Healthcare facilities, HR leaders, and recruiting teams are facing a growing challenge: meeting patient demand when provider supply can’t keep pace.
Physician assistants (PAs) have become essential contributors across health care settings. They help you manage rising patient volumes and physician shortages. In a recent national AAPA survey, 86 % of physicians said PAs improve access to care, and 90 % said they play an important role in improving care delivery.
This article explains where the PA profession is headed. We’ll look at the important trends around the scope of practice, compensation, advanced education, and virtual care adoption.
And we’ll break down what these trends mean for recruiting, retention, and patient outcomes, with insights from our experience helping healthcare organizations.
P.S. Struggling to keep patient care on track when PA roles go unfilled, or burnout starts rising? AAG Health’s physician assistant locum tenens staffing delivers credentialed PAs fast, so you can protect coverage, support your teams, and avoid costly care disruptions.
What are Physician Assistants?
Physician assistants are licensed medical professionals who work alongside physicians and other health care teams to deliver patient care in a wide range of settings.
They train under a medical model that emphasizes clinical decision‑making, diagnostics, and hands‑on care. This prepares them to step into roles from primary care to emergency medicine, critical care, and specialty services.
PAs complete rigorous education and training that typically includes:
- Bachelor’s degree in a health‑related field
- Accredited postgraduate PA program, featuring classroom instruction in anatomy, pathophysiology, pharmacology, and ethics
- Supervised clinical rotations in core areas like family medicine, internal medicine, urgent care, and surgery
- Successful completion of the Physician Assistant National Certifying Exam (PANCE) and state licensure before entering clinical practice
While PA programs are shorter than physician training, they still require significant clinical skills and prepare graduates to perform many of the same tasks physicians do in routine care. These include patient histories, physical exams, ordering tests, diagnosing illnesses, and helping manage treatment plans.
In the U.S., there were 189,907 board-certified physician assistants in 2024, and that number has grown over the last year as health care needs rise across settings from rural clinics to metropolitan hospitals.
The following YouTube video breaks down the basics of what a PA does:
Physician Assistant Job Growth and Workforce Outlook
The physician assistant profession is growing fast, and it’s not showing any signs of slowing down. The U.S. Bureau of Labor Statistics projects physician assistant employment will grow 20% from 2024 to 2034, which is much faster than the average for all occupations.
This growth reflects not just more PAs entering the workforce, but a broader shift in how healthcare systems are staffing care delivery.
According to the NCCPA report we shared earlier, the PA pipeline has expanded rapidly over the last decade, and that momentum looks set to continue as more health systems lean on advanced practice providers to close clinical gaps.
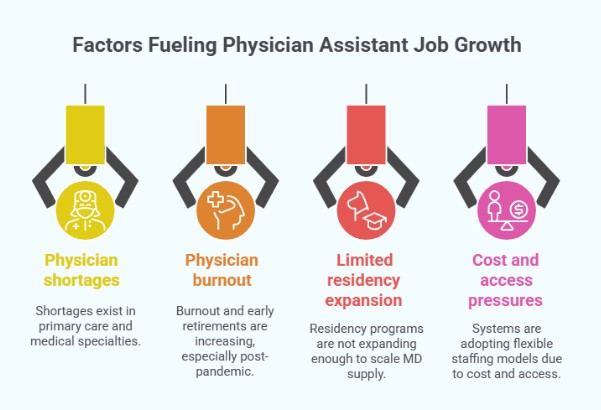
There are several factors fueling this growth:
- Ongoing physician shortages in both primary care and medical specialties
- Burnout and early retirements among physicians, especially post-COVID-19 pandemic
- Limited residency program expansion, which makes it harder to scale the MD supply
- Cost and access pressures are pushing systems to adopt more flexible, team-based staffing models
For healthcare facilities, this means:
- More competition for qualified PA candidates, particularly in high-demand specialties
- Expanded PA roles across emergency rooms, outpatient clinics, rural communities, and virtual medicine
- A need for strategic workforce planning over reactive hiring
Recruiters and HR leaders need to start treating this as a long-term shift in how care gets delivered.
Not sure how to attract and hire the right physician assistant as demand rises? Check out our guide on Hiring a Physician Assistant? Here’s How to Get It Right the First Time to avoid common hiring mistakes.
Expanding Physician Assistant Scope of Practice Across Specialties
Physician assistants are stepping into more complex and demanding roles than ever before. While many still serve in primary care, a growing number now work across high-acuity specialties like:
- Cardiology
- Orthopedics
- Surgical subspecialties
- Oncology
- Emergency medicine
What’s happening? Well, states are updating their supervision requirements and giving experienced PAs more room to practice independently under defined team structures. In Arizona, for example, PAs can now qualify for a system that allows expanded responsibilities after gaining clinical experience.
These changes affect day-to-day care by:
- Improving patient throughput in clinics and emergency rooms
- Easing pressure on physicians in high-demand departments
- Expanding specialty access in rural and underserved areas
For HR teams and healthcare recruiters, this trend means job descriptions are evolving. Facilities are increasingly sourcing PAs with specialized training, clinical research backgrounds, and the ability to manage complex patients.
Physician Assistant Salary Trends and Compensation Growth
Compensation for physician assistants is climbing as health care systems compete for talent with strong clinical skills and specialty experience.
The American Academy of Physician Associates (AAPA) reports that median PA pay increased more than 5.5% in the latest annual salary report. This reflects rising demand across clinical practice settings from primary care to emergency medicine.
The data shows:
- Median salary around $134,000 for full‑time physician assistants, excluding benefits and bonuses
- Higher earnings in specialty areas such as orthopedics, cardiology, and surgical practice
- Bonus structures and incentive pay are adding meaningful income in many markets
- Wage differences by location, with metropolitan areas often paying more than rural settings
Don’t forget about the cost of living. In states with higher housing and transportation expenses, take‑home pay usually adjusts upward to help clinicians manage everyday costs.
Compensation dynamics matter more than ever for recruiting and retention. Health care employers that benchmark against up‑to‑date salary data are much better placed to:
- Attract PAs with strong clinical skills and leadership ability
- Reduce turnover in competitive markets
- Compete in specialties where earnings frequently exceed median levels
Facilities that ignore current compensation trends may find top candidates are being drawn away from them to offers with higher pay, stronger benefits, or clearer career growth.
Check out our detailed guide to learn more about the physician assistants' salary.
Advanced Education and PA‑Specific Doctorate Programs
Physician assistants have traditionally entered clinical practice with a master’s degree, but advanced education pathways are gaining traction.
There are now at least 24 PA‑specific post‑professional doctoral programs across the U.S. Most of these have launched in the past few years and focus on leadership, clinical practice advancement, or specialty preparation.
In addition to doctorate programs, postgraduate residencies and fellowships continue to expand and offer structured clinical experience beyond entry‑level training. By 2020, there were around 72 of these postgraduate programs spanning a variety of specialties, and that number continues to grow with the profession’s expanding scope.
Advanced credentials are often a sign of:
- Deeper clinical specialization
- Readiness for leadership roles in departments or service lines
- Stronger professional credibility when working with multidisciplinary teams
For facilities, this can mean better alignment with complex care needs. A PA with a doctorate or residency training may have strengths in areas like procedural care, chronic disease management, quality improvement, or academic roles. This can improve patient outcomes and service line reputation in units where advanced clinical decision‑making is critical.
Physician Assistants and Telehealth: Virtual Care Adoption Trends
Telehealth has become a bigger part of how care is delivered, and physician assistants are right in the middle of that shift.
According to a recent American Academy of Physician Associates Salary Report, about 49 % of PAs used telemedicine in their clinical work over the past year, up sharply from under 10 % before the COVID‑19 pandemic.
Here’s how PAs support virtual care models:
- Chronic care management with regular remote check‑ins
- Follow‑ups and triage for nonurgent concerns
- Specialty consult support through video or secure messaging
Telehealth brings clear benefits for facilities, like:
- Expanded access without increasing physician headcount
- Better coverage for rural and underserved communities
These advantages matter because virtual care can connect patients to care faster and lower the barriers tied to travel or clinic capacity.
Operational considerations for healthcare facilities include:
- Telehealth competencies are becoming core PA skills
- Structured onboarding and training to get clinicians up to speed
- Digital workflow support, like integrations with electronic health records
What recruiters and HR teams should know:
- Virtual care skills are now a must‑have in many PA candidate profiles
- Training and support structures help clinicians thrive in hybrid care settings
If you’re building teams that deliver care both in person and online, we at AAG Health can help you attract candidates with the right mix of skills and experience.
Physician Assistant Workforce Strategy for Healthcare Facilities
As demand for physician assistants grows and their roles expand, facilities that wait to adjust workforce strategy will face steeper competition for talent. The number of certified PAs has increased by more than 60% over the past decade. This shows how quickly the profession is scaling to meet national healthcare needs.
Healthcare facilities can’t afford to take a reactive approach here. Strategic workforce planning is essential.
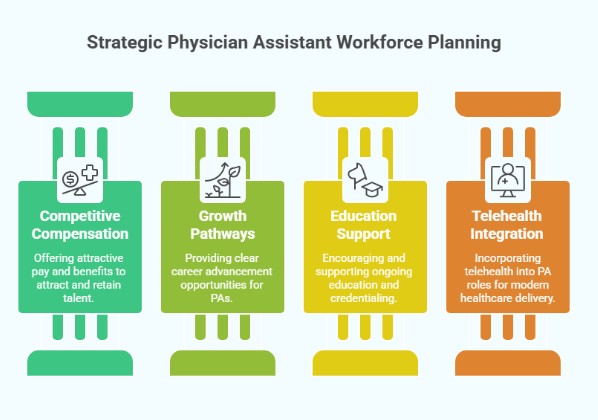
Here’s what you should prioritize:
1. Design competitive compensation and benefits packages
In our experience, successful PAs' offers reflect current market rates and go beyond base pay. We’ve seen that incentives tied to specialty expertise, location challenges, schedule flexibility, or advanced training consistently improve acceptance rates and long-term retention.
2. Create clear clinical growth and specialty pathways
Clinicians are increasingly looking for long-term growth, rather than just a role to fill today. From what we’ve seen working with different healthcare teams, facilities that clearly outline pathways into subspecialties, leadership roles, or advanced clinical responsibilities see higher engagement and stronger retention over time.
We’ve learned that even simple clarity, such as defining how a PA can progress into emergency medicine, surgical support, or supervisory roles, helps candidates visualize a future with the organization rather than viewing the role as temporary.
3. Support advanced education and credential development
Clinicians with advanced degrees or postgraduate training often bring added value in high-acuity and specialty care environments. In our experience, facilities that actively support continuing education stand out in competitive hiring markets.
We’ve observed that tuition assistance, CME stipends, and credentialing support attract more qualified candidates as well as encourage long-term commitment. When organizations invest in professional development, PAs are more likely to invest back through stability, performance, and leadership.
4. Integrate PAs into the telehealth model
As virtual care becomes a permanent part of healthcare delivery, telehealth can no longer sit on the sidelines of PA role design. Based on what we’ve observed across healthcare facilities, teams that intentionally build telehealth into PA responsibilities adapt faster and experience fewer workflow disruptions.
In day-to-day workforce planning, we mostly see that early exposure to digital workflows, such as virtual documentation, remote triage, and patient communication tools, helps PAs gain confidence and deliver more consistent care in hybrid environments.
Facilities should also focus on:
- Proactive pipeline building to maintain a consistent candidate flow
- Role clarity and scope alignment to avoid turnover or misalignment
- Retention-focused workforce planning that looks beyond salary to engagement and satisfaction
Partner with AAG Health to Hire, Retain, and Scale Physician Assistant Talent
The physician assistant profession is changing. From expanding into high-acuity specialties to stepping into virtual care and advanced training programs, PAs are now essential to how care gets delivered, particularly where physician supply is limited or demand keeps rising.
These trends bring opportunity, but they also require new strategies. Facilities that want to attract top-tier PA talent need to stay on top of compensation benchmarks, define role expectations clearly, and support clinical growth through education, telehealth readiness, and long-term workforce planning.
At AAG Health, we work directly with healthcare leaders to do exactly that. We help hospitals, health systems, private practices, and rural clinics:
- Source PAs with the right clinical experience and credentials
- Set compensation structures that reflect real market data
- Shorten time-to-hire without sacrificing candidate quality
- Build lasting placements that improve care continuity and team performance
With over 400 candidate inquiries daily and a 90-day replacement guarantee on exclusive searches, we’re built for precision. Whether you’re filling a high-priority specialty role or planning your workforce for the next 6-12 months, we’ll help you move with confidence.
Ready to strengthen your PA recruiting strategy? Talk to AAG Health today!
FAQs
What’s driving the rapid growth in demand for Physician Assistants?
Demand is rising due to ongoing physician shortages, burnout, limited residency expansion, and increasing healthcare needs across both primary care and specialty settings. PAs help health care teams maintain access and continuity without overextending physician staff.
How are PA roles expanding beyond primary care into specialty areas?
PAs are increasingly working in cardiology, orthopedics, emergency medicine, surgical subspecialties, and oncology as states adjust scope-of-practice rules and facilities rely on team-based care models. This allows experienced PAs to take on more complex clinical responsibilities.
What are current salary trends for PAs, and how should facilities benchmark compensation?
Median PA salaries are now around $134,000, with annual increases exceeding 5% in recent years, particularly in high-demand specialties. Facilities should benchmark compensation using current national and regional data rather than relying on outdated averages.
How are PAs being integrated into telehealth and virtual care models?
Many PAs now support chronic care management, follow-ups, triage, and specialty consults through telehealth platforms. This helps facilities expand access, especially in rural and underserved communities, without increasing physician headcount.
How can AAG Health help healthcare facilities attract and hire top Physician Assistant candidates?
We help facilities define roles clearly, align compensation with market data, and connect with a steady pipeline of qualified PA candidates. Our approach focuses on long-term fit, clinical readiness, and faster placements.
What insights does AAG Health offer on PA compensation benchmarking and market trends?
We provide data-backed guidance on salary ranges, specialty differentials, and regional pay expectations. This helps facilities stay competitive and reduce offer friction during recruiting.
How does AAG Health support facilities in recruiting PAs with specialized clinical or telehealth expertise?
We match facilities with PAs who have the right specialty experience, telehealth skills, and team fit. Our process prioritizes precision sourcing and clear alignment between clinical needs and candidate capabilities.

