pace of change and how often responsibilities evolve
- Any support systems in place (e.g., scribes, team-based handoffs, admin backup)
Why this matters for performance and retention: Aligning expectations early prevents frustration and frustration-driven turnover. PAs who adapt well to varying roles help fill gaps, reduce bottlenecks, and often drive longer-term retention because they feel trusted and impactful instead of siloed or sidelined.
7. Gauge their comfort with institutional hierarchy
Hospitals, especially large academic or public centers, come with multiple layers: department heads, administrators, interdisciplinary committees, and shifting priorities. Some PAs thrive in that structure. Others hit a wall quickly. During interviews, dive into how deeply they’ve worked within complex systems.
The image below highlights this difference:

Why it matters: Healthcare systems with strong alignment between staff and leadership see direct benefits. A BMJ Open study of over 63,000 NHS staff found that higher leader support and greater influence over decision-making significantly reduced perceived work pressure, and that pressure was directly tied to lower patient satisfaction. In essence, a PA’s ability to navigate hospital politics and feel heard matters for both team cohesion and patient care.
What to ask in interviews:
Rather than vague questions about collaboration, probe with:
“Tell me about working in a setting where decisions happened above your level, like changes in policy or protocol. How did you make yourself heard? What approach helped you navigate that?”
Strong candidates share stories about collaboration, escalation, and constructive feedback instead of closed-door frustration.
What to clarify during hiring: Be explicit about your facility’s decision-making structure. How much autonomy do PAs have in patient care, training, or procedure selection? Who approves protocol changes? What support systems exist for escalating workflow issues or case reviews?
Why this matters for long-term success: A PA who respects hierarchy, but knows how to ‘push upward’ when necessary, adapts to institutional complexity. They help build mutual trust, reduce confusion over responsibilities, and thrive in environments that reward initiative.
8. Explore how they’ve handled medical errors or near-misses
Mistakes happen: it’s how a PA responds that really counts. You want someone who owns their actions, learns from them, and communicates clearly. Their answer here reveals character: integrity, critical thinking, and emotional maturity.
Here’s how healthcare facilities should view PA mistakes:
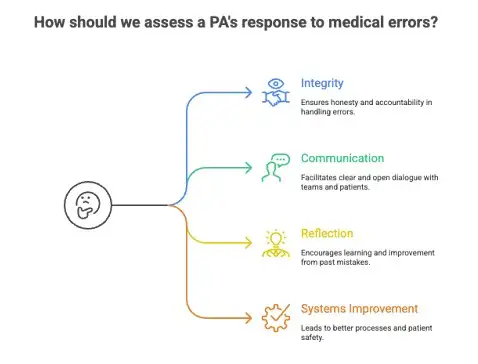
Why it matters: In a pilot program using an anonymous near-miss reporting system across seven diverse primary care clinics, over 630 near-miss events were reported in nine months which led to 32 quality-improvement initiatives based directly on those findings.
These findings show how even minor incidents can surface real system gaps, and that learning from them requires transparency and active reflection.
What to ask in interviews:
Frame questions like: “Tell me about a medical error or near miss you were involved in. How did you handle the situation, communicate with the team or patient, and what did you change afterward?”
Strong responses include these elements: owning the issue, clear communication, thoughtful reflection, and systems improvement.
What to clarify during hiring: Describe how your facility handles errors and near misses. Do you have a non-punitive reporting system? Is feedback timely? Is there a formal review process or culture of safety that supports open communication? Setting that tone up front ensures candidates know what’s expected.
Why it matters for your institution: PAs who handle mistakes well help cultivate a just culture, where learning and improvement are prioritized over blame. That leads to fewer repeat errors, greater trust among clinical teams, and stronger patient safety outcomes.
9. Look for experience in multidisciplinary collaboration
In clinical environments with dietitians, social workers, case managers, and specialists all contributing to care, a PA who knows how to plug into that web makes a huge difference. During interviews, ask for specific teamwork examples and how they kept the patient at the centre of complex care coordination.
Why it matters: A comprehensive review of multidisciplinary efforts in primary care (34 systematic reviews across multiple studies) found that interprofessional collaboration is associated with improvements in clinical markers (like HbA1c and blood pressure), better medication outcomes, streamlined care processes, and higher patient satisfaction.
Another recent meta‑analysis of multidisciplinary teams in non‑hospital settings reported measurable improvements in patient-reported outcomes for chronic disease patients, especially around coordination of care and overall satisfaction.
What to ask in interviews: Ask questions such as: “Tell me about a case where you worked with multiple professionals like dietitians, social workers, or specialists, to manage a patient's care plan. How did you help keep things coordinated?”
Look for candidates who discuss communication strategies, role clarity, and how they structured team interactions to keep the patient supported at every step.
Here are other questions to consider:
What to communicate during hiring:
Be transparent about the collaborative environment:
- Types of allied health professionals involved in care
- Tools used for coordination (team round‑ups, shared care plans)
- Expectations for communication and handoffs across disciplines
Why this matters for outcomes and cohesion: PAs who are comfortable navigating multi-role teams support better outcomes across metrics and help contribute to stronger team cohesion. Whether it’s reducing errors, smoothing discharge plans, or elevating patient experience, interdisciplinary collaboration is a proven quality driver, and PAs who thrive in it are high-impact hires.
10. Don’t overlook your facility’s brand and rep
Healthcare is a small world, which means your organization's reputation matters. If candidates hear about burnout culture or poor onboarding, you might lose strong applicants before you even begin. To improve hiring and retention, you should try to understand how people perceive your facility both internally and publicly.
Why it matters: Turnover is expensive, and a damaged reputation drives it. Industry experts estimate that the total cost of replacing staff in healthcare can reach 150% of that employee’s annual salary. For instance, replacing a bedside nurse might cost over $46,000, and hospitals often lose $5 to $9 million a year due to turnover alone.
Meanwhile, healthcare facilities with strong online reputation scores generate substantially more patient interest. Organizations with robust scores on Google My Business see up to 1,290% more interactions (clicks, calls, website visits) from prospective patients. That effect translates into real competitive advantage in attracting both patients and top talent.
What to ask in interviews: Explore the candidate’s perspective and your past staff experience: “What have you heard about our organization from peers or former employees? What stood out, good or bad?”
Also consider exit interviews with departing PAs: “Why did you leave? What was your onboarding like? What could have made you stay?”
What to clarify in hiring:
Be transparent about your culture and processes:
- Explain how you onboard and mentor new hires.
- Highlight support for well-being, career growth, and feedback loops.
- Share any recent improvements like restructuring workloads, better staffing, or revamping training to show you're listening and evolving.
Why this step matters long-term: Understanding reputation helps you fix systemic issues before they become recruiting problems. It improves retention, reduces costly turnover, and reinforces a positive employer brand. When your facility is known for a supportive culture and good systems, it attracts PAs who stay and perform for the long haul.
Red Flags That Signal a Bad PA Fit (Before You Hire Them)
Spotting the wrong hire early is just as important as recognizing the right one. Here are a few subtle red flags that should prompt deeper follow-up questions during the hiring process, each tied to one of the challenges we covered earlier.

If they say:
“I’ve worked mostly solo.”
Ask: “How do you decide when it’s time to escalate or consult?”
Why: They might struggle with clinical boundaries or overestimate their autonomy in team-based care.
“I prefer to stick to a strict routine.”
Ask: “Can you tell me about a time your role shifted unexpectedly mid-day?”
Why: May not adapt well in dynamic or high-shift-volume environments.
“I’m very fast with patients, I like to keep things moving.”
Ask: “How do you balance efficiency with patient understanding and safety?”
Why: Could point to "bouncer syndrome": rushing at the expense of quality.
“I’ve never really had to use interpreters or work with non-English speakers.”
Ask: “How would you approach a language or cultural barrier in a clinical setting?”
Why: Limited exposure to diverse populations may impact their effectiveness and empathy.
“I’m not sure what others said about me when I left.”
Ask: “If we asked your last supervisor or colleague to describe your collaboration style, what would they say?”
Why: Dodging this question may hint at issues with team dynamics or accountability.
“I haven’t had to handle medical mistakes; those are pretty rare.”
Ask: “What would you do if you caught a documentation or medication error after a patient visit?”
Why: Overconfidence or lack of self-awareness around risk and reflection.
In this video, a medical practice owner walks through a real-life case where a poor physician hire led to severe financial loss, damaged reputation, and operational disruption. It lays out precisely what red flags were missed, from inflated credentials to cultural mismatch.
You will understand the tangible consequences of bad hires and why thorough vetting and structural hiring frameworks are non-negotiable for healthcare organizations.
Final Takeaway: Hire for Fit, Not Just Function
Hiring a Physician Assistant means taking into account chemistry, adaptability, and long-term alignment with how your facility actually runs. The cost of a bad hire in healthcare is clinical, cultural, operational as well as financial.
If your team is feeling the pressure of high turnover, sluggish onboarding, or inconsistent care quality, the fix might not be “more candidates.” It might be better hiring questions, clearer expectations, and a closer look at how your PA role is defined from day one.
Next step:
Before your next round of interviews, pull out two things:
- Your last PA job description
- The feedback from your last departing PA
Compare the story you told with the reality they experienced. That gap is where your hiring strategy needs work.
The best PAs make your team smarter, stronger, and more sustainable. You don’t need more applicants; you need a better strategy.
A solid recruiting partner can make that strategy happen.
At AAG Health, we help healthcare organizations find physicians who are aligned clinically, culturally, and operationally with your team.
How we do it:
- Culture + fit first: We go beyond credentials to ensure every physician we place can adapt to your workflows, values, and patient mission.
- Rigorous vetting: Every candidate is thoroughly screened on experience, licensing, and patient care standards.
- Referral-driven network: Our physician pipeline is built on trusted referrals and established relationships, giving you access to candidates your competitors can’t reach.
- Quality guarantee: We back our placements with a 90‑day replacement policy, so you can hire with confidence.
Ready to strengthen your physician team? Contact us today to discuss your staffing needs and see how we can help you build resilient teams and get better patient outcomes.
FAQ: Hiring the Right PA
What are some common challenges with hiring PAs?
Hiring Physician Assistants, especially for high-demand specialties like Emergency Medicine, Urgent Care, or Occupational Medicine, comes with unique challenges. These include misalignment on autonomy, lack of adaptability to the medical model, poor EMR skills, or limited experience with procedures like wound care and dressing changes. Using a specialized staffing agency or placement service can help avoid mismatches by sourcing candidates with the right clinical and cultural fit.
What does a PA typically do?
PAs provide a wide range of medical care, from diagnosing illnesses and ordering diagnostic tests to assisting in surgery and managing chronic conditions. They work under a physician’s supervision and are trained in the medical model, which prepares them to deliver comprehensive medical services across many settings, including Family Medicine, Emergency Departments, and General Surgery.
Can a PA perform surgery?
PAs in surgical specialties like General Surgery can assist in the OR, perform minor procedures, close incisions, and manage pre- and post-op care. They’re critical members of the healthcare team, especially in high-volume environments where surgical PAs help keep patient flow steady and outcomes on track.
Why hire an NP over a PA?
It depends on the needs of your setting. Nurse Practitioners (NPs) may be a better fit for wellness-focused practices or long-term Family Medicine management, while PAs trained in the medical model often offer broader procedural and acute care flexibility. For high-volume or fast-paced areas like Emergency Medicine or Urgent Care, many facilities lean toward hiring PAs.
How are PAs trained?
PAs undergo rigorous medical education modeled on the training physicians receive. Their programs are shorter than med school but still intensive, covering diagnostics, pharmacology, clinical rotations, and more. This prepares them to work effectively across specialties and adapt quickly to different clinical environments in the United States.
What’s the role of Advanced Practice Providers in staffing solutions?
Advanced Practice Providers (APPs) like PAs and NPs are increasingly central to clinical operations, especially in specialties like Emergency Medicine and Occupational Medicine. A good staffing agency or locum tenens partner can help you match the right APP with the right role, improving patient care while reducing burnout and turnover.
Where can PAs find job opportunities?
There’s strong demand for PAs across the United States in settings like Family Medicine, Urgent Care, and Emergency Departments. Services like PA Solutions and national placement services can help PAs explore both permanent roles and locum tenens contracts, and offer flexibility and access to a wide range of job opportunities.

