Across the U.S., especially in rural towns, inner‑city neighborhoods, and under‑resourced communities, there just aren’t enough healthcare providers to go around. Data from the USDA found that rural areas had only about 5.1 primary care physicians per 10,000 residents, compared with 8.0 per 10,000 in urban areas.
That shortage leaves clinics overburdened, wait times long, and continuity of medical care spotty, which is rough on both patients and providers.
Fortunately, physician assistants can fill this gap. With solid training, flexibility, and the ability to work under supervision or collaborative care models, PAs offer a practical way to expand access.
In this article, we’ll explain why physician assistants make sense for underserved areas, and how a partner like AAG Health can make hiring them fast, smart, and hassle-free.
Who Are Physician Assistants? A Primer
A physician assistant (PA) is a trained, licensed medical provider who works under supervision or as part of a care team. They help deliver patient care where demand outpaces supply.
To become a PA, most candidates start with a bachelor’s degree (for example, in a science or health‑related field), then complete a postgraduate PA program (master’s level). This program combines medical sciences, diagnostic tests, and laboratory tests training, clinical medicine, and supervised clinical rotations across specialties like primary care, emergency medicine, internal medicine, and more.
After that, they pass a national certifying exam (PANCE) to become certified, and then they obtain state licensure.
PA vs. NP vs. MD: What’s the Difference?
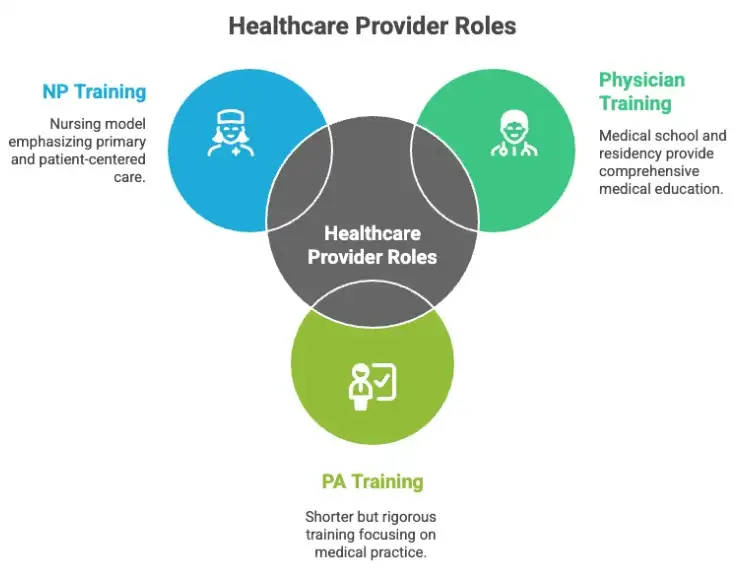
- PAs vs. Physicians (MD/DO): Unlike physicians, PAs don’t go through medical school and residency. Their training is shorter but medically rigorous enough to allow them to take patient histories, perform physical exams, order diagnostic tests, and, under supervision or collaborative care models, help diagnose and treat illness. MDs undergo up to 17 years of training, but have more autonomy, a higher salary, and can do surgery. However, they can’t change specialties as easily as PAs do because it requires completing another residency.
- PAs vs. Nurse Practitioners (NPs): While both PAs and NPs play major roles among healthcare providers, PAs train under a medical model, which means their education emphasizes pathophysiology, diagnostics, and a broad scope across medical disciplines. NPs tend to follow a nursing model, usually with a greater focus on primary care, prevention, chronic care, and patient-centered care (although overlap exists depending on the regulations). Learn more about this difference in our article here.
This flexibility across specialties, settings (rural clinic, community health, urgent care, and mobile units), and types of medical issues makes PAs ideal for underserved or resource‑limited areas.
Quality Care and Cost‑Efficiency
Research supports that adding PAs to care teams doesn’t sacrifice quality. A 2025 review by Nicola Cooper et. al. found that, in many studies, patients treated by PAs reported no difference in satisfaction compared with physicians, and when working under direct supervision, PAs practiced safely and effectively.
Given their training and flexibility, PAs offer a cost‑effective alternative to full-time physicians. This is a big plus for clinics that are operating under tight budgets but need to deliver reliable health care services.
Pro tip: Need to get your PA hired fast? Alpha Apex Group Health’s model delivers resumes in your inbox within 72 hours, and it’s 50-70% more cost-effective than other models.
Why PAs Make Sense for Underserved Areas: Key Benefits
In places where healthcare access is stretched thin, physician assistants are essential. From cutting wait times to expanding care options, PAs bring flexibility, efficiency, and real clinical impact to communities that need it most. Here are some of the ways they make a difference.
Physician Assistants Offer Expanded Access and Reduced Wait Times
When demand outpaces supply, care suffers, and that’s exactly where physician assistants (PAs) shine. By adding PAs to your team, clinics can dramatically expand access, cut patient wait times, and keep care flowing smoothly.
That’s because PAs can handle:
- Routine visits
- Chronic‑disease follow‑ups
- Preventive care
- Common urgent‑care needs
We’ll discuss these tasks in more detail below.
As such, they take a big load off physicians, which frees MDs to focus on complex cases while giving more timely care to patients. In fact, the Nicola Cooper et. al. review above shows that adding PAs to primary‑care teams consistently increases access to care.
One study of clinics that introduced PAs found that many of the extra appointments offered were for “same‑day” or nearly immediate access; PAs handled a broad mix of non‑complex patient visits and effectively kept services moving.
For underserved or rural clinics where physician shortages, long travel times, and under‑resourced infrastructure already hinder access, that boost in capacity can make all the difference.
With a PA on staff, patients are more likely to get care when they need it, which:
- Reduces backlog
- Avoids crisis visits
- Improves overall healthcare continuity
Physician Assistants’ Versatility and Scope: From Primary Care to Urgent Needs
One of the biggest strengths of physician assistants (PAs) is just how flexible they are. They’re not limited to one specialty. Instead, they move fluidly across settings and patient needs, and this makes them ideal for clinics where every day looks different. They’re also great if you’re dealing with a physician shortage.
PAs can help cover:
- Primary care visits (routine checkups, screenings, and chronic disease management)
- Urgent care needs (mild injuries, infections, and same-day visits)
- Preventive health (immunizations, wellness exams, and lifestyle counseling)
- Patient education (medication instructions, care plans, and health coaching)
- Follow-ups for chronic conditions like diabetes, asthma, or hypertension
Their medical training spans multiple disciplines, so they can also step into roles depending on the clinic’s focus and the supervising physician’s scope. That includes:
- Maternal health (prenatal checkups and postpartum care)
- Pediatrics and adolescent care
- Geriatrics (routine management of aging-related health issues)
- Mental health (monitoring mood disorders and coordinating therapy plans)
- Emergency or walk-in care in high-volume clinics
Warning: This is true only if the supervising physician’s scope includes those areas and the PA has relevant training. PAs do not independently provide prenatal care, postpartum care, mental-health management, or pediatric primary care unless allowed by state law, the supervising physician, and the clinic’s scope.
In emergency departments and urgent care settings, studies show that PAs help ease pressure on physicians while maintaining safe, effective care.
In short, a single PA can fill multiple roles and adapt to the clinic’s changing needs. That’s a huge asset in underserved areas where staffing is tight but patient demand is high across a range of medical issues.
Physician Assistants Offer Better Continuity and Retention vs Other Models
When your clinic’s coverage depends on “fly‑in/fly‑out” doctors or short‑term locums, you get flexibility, but it often comes at the cost of continuity, consistency, and long-term community relationships. That’s where PAs, especially when placed through a dedicated staffing firm, really shine.
Why PAs Tend to Bring Better Continuity and Retention
- Unlike traveling physicians or locums who rotate in and out based on assignments, PAs (especially those hired for full-time or long-term placement) are more likely to stay put. That translates into a stable care team, which helps build patient trust and smoother workflows.
- When a PA stays at a clinic for months or years, they get to know the community. They learn about patients’ histories, recurring needs, family backgrounds, and chronic conditions. This kind of continuity improves the patient experience and supports better long-term management of chronic disease, preventive care, and follow-up.
- With locums or flying clinicians, handoffs are frequent and often require catch-up, re-review of patient records, or re-establishing rapport. PAs embedded in the practice avoid that disruption.
- Using PAs for permanent placements can cost less than repeatedly relying on locum/fly‑in physicians. This reduces recruitment, credentialing, and turnover costs while maintaining care coverage.
- Because PAs usually train broadly (in the specialties we mentioned above: primary care, emergency medicine, chronic care, and so on), they can cover many needs, from routine visits to emergencies, without hiring a rotating cast of specialists or locums.
Especially in primary care settings, the presence of PAs contributes significantly to rural health coverage. PAs can help offset declining physician availability without sacrificing access or quality.
Cost and Resource Efficiency
When budgets are tight (as they usually are in underserved areas), every dollar counts. That’s one of the biggest wins of using physician assistants (PAs): they deliver high‑quality medical care at a lower cost than physicians. Because of this, clinics can stretch limited resources further while maintaining (or even improving) service coverage.
- A comprehensive 2021 systematic review of international evidence comparing PAs and physicians found that, in the majority of studies, “labor and resource costs were lower when the PA delivered the care” while maintaining comparable or better outcomes.
- Another analysis showed that for many common conditions, total cost per patient visit was lower under PAs than under physicians, without increasing return‑visit rates or lowering care quality.
According to the Bureau of Labor Statistics, the current median annual salary for a physician assistant is $133,260. By comparison, a physician earns at least $239,200 per year.
For underserved clinics, that translates into tangible benefits:
- More patient visits per dollar spent. With lower labor costs, a PA can see as many patients (or close to as many) as a physician, especially for routine, preventive, or follow‑up care.
- Broader service coverage without overspending. Clinics can afford to staff for a wider range of services (like chronic‑disease management, preventive care, and urgent visits) without needing a full complement of specialists.
- Reduced pressure on staffing budgets. PAs can act as a cost‑effective backbone for medical care, which frees up funds for other critical needs like equipment, outreach, community health programs, or facility improvements.
If your clinic is juggling limited resources, unpredictable demand, and a wide range of patient‑care needs, PAs offer a financially sustainable way to deliver reliable, high‑quality medical services without constantly overshooting budgets.
The Challenges of Hiring Physician Assistants: What to Watch Out For & How to Overcome Them
Bringing physician assistants (PAs) into your clinic can be a game-changer, but it’s not without challenges. From compliance issues to hiring roadblocks, many underserved clinics hesitate because they’re not sure how to navigate the logistics. Here’s what to look out for and how to get ahead of it.
Physician Assistants Regulatory and Scope-of-Practice Limitations
In some states, PAs have broader practice authority. In others, their role is more restricted, and this is tied to detailed oversight or collaborative agreements with a supervising physician. That variation can make adoption tricky, especially for clinics new to the PA model.
This is where many organizations hit pause. Sorting out legal language, supervision rules, and credentialing forms feels like a mountain of paperwork. But it doesn’t have to be.
Credentialing 101: What HR Teams Should Know:
- Licensing: PAs must be certified by the National Commission on Certification of Physician Assistants (NCCPA) and licensed by the state medical board
- Supervisory requirements: Most states require a named supervising physician or a collaboration agreement. Some limit how many PAs a physician can oversee.
- Collaborative agreements: These spell out how the PA and physician work together. It should specify who approves treatment plans, prescribes meds, handles oversight, and so on.
- Malpractice coverage: Clinics must make sure both the PA and supervising provider are covered. That can be part of a broader policy or purchased separately.
- State-by-state rules: Scope of practice, prescribing authority, and supervision models differ across the U.S., and staying compliant is essential to avoid risk or disciplinary action.
This is worth taking seriously. Compliance mistakes can lead to delayed care, patient safety issues, or even penalties.
Physician Assistants’ Hiring and Staffing Barriers: Why It’s Hard to Fill PA Roles on Your Own
Underserved clinics face major recruiting headwinds, like:
- Talent is scarce. Many PAs prefer urban or suburban settings, which leaves rural or resource-limited communities with fewer options.
- You’re competing with big players. Large health systems can offer more in terms of pay, perks, and upward mobility.
- It’s time-intensive. Finding the right PA takes time, from outreach to credentialing to onboarding, and most HR teams are already stretched thin.
Integration & Onboarding: Fitting PAs Into Existing Care Teams
Even the best hire won’t succeed without the right support. For a PA to thrive in a new clinic, they need:
- A clear role and expectations
- Defined workflows (to show them who handles what and how supervision works)
- Tech access (like EHR logins, charting systems, and diagnostic platforms)
- A strong onboarding plan
- Community and team buy-in
Retention, Burnout, and Funding Constraints
Long-term staffing in underserved areas is hard for a few reasons. First, funding fluctuates, and support structures can be thin. Besides, healthcare staffing statistics show that burnout is a real problem for providers juggling high patient loads with limited resources.
Without a solid plan, clinics risk high turnover, which disrupts care, hurts patient trust, and drives up costs.
Practical Steps for HR Teams & Recruiters: How to Start Hiring Physician Assistants for Underserved Clinics
Ready to bring a physician assistant on board? Here’s a step-by-step guide to help you move from idea to implementation.

Evaluate Your Clinic’s Needs
Start by mapping out patient volume, current service gaps, and specialties you’re struggling to cover. Are wait times growing? Are chronic care needs slipping through the cracks? This helps define what kind of PA support you actually need.
Review Your State’s Scope-Of-Practice Rules
Know what PAs can and can’t do in your area. Look at supervision requirements, prescriptive authority, patient ratios, and more. This helps you shape a role that’s compliant from the start.
Decide How You’ll Hire
Direct hire or agency placement? If you need speed, credentialing support, and a vetted shortlist, a staffing partner can take a lot off your plate.
Define the Role
Clarify schedule, scope, clinical responsibilities, supervision model, and expectations. (If you’re working with a recruiter, they can help build this out.)
Plan for Onboarding and Integration
Integrate PAs into your clinical team, set up EHR access, clarify workflows, and get buy-in from physicians and staff.
Track Quality and Outcomes
Set clear goals: Are patient wait times going down? Are chronic conditions being followed up more consistently? Measure impact early and often.
Make your Clinic PA-Friendly
Offer competitive compensation, flexible scheduling, support for continuing education, and community connection. PAs want to feel valued, and they’ll stay longer when they do.
Treat PAs as Core Team Members
Mid-level providers thrive when they’re empowered to lead care, rather than just fill in when someone’s out. Build a culture that respects their training, scope, and contribution.
How AAG Health Helps You Close the Gap One PA at a Time
Underserved communities need practical, scalable solutions. Physician assistants offer flexible, high-quality care that expands access, lightens the load on physicians, and fits within limited budgets.
And while hiring a PA can seem daunting, the right support makes all the difference. A partner like AAG Health helps you move faster, avoid compliance pitfalls, and find the right fit the first time.
Ready to bring in a PA? Get in touch with us to learn more about finding and placing the best talent.
FAQs
What education requirements must a physician assistant meet?
PAs must complete a bachelor’s degree, followed by a master’s degree from an accredited medical training program that includes supervised clinical training.
How do PA education programs compare to medical school?
While shorter than a full medical school curriculum, PA programs still cover core clinical specialties, surgical disciplines, and medical histories, with rigorous clinical experience requirements.
What kind of procedures can PAs perform?
Depending on the state and setting, PAs may assist in or perform surgical procedures, manage patients in a medical office, and follow clinical guidelines for diagnostics and treatment.
What exam do PAs need to pass before practicing?
After the successful completion of their education, PAs must pass a qualifying exam and meet all administrative rules set by their state licensing board.
Are PAs considered physician associates or healthcare professionals?
The terms physician associates and healthcare professionals are both used to describe PAs. This reflects their central role in improving health outcomes.
How can I evaluate if a PA candidate meets clinical and education standards?
Work with a recruiter who verifies education programs, clinical experience, and successful completion of all certification steps, including licensing and the qualifying exam.
What role does AAG Health play in ensuring compliance with administrative rules?
AAG Health helps you navigate state-level administrative rules, from verifying licensure to confirming clinical specialties, supervision models, and scope-of-practice documentation.
How do I define a PA role that aligns with our needs?
Use real data to tailor the role based on your clinic’s patient load, whether you need help with medical office flow, surgical procedures, or specific clinical guidelines.

