The healthcare industry’s facing serious pressure. Patient volume continues to climb, but many facilities struggle to maintain enough qualified providers to keep up with demand.
That’s where physician assistants (PAs) come in. These highly trained, flexible healthcare professionals help facilities manage capacity, improve patient outcomes, and ease provider burnout.
So, what is a physician assistant exactly? In this article, we’ll break down the role, salary expectations, and job outlook, and show why partnering with AAG Health can be a game-changer for PA staffing.
P.S. Struggling to keep your facility fully staffed or worried about gaps in patient coverage? AAG Health connects you with skilled physician assistants fast, so you never lose momentum. If you need reliable PA staffing support, our team can help you out.
What is a Physician Assistant?
A physician assistant (PA) is a licensed medical professional who practices medicine as part of a collaborative healthcare team. Trained in the medical model, PAs assess patients, diagnose illnesses, develop treatment plans, assist in surgery, and, in most states, prescribe medications. They typically hold a master’s degree, complete thousands of clinical rotation hours, and pass the National Certifying Exam before getting licensed.
What Does a Physician Assistant Do?
Physician assistants play a hands-on clinical role across nearly every area of medicine. They examine patients, take medical histories, perform physical exams, order and interpret diagnostic tests, diagnose illnesses, develop treatment plans, and in most states, prescribe medications. Many also assist in surgery or manage procedures depending on the specialty.
PAs work alongside physicians, nurses, techs, and specialists, adapting easily to any care team. Their versatility expands access, speeds up patient flow, and reduces pressure on overextended providers. You’ll find PAs in primary care, emergency departments, internal medicine, surgical services, urgent care, outpatient clinics, and even telemedicine.
Here’s a telling stat from the most recent data. More than 178,700 board‑certified PAs were practicing in the U.S. at the end of 2023, a 6.2% increase over the prior year and more than a 75% rise over the past decade. Nearly 95% are clinically active and provide care to millions of patients every week.
Because of this broad scope and flexibility, PAs are a major asset for healthcare facilities. They help:
- Cover workloads
- Fill staffing gaps (especially in high‑demand areas)
- Extend reach into underserved or rural communities
Recruiters and HR teams can use PAs to increase capacity without the full costs or time investment required to hire physicians or wait for long training pipelines.
Physician Assistant Salary: A Detailed Breakdown
When it comes to compensation, physician assistants are among the most well-paid healthcare professionals outside of physician roles, and for good reason. With advanced training, broad clinical skills, and the ability to work across specialties, PAs bring serious value to any medical team.
In this section, we’ll break down the latest data on physician assistant salary, including averages by specialty, setting, and location, so facilities and recruiters know exactly what to expect when budgeting for top-tier PA talent.
Physician Assistant Average Salary
As of May 2024, the median annual wage for physician assistants is $133,260, with a median hourly rate of $64.07. These figures show the growing demand and increasing value PAs bring to healthcare organizations.
Salary varies by work setting. For instance, PAs in outpatient‑care centers, hospitals, physician offices, or government roles may see different compensation levels depending on demand, workload, and local market.
Compensation has been rising: according to the American Academy of Physician Associates (AAPA) 2025 Salary Report, median total compensation increased by roughly 5.5% from 2023. This is a sign that the profession’s value is climbing as demand for PAs grows.
Of course, pay depends on several factors like specialty (emergency medicine, surgery, dermatology, etc.), years of experience, geographic location (cost‑of‑living and regional demand), bonuses or productivity incentives, and setting (hospital, outpatient, private practice, etc.).
Physician Assistant Salaries By Specialty
Compensation for PAs can vary widely by specialty. Here are the top‑earning Physician Assistant specialties in 2024, according to data from the American Academy of Physician Associates (AAPA).
Cardiovascular/Cardiothoracic Surgery
PAs in this surgical specialty were the highest earners in 2024, with a median total compensation of ~$171,000. That includes a base salary of around $162,914 and a median bonus of $10,000. The complexity of cardiac cases, high acuity, and surgical support duties make this one of the most demanding and well-compensated PA roles.
Orthopaedic Surgery
Orthopaedic PAs earned a median total compensation of ~$143,820, with base pay around $135,000 and bonus pay close to $9,000. The role often includes assisting with surgery, managing post-op care, and handling musculoskeletal injuries, all of which command higher salaries.
Radiology
With a median total compensation of ~$143,950, radiology PAs enjoy both strong pay and a unique scope of practice focused on imaging interpretation and procedural support. Their base salary averages $140,000, with bonuses making up the rest.
Emergency Medicine
Emergency medicine remains a top-paying, high-demand specialty for PAs. Total compensation is typically around $155,000 depending on shift structure, overtime, and employer type. PAs in this field often thrive in fast-paced, acute care environments.
Dermatology
Dermatology PAs command impressive compensation, averaging ~$166,000 annually, thanks to a mix of procedures, cosmetic services, and strong patient demand. The dermatology field remains a favorite among PAs for both earning potential and work-life balance.
Critical Care/ICU
PAs working in critical care, ICUs, or hospital medicine often earn around $146,000, depending on the region, patient volume, and bonus structures. These roles involve managing high-acuity patients and coordinating with multidisciplinary teams.
Internal Medicine (General)
Even in more generalist roles, PA compensation is strong. Internal medicine PAs had a median total package of ~$140,000, with base pay around $132,000 and a $10,000 bonus. This specialty offers a broad scope, continuity of care, and wide applicability across health systems.
What Drives the Differences?
- Complexity and risk: Specialties like cardiothoracic surgery, neurosurgery, and orthopedic surgery involve higher‑risk procedures, specialized knowledge, and often surgical assistance, which boosts pay.
- Demand and workload: Fields like emergency medicine or oncology involve high acuity, irregular hours, or high demand, which tends to increase compensation.
- Practice setting: Hospital‑based, surgical, or specialty centers mostly pay more than standard outpatient or primary‑care settings (though outpatient and primary‑care remain valued).
- Bonuses and productivity pay: Many specialties include incentive-based compensation or bonuses on top of the base salary, which can significantly raise total compensation.
Physician Assistant Salaries By Practice Setting
Another important factor in PA salaries is where they work. Here’s how that breaks down.
Operating Rooms and Surgical Centers
PAs working in surgical settings such as operating rooms, surgical centers, or other high‑acuity procedure environments fall among the highest paid. According to a report, PAs in OR/surgery settings had total annual compensation of around US $165,000.
This higher pay reflects the increased responsibilities, like assisting in surgeries, pre‑ and post‑operative care, managing complex patients, and often working irregular hours.
Acute Care Hospitals and Inpatient Units
For PAs in hospital-based inpatient or acute‑care units, compensation remains strong. A report by Medscape shows a median total compensation of around US $146,000 for hospital-employed PAs.
Because hospitals mostly deal with a mix of high-acuity patients, 24/7 care, and varied case loads, these settings reward PAs for flexibility, clinical breadth, and reliability.
Emergency Departments and Urgent Care Centers
PAs in emergency medicine, urgent care, and other fast-paced outpatient settings earn approximately $152,000 per year, according to the same Medscape report that we shared above.
These environments come with heavy patient flow, unpredictable scheduling, and diverse case mixes, all factors that support higher pay ranges.
Why this matters for employers
If you’re hiring PAs, understanding how compensation changes by setting is essential. Pay expectations in surgery, emergency medicine, and inpatient care often differ sharply from roles in primary care or outpatient clinics. Competitive, setting-specific offers help attract qualified candidates, particularly in high-demand markets.
Physician Assistant Salaries By Geographic Location
Where a PA works also has a significant impact on how much they get paid. Below is a breakdown by major region, followed by concrete numbers for some states, especially those paying the most (and least).
Regional Snapshot
- West Coast/Pacific States: States like California and Washington tend to offer some of the highest nominal wages for PAs, driven by high demand, cost of living, and robust hospital/clinic networks.
- Northeast and Mid‑Atlantic: With dense population centers, high healthcare use, and competitive markets, states in this region often offer pay above the national average.
- South and Rural/Lower‑Cost States: Many states here report lower nominal wages, but lower cost of living means pay may still offer decent purchasing power.
- Mixed/Transitional Regions: Some states with mid‑range nominal wages combine moderate cost‑of‑living and access needs, which makes PAs attractive and provides stable salary opportunities.
Top‑Paying States (among the highest in the U.S.)
Here are 10 states that consistently show up among the highest‑paid for PAs according to data on the median annual wage by the U.S. Bureau of Labor Statistics:
These states combine high nominal pay with demand for PAs, often due to dense populations, high cost of living, or strong healthcare infrastructure.
Lower‑Paying States (bottom of national PA salary range)
Here are five states where nominal PA pay is among the lowest in the U.S., according to the same source by the BLS:
Physician Assistant Job Outlook
The future is bright for physician assistants. The employment of PAs is predicted to grow 20% between 2024 and 2034, which is much faster than the average for all occupations.
What’s Driving This Surge
- Aging population and chronic‑disease burden: As more people age or live with chronic conditions, demand for medical care (primary care, chronic‑disease management, preventive care) rises.
- Physician shortages and access gaps: Shortages of physicians, particularly in primary care, rural areas, and underserved communities, create a pressing need for clinically trained providers.
- Shift toward team‑based care and cost‑effective models: Healthcare systems increasingly rely on collaborative models. PAs offer a strong balance between advanced medical training and lower overhead compared with physicians.
- Growth of outpatient care, telemedicine, and flexible care settings: As more care moves outside traditional hospitals (urgent care, outpatient clinics, and remote care), facilities need versatile providers who can handle broad scopes. PAs fit that bill well.

What This Means for Facilities and Recruiters
For healthcare facilities and HR teams, the projected growth and rising demand mean two things:
- Competition for PA talent will intensify. As more facilities seek PAs, quality candidates will be in demand, which makes strategic recruiting and employer branding more important than ever.
- Flexible staffing plans matter. Given high demand, staffing “just in time” or using locum/contract PAs can help cover fluctuations and growth without long delays.
That’s where AAG Health steps in: by tapping into our proprietary data‑driven sourcing platform and high-touch recruiting model, we can help facilities secure qualified PAs quickly, even in competitive markets.
If you’re curious about how a PA compares to other advanced providers (like nurse practitioners), you might also want to check out this helpful comparison.
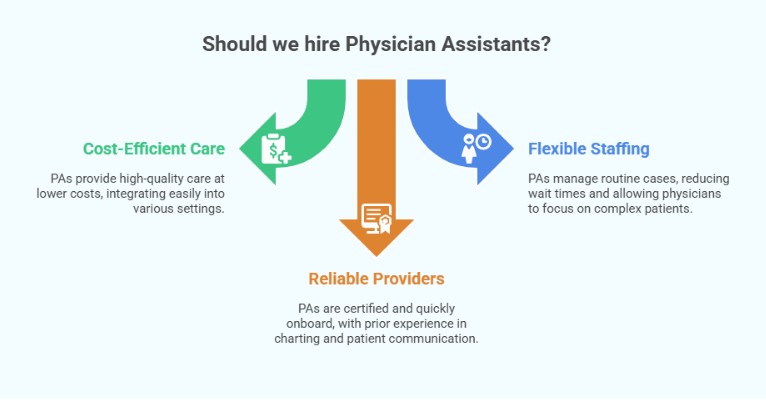
Why Healthcare Facilities Should Hire Physician Assistants
Let’s run through some of the main reasons why healthcare facilities should consider hiring physician assistants.
Cost-Efficient Care Without Sacrificing Quality
PAs deliver high-quality care at a lower cost than physician hires. Their advanced training allows them to diagnose, treat, order tests, perform procedures, and prescribe medications in most states. They integrate easily into hospitals, clinics, surgical teams, and outpatient settings.
Flexible staffing for growing patient volumes
PAs manage routine and lower-acuity cases, support preventive care, and help reduce wait times. This allows physicians to focus on complex patients and high-priority procedures. In rural or understaffed regions, PAs expand access and keep care delivery consistent.
Reliable, credentialed providers who onboard quickly
Every PA completes national certification, state licensure, and ongoing education. Many have prior healthcare experience, which helps them ramp up fast. For HR teams, onboarding a PA means integrating a provider who’s already trained in charting, diagnosing illnesses, care coordination, and communicating with patients.
In fact, a systematic review of 39 empirical studies found that when PAs substitute for physicians, care quality was “comparable or even better,” and 29 of those studies showed lower labor and resource costs when care was delivered by a PA rather than a physician.
AAG Health helps healthcare systems identify, vet, and deploy surgical PAs, primary care PAs, and specialists nationwide. Our average placement time is just 55–90 days (far below the industry norm), and we offer a 90-day replacement guarantee.
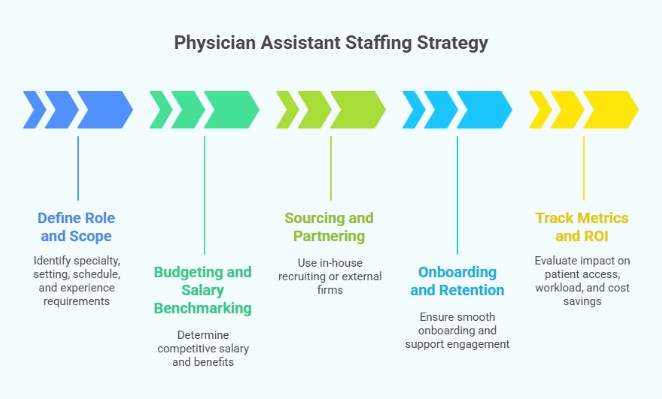
How HR and Recruiting Teams Can Build a Physician Assistant Staffing Strategy
To get the most out of hiring physician assistants, HR teams need a solid strategy. Here's how to build one that works.
1. Define the Role and Scope
Start by clearly identifying your staffing needs:
- Specialty: Do you need a surgical PA, someone for family medicine, or a generalist in clinical medicine?
- Setting: Will the PA work in a medical office, hospital, urgent care, or telehealth?
- Schedule: Decide if the role is full-time, locum tenens, contract, or permanent.
- Experience requirements: Clinical rotations, prior healthcare experience, or specialty-specific skills
Clear role definition prevents mismatches and accelerates sourcing.
2. Budgeting and Salary Benchmarking
We suggest using the current data to offer competitive, realistic packages:
- PA salary can vary greatly by specialty, geography, and setting, so it’s important to clearly understand the market you’re hiring in and how much to offer
- Include performance incentives, benefits, and continuing medical education support to stay competitive
- Reference earlier sections on PA salary by specialty, region, and setting for planning
Remember that competitive packages speed up hiring and improve acceptance rates.
3. Sourcing and Partnering
There are several ways to find qualified candidates:
- In-house recruiting: Use internal HR teams and referral networks
- External staffing firms: You can also save time by partnering with experienced healthcare firms like AAG Health for faster sourcing and access to pre-vetted PA talent.
4. Onboarding and Retention
Smooth onboarding leads to better performance and retention:
- Confirm state licensure, certification examination status, and match with a supervising physician
- Outline clear job responsibilities, including patient volume, prescribing medications, and diagnosing illnesses
- Track performance through patient satisfaction, health outcomes, and clinical impact
- Support long-term engagement through mentorship, career-pathing, and access to continuing medical education
5. Track Metrics and ROI
Evaluate impact beyond cost:
- Patient access metrics: Are wait times going down?
- Provider workload: Are physicians able to focus on complex cases?
- Cost savings: Are PAs reducing reliance on costly temp solutions or overburdened doctors?
Use these metrics to demonstrate the PA program’s value and refine it over time.
Build Smarter, Stronger Care Teams with AAG Health
Understanding what a physician assistant is and how they impact everything from patient access to care quality is a key part of any healthcare staffing strategy. With strong salaries, a promising job outlook, and clinical versatility, PAs offer real value to facilities of all sizes.
If your organization is ready to grow or optimize its workforce, AAG Health can help. Contact us to connect with the right PAs for you and build a team that delivers on every front.
FAQs
What educational requirements does a physician assistant have?
PAs must complete a bachelor’s degree, followed by a master’s degree from an accredited PA program, plus clinical training and a national certification examination.
In which specialties do physician assistants commonly practice
PAs work in a wide range of specialties, including primary care, emergency medicine, surgery, family medicine, internal medicine, and more.
How does the salary of a physician assistant compare to a nurse practitioner?
Both earn competitive salaries, but PA compensation often varies more by specialty and setting, with some surgical PAs earning over $170K annually.
Are physician assistants able to prescribe medication?
Yes, in most states, PAs can prescribe medications as part of their scope of practice under the oversight of a supervising physician.
What is the job outlook for physician assistants in rural versus urban areas?
Rural areas often have higher demand due to physician shortages, which makes PAs crucial for patient care access in underserved regions.
How does the role of a physician assistant differ from that of a physician?
PAs are licensed clinicians who work under a physician's supervision and typically have shorter, more flexible training than medical doctors, though they perform many of the same duties.
How does AAG Health source and vet physician assistants for healthcare facilities?
We use a proprietary sourcing platform that generates over 400 candidate inquiries daily, combined with rigorous screening for clinical fit and cultural alignment.
What types of physician assistant staffing models does AAG Health offer?
AAG Health supports locum tenens, permanent, contract, and hybrid staffing models that are matched to each facility’s needs.

