Locum tenens is no longer just a backup plan. According to CHG’s 2025 State of Locum Tenens Report, what used to be seen as short-term coverage has now become a core workforce planning strategy for hospitals, medical groups, and health systems all over the country.
As per the CHG’s 2025 report, by the end of 2024, actual locum tenens use surged 25% points higher than organizations had forecasted earlier in the year.
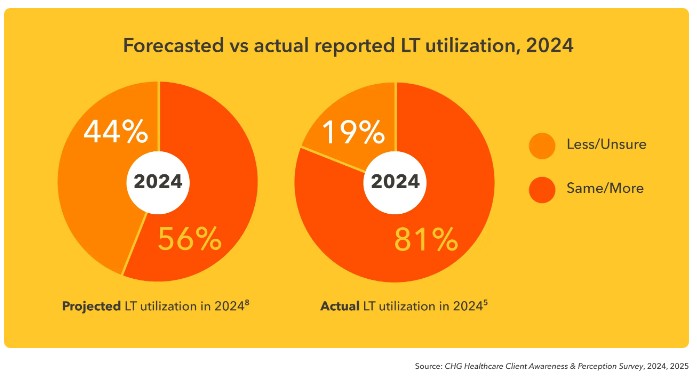
This major gap exposed just how quickly the healthcare industry is changing. Facilities across the U.S. are turning to locums not just to fill gaps, but to protect patient access, ease administrative burdens, and keep revenue flowing in the face of ongoing staffing shortages.
By 2025, this shift had solidified even more. Locums have now become essential tools for stabilizing care delivery, protecting revenue, and adapting to the pressures of a stretched physician workforce.
In the rest of this article, we’ll dive deeper into CHG’s 2025 State of Locum Tenens Report and what it tells us about the current state of locum tenens. We’ll also explore why healthcare facilities are using this model even more than expected.
P.S. Need to backfill a provider role fast without risking care quality? AAG Health can help you place locum tenens quickly with streamlined coordination. Share your specialty, schedule, and start date, and we’ll get moving immediately.
What CHG’s 2025 Report Revealed: Demand Outpaced Forecast
If 2024 proved anything, it’s that locum tenens has become a foundation of healthcare staffing. CHG’s 2025 report showed a major mismatch between what health systems expected and what actually happened.
This surprise surge marked a turning point. Locums have become baseline coverage for many medical groups and hospitals, and is no longer being treated as just a temporary patch during a staffing crunch. And in 2025, 80% of facilities expected their locum usage to either hold steady or increase.
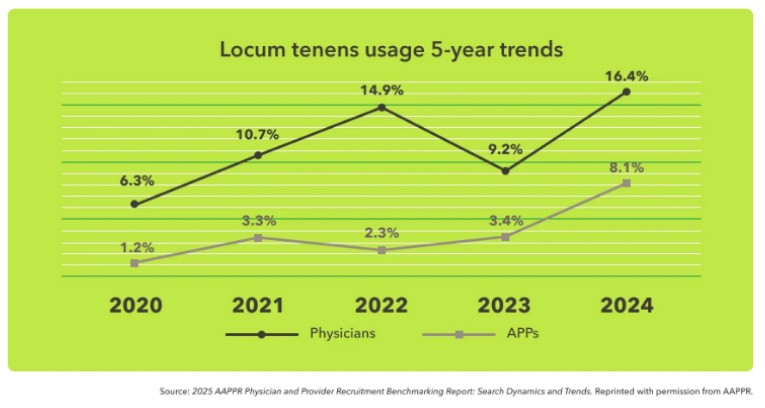
This rising demand was evident in the recruitment data, too. In 2024, locums were involved in 16.4% of physician searches, which is the highest level ever recorded. And for advanced practice providers (APPs) like nurse practitioners and physician assistants, that number hit 8.1%, also a record high.
Whether it’s to manage growing patient volumes, fill in during transitions, or relieve pressure from physician burnout, it is evident that facilities are turning to locums more than ever.
“Locums isn’t just a temporary fix anymore. It’s become a core part of how hospitals and health systems are tackling staffing challenges, maintaining continuity of care, and preventing provider burnout.” — CEO & President of CHG Healthcare, Leslie Snavely
Why Facilities Turned to Locums Tenens Most Often
As per CHG’s 2025 Locum Tenens report, backfill remained the top reason healthcare organizations turned to locum tenens in 2024. When a provider leaves unexpectedly, or a search for a permanent hire stretches on, locums help keep schedules intact and patient care uninterrupted.
According to the report, 67% of facilities used locums while searching for a permanent provider, and 61% brought in locums immediately after someone left the organization. Other common reasons include maternity and paternity coverage, vacation coverage, and rising patient demand.
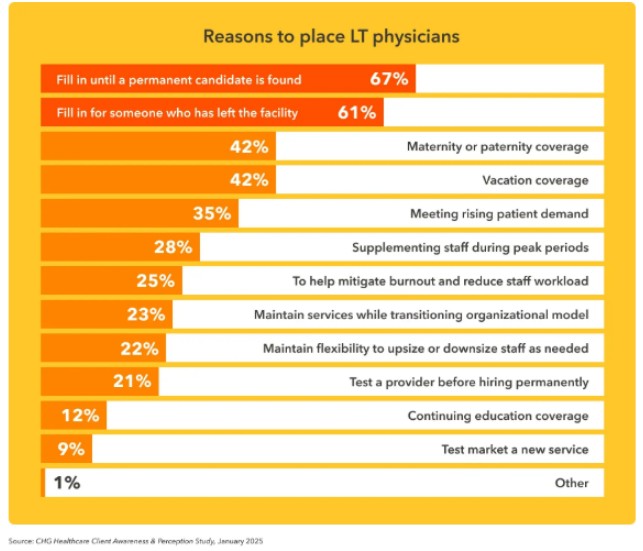
So the heart of locum use is still the same: making sure care doesn’t stall just because there’s a gap on the schedule.
But that’s not the whole story anymore. More and more leaders say they’re using locums as part of a broader, more intentional workforce strategy. Instead of just reacting to turnover, they’re planning ahead by building locums into staffing models.
This helps maintain access, reduce pressure on permanent teams, and create more flexibility across the clinical workforce.
Check out the following YouTube video to learn more about how healthcare facilities are using locums to deal with staffing shortages:
The New Locums Use Cases That Emerged in 2025
Locum tenens staffing has always helped cover provider gaps, but now the use cases are expanding well beyond that. Instead of just reacting to turnover, more health systems started using locums to proactively manage patient volumes, reduce burnout levels, and explore new services without the risk of permanent hires.
This marked a real shift in how locums fit into the healthcare staffing industry. Facilities were building locum support into their plans from day one, not just when things went sideways.
Meeting demand and smoothing peaks
As patient volumes climbed in 2024 and into 2025, more organizations used locums to handle the surge. 35% of facilities reported bringing in locums to meet rising patient demand, while 28% used locums during predictable peak periods such as flu season or summer vacations.
Instead of overloading permanent staff or risking patient access, leaders used locums to maintain coverage and service quality year-round.
Burnout mitigation became a formal strategy
The link between physician burnout and staffing gaps is clearer than ever before. In the 2025 report, 25% of facilities reported using locums specifically to reduce workload and relieve burnout. This is a sign that well-being is becoming an active part of workforce strategy.
With staffing shortages continuing and administrative tasks piling up, using locums for burnout relief is now a practical tool to protect both care delivery and physician retention.
Transitions, flexibility, and testing new services
Beyond demand and burnout, facilities got creative. 23% used locums to support transitions like department restructuring or leadership changes. 22% used locums to build more staffing flexibility into rigid workforce models. And 9% used locums to test-market new services before committing to full-time hires.
The “Modern Locums Physician” Profile CHG Documented
Forget the old image of the always-on-the-road, suitcase-in-hand locum physician. The CHG 2025 report paints a much more grounded and experienced picture of today’s locum workforce.
As of May 2024, 8% of physicians (roughly 57,000) were actively working locum tenens. Add in those with prior experience, and about one-third of physicians overall had worked locums at some point in their careers.
Interestingly, many of these providers didn’t wait until late career to try it out. More than half (56%) started locum work within 10 years of finishing training, and the average physician had six years of locum experience under their belt. About 15% had been doing locum tenens work for over a decade. For a lot of providers, then, it's not just a phase, but a long-term choice.
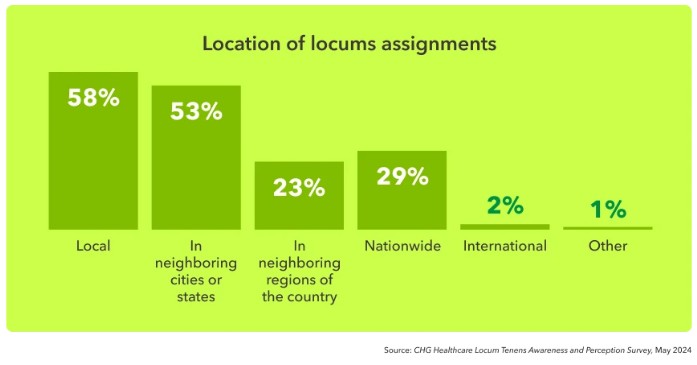
Another interesting shift here is that travel isn’t the default. While some locums still take cross-country assignments, most are staying closer to home. 58% preferred local work, and 53% opted for neighboring cities or nearby states. That makes locums more sustainable for providers and more appealing to facilities that care about continuity and cultural fit.
Quality of Care: Studies CHG Cited Showed Comparable Outcomes
One of the most common questions around locum tenens is whether quality takes a hit when you're not working with permanent staff. But the data is encouraging here.
The CHG report highlighted multiple studies showing that patient care delivered by locum physicians was just as strong as that provided by full-time staff. When facilities bring in vetted, qualified locums, particularly through experienced healthcare staffing partners, the outcomes speak for themselves.
Key outcomes were similar to those of staff physicians
- A large Medicare analysis found no significant difference in 30-day mortality between patients seen by locums and those seen by permanent physicians
- Other peer-reviewed studies showed no meaningful differences in complication rates, length of stay (LOS), or key emergency department metrics
The takeaway is simple: locums are fully capable of delivering high-quality medical care, particularly when their placements are well-matched and supported by effective systems.
Administrative perception improved sharply by 2025
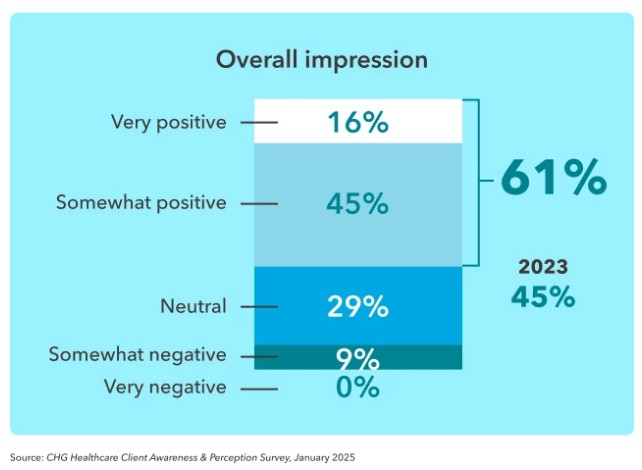
Hospital leadership also changed its views in a big way in 2025.
- 61% of hospital decision-makers had a positive impression of locum tenens physicians by 2025, up from just 45% in 2023.
- 29% reported a neutral impression.
- Only a small minority (9%) left somewhat negative views.
Locums and Financial Impact: How Healthcare Facilities Used It to Protect Revenue
Staffing gaps stretch your clinical teams, but they hit your bottom line, too. In 2025, healthcare facilities leaned more heavily on locum tenens to prevent major revenue loss tied to long provider vacancies.
The CHG report made it clear. When it takes months to fill a role, keeping patient access steady with locums can be the smarter financial move.
Vacancy-driven revenue loss was a major pressure point
- The median physician search time was 129 days, over four months of open schedules and delayed services
- During that time, facilities faced an estimated $2.6 million in lost patient revenue for each unfilled physician role
For health systems, outpatient clinics, and medical groups, this kind of revenue gap isn’t sustainable.
CHG reported locums could produce ROI
Despite common concerns about cost, many organizations found locums actually delivered a strong return, especially when used strategically.
- The average locum physician generated a 5.6x ROI, with some systems reporting up to 8x returns
- 46% of facilities cited revenue loss prevention as a key benefit of their locum staffing strategy
When you factor in the cost of delays, lost billing, and patient leakage, timely locum coverage starts to look like a smart investment.
Facilities weighed cost vs continuity
Facilities acknowledged the higher price tag associated with locums, but many were willing to pay for stability and patient access.
- 63% said cost was a drawback, but it wasn’t a dealbreaker
- 65% said continuity of care was a benefit worth the investment, especially when locums could be kept in place for longer-term assignments
APP Locums Growth Is Accelerating (Especially CRNAs)
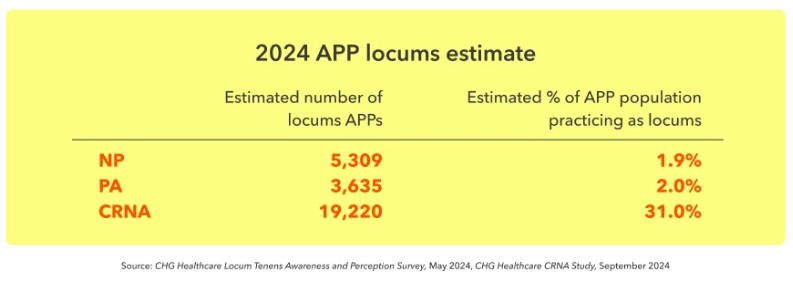
While physicians still make up the bulk of the locum tenens workforce, advanced practice providers (APPs) like nurse practitioners, physician assistants, and CRNAs have been gaining ground fast. As health systems look for more flexible, team-based care models, APP locums have become a key part of the strategy.
Whether to fill gaps, extend physician bandwidth, or launch new services, APP locums are now playing a bigger role in provider recruitment and care delivery than ever before.
Looking for qualified APP locums to support your care teams? AAG Health can help you place experienced APPs quickly. Find out more here.
APPs remained a smaller share but expanded rapidly
CHG’s 2025 data showed that although APP locums still represented a minority of the market, their adoption was accelerating across care settings.
- APPs made up around 15% of all locum providers in 2024. This means they’re still a smaller slice, but growing quickly.
- More than 28,000 APPs were working locums and helping to fill urgent staffing needs across inpatient and outpatient settings
Facilities planned to scale APP locums
As staffing pressures continued into 2025, many healthcare organizations identified APP locums as a scalable solution to support care delivery without overextending physician teams.
Looking ahead, 39% of healthcare organizations said they planned to increase their use of APP locums, reflecting confidence in their impact on patient care and team efficiency.
APP locums offered a way to improve staffing flexibility, reduce burnout levels, and support more sustainable clinical workforce models.
CRNA demand surged
One of the fastest-growing APP specialties in the report was Certified Registered Nurse Anesthetists (CRNAs).
In 2025, CRNA demand was projected to grow by 25%, driven by ongoing workforce shortages and a growing need for anesthesia services in both hospitals and outpatient centers.
From surgical teams to rural clinics, more facilities are realizing that APP locums, particularly CRNAs, can play a strategic role in filling care gaps and supporting consistent access.
Telehealth Locums: High Interest, Limited Supply
Telehealth is now a permanent part of how care gets delivered. And in 2025, locum tenens providers made it clear: they want in.
The CHG report showed strong demand from physicians and advanced practice providers looking for virtual care roles. But while the interest was high, the actual number of telehealth locum assignments lagged behind.
- 47% of locum providers said they were very or extremely interested in taking on telehealth work
- Another 21% were moderately interested, showing that virtual care options are top-of-mind for a majority of clinicians in the locum tenens industry
Availability lagged behind interest
- Despite that interest, only 20% of providers reported being offered telehealth locum opportunities
- When those assignments were available, they were popular. In fact, 62.5% of providers accepted when given the option.
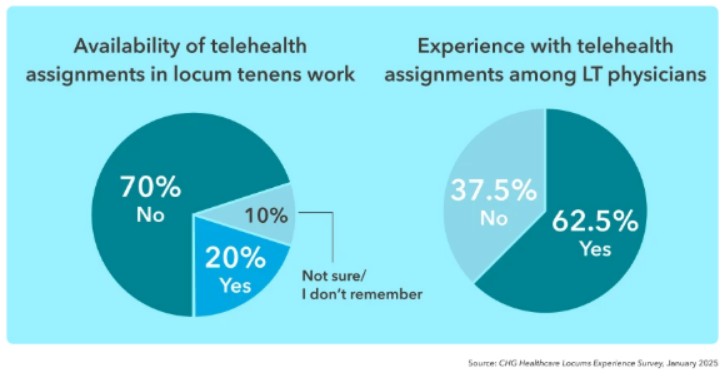
As telehealth integration continues to improve and digital platforms mature, the gap between provider interest and assignment availability may start to close. But in 2025, demand still outpaced supply. This points to an opportunity for health systems to expand access through virtual locum coverage.
Looking to close the gap between telehealth demand and provider availability? AAG Health’s telehealth locum tenens staffing services can help you deploy telehealth-ready locum physicians quickly, without licensing or onboarding delays.
Technology’s Role in 2025: Faster Locums Operations Through Systems and VMS
As locum tenens have become more central to workforce planning, healthcare organizations have started turning to tech to solve one of their biggest pain points: speed.
From faster credentialing to streamlined vendor coordination, technology, especially AI tools and vendor management systems (VMS), is helping health systems reduce delays and improve their overall locum staffing experience.
Digital platforms, data-driven tools, and workflow optimization strategies are now critical parts of modern healthcare staffing solutions. This is true across the entire locum tenens pipeline.
Leaders believed tech could improve contingent workforce outcomes:
- 59% of healthcare leaders said they believed technology could improve locum staffing outcomes, particularly around coordination and efficiency
- 54% reported seeing real value in emerging AI tools like digital portals for credentialing, automated scheduling, and even AI-assisted candidate matching.
Credentialing delays topped the pain points
Despite all the progress, credentialing continued to be the top operational hurdle in 2025:
- 49% of leaders cited credentialing delays as their biggest barrier to faster placements
- Other major issues included scheduling conflicts (44%) and inefficient processes (43%), all of which slowed down time-to-fill, especially in urgent coverage situations

VMS adoption reached the mainstream:
- By 2025, 53% of health systems had adopted a vendor management system (VMS) to streamline locum operations
- Another 20% said they expected to deploy a VMS within the year, which shows that VMS platforms are now a go-to solution in locum staffing strategy
Top reasons for VMS adoption included:
- Efficiency: 61%
- Reporting and visibility: 56%
- Faster placements: 53%
- Pricing control: 53%
These tools are playing a bigger and bigger role in helping organizations stay competitive when it comes to hiring and managing locums.
How Facilities Can Hire Locum Tenens Faster
With demand high and vacancies costly, the fastest-moving health systems need to plan ahead rather than react. The CHG report made it clear that speed-to-fill depends heavily on getting organized.
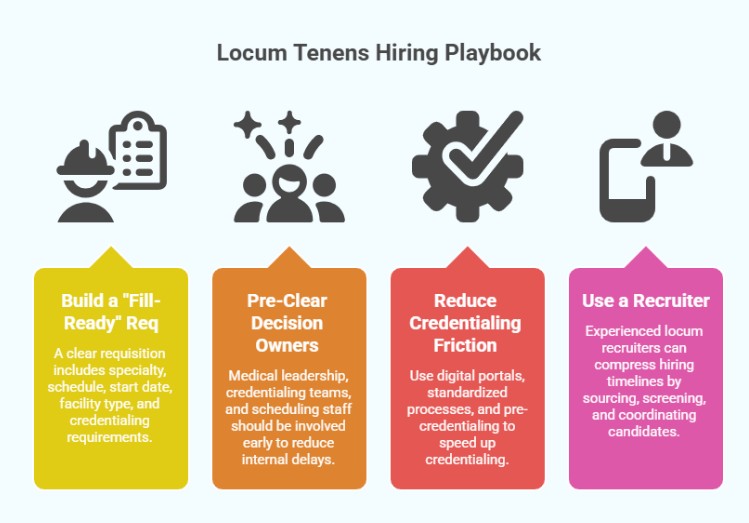
Facilities that built streamlined processes around locum staffing saw faster placements, fewer disruptions, and better patient care continuity. Here’s the four-part playbook they followed:
1. Build a “fill-ready” req
Start with a clear, complete requisition so there’s no back-and-forth once the search begins. A good req should include:
- Specialty and subspecialty (if applicable)
- Schedule, including call requirements
- Start date and expected duration
- Facility type or setting
- Credentialing requirements (licenses, DEA, board certs)
This helps agencies move quickly, with qualified candidates submitted right out of the gate.
2. Pre-clear decision owners to reduce internal delays
Bottlenecks usually happen inside the organization. Facilities that moved fastest had already looped in:
- Medical leadership (for clinical approval)
- Credentialing teams (for paperwork and systems access)
- Scheduling and onboarding staff (for start logistics)
The fewer back-and-forths during the placement process, the faster you can lock in top talent.
3. Reduce credentialing friction
As we learned, credentialing delays were the number one operational challenge cited in CHG’s 2025 report and were a problem for nearly half of all leaders. To avoid getting stuck in the same spot:
- Use digital portals or talent management software to collect paperwork quickly
- Set up a standardized process for internal teams
- Consider pre-credentialing for high-priority roles when possible
4. Use a recruiter to compress time-to-fill
Facilities working with experienced locum recruiters like AAG Health, particularly ones focused on niche specialties, shaved days or even weeks off their hiring timelines. Here’s what they gained:
- Faster sourcing from a pre-vetted locums database
- Smarter screening that matched not just skill, but fit
- Submission-ready candidates with confirmed availability
- Seamless coordination to get providers to the start line with minimal friction
Why Facilities Partnered With AAG/H for Speed-to-Fill
When healthcare organizations need to act quickly to fill mission-critical roles in specialties such as radiology, emergency medicine, and infectious diseases, many turn to AAG Health. We bring scale, strategy, and precision to the table.
Here’s what made AAG Health different:
- With an average placement time of 55–90 days, far faster than the industry norm of 120+ days, AAG Health helped facilities stay ahead of staffing shortages.
- Our proprietary locums database and AI-driven sourcing tools generate over 400 candidate inquiries daily, ensuring scale without sacrificing fit.
- We identify mission-aligned clinicians who integrate into the culture and improve the patient experience. This supports long-term outcomes.
- AAG Health helps clients streamline vendor management, which fits into the broader industry trend toward centralized platforms and more transparent VMS-driven operations.
- Our placement success rate is 80% on exclusive searches, and we back our work with a 90-day replacement guarantee.
- We are also a proud member of the American Staffing Association (ASA), thanks to our strong compliance, measurable impact, and commitment to healthcare workforce excellence.
We’ve supported health systems, specialty clinics, and multi-site providers through some of their toughest workforce challenges.
If your locum needs are rising, the fastest path is operational readiness plus a recruiter that moves fast. Reach out to AAG Health to fill locum physician or APP roles quickly and keep your service lines covered.
Key Takeaways (Looking Back at CHG’s Locum Tenens 2025 Report Findings)
The 2025 State of Locum Tenens Report confirmed what many healthcare leaders already suspected: locum tenens staffing is rapidly moving from optional to essential.
As the workforce shortage continues and patient access becomes harder to maintain, facilities are leaning on locums to operate smarter and protect continuity of care.
Here’s a quick recap of what stood out:
- Locum use outpaced forecasts by 25 percentage points in 2024, which highlights the growing gap between staffing plans and real-world needs
- 80% of organizations expected their locum use to remain steady or increase
- Recruitment reliance reached record highs, with locums used in 16.4% of physician searches and 8.1% of APP searches.
- Vacancy-driven revenue loss was steep, with median search times at 129 days and potential revenue loss topping $2.6 million per open physician role
- Strategic locum use delivered real ROI, with many organizations reporting returns of 5.6x to 8x or more
Whether you’re planning ahead or responding to urgent coverage needs, locum staffing is now a strategic necessity, and having the right systems and partners in place makes all the difference.
FAQs
What is locum tenens, and how does it work?
Locum tenens refers to temporary medical staffing, typically physicians or advanced practice providers (APPs), who fill in when a facility needs short-term coverage. These roles help health systems maintain continuity of care during vacancies, spikes in demand, or transitions. The model is especially useful in health system planning where staffing flexibility is critical to long-term success.
Why are more healthcare organizations using locum tenens in 2026?
The physician workforce is stretched thin, and staffing shortages continue to impact patient access and outcomes. Facilities turned to locum tenens not just for backfill, but as part of a strategic shift toward more agile revenue models, better patient engagement, and even testing new care delivery structures. Locums also help offset provider burnout and protect operational stability.
What’s the difference between APP locums and physician locums?
APP locums, like nurse practitioners, physician assistants, and CRNAs, offer additional flexibility and can extend care teams in both inpatient and outpatient settings. Physician locums typically handle more complex or specialized cases. Both play a key role in workforce planning and improving patient outcomes when used strategically.
Is locum care as good as permanent staff care?
Yes. Multiple studies have shown that locum providers deliver care with no meaningful difference in patient outcomes compared to permanent staff. With proper support, onboarding, and systems in place, locum clinicians contribute just as effectively to quality care and patient safety.
How does locum staffing affect hospital revenue?
Locums help prevent massive revenue loss during long vacancies. As per CHG’s 2025 locum tenens report, in 2024, the average unfilled physician role resulted in $2.6M in lost patient revenue. Strategic locum staffing can generate a 5.6x to 8x ROI by maintaining services and reducing provider turnover.
What specialties does AAG Health cover for locum placements?
AAG Health places physicians and advanced practice providers across a wide range of specialties, including radiology, emergency medicine, infectious disease, anesthesia, and more. We also support hard-to-fill roles in niche specialties and underserved markets, using real-time market intelligence and proprietary sourcing tools to deliver mission-aligned talent quickly and reliably.
How fast can AAG Health fill a locum tenens position?
Our average placement time is 55-90 days, which is significantly faster than the industry norm of 120+ days. We achieve this speed by combining high-volume inbound candidate flow (400+ daily inquiries), AI-enabled sourcing, and a streamlined, high-touch coordination model that keeps every step of the process moving from credentialing to onboarding.
Why should I choose AAG Health over other locum staffing agencies?
We deliver a placement success rate of 80% on exclusive searches, offer a 90-day replacement guarantee, and help clients realize 50-70% cost savings through efficient, tailored locum strategies. We’re proud members of the American Staffing Association, recognized for compliance, ethics, and quality.

