Telehealth and telemedicine are frequently used interchangeably. But if you’re running a clinic or healthcare organization, the difference matters a lot. That’s because it affects how you invest in tech, how you staff your team, how you bill, and ultimately, how you care for patients.
Telemedicine is about direct clinical care. Telehealth is broader, encompassing the entire digital care experience, from remote monitoring to patient engagement to staff training. Knowing where one ends and the other begins can save you time, money, and a lot of frustration.
And here’s why this matters right now: according to a 2021 McKinsey article, up to $250 billion in U.S. healthcare spending could shift to virtual care models, if organizations can learn how to use them strategically.
This article breaks it all down for you. You’ll walk away with real clarity and next steps to help you decide what’s right for your clinic.
What to expect:
- A side-by-side breakdown of telehealth vs. telemedicine, including who uses what and why
- The top 10 differences every clinic should understand
- Practical advice on how to choose (and combine) both for maximum impact
- A checklist to guide your virtual care strategy
- Real-world insights on billing, tech, and compliance
Let’s dive in.
Telemedicine vs Telehealth at a Glance
Telemedicine and telehealth have the same medium, but they differ in terms of services, beneficiaries, type of care, and even regulations and billing.
Here’s how they compare:
1. Telemedicine vs Telehealth: Scope of Services
Telehealth is the big umbrella, covering clinical care and the broader healthcare ecosystem:
- Remote medical services like diagnosing and treating patients via video or phone
- Non-clinical functions such as provider training, administrative meetings, patient education, and chronic care monitoring
The Health Resources & Services Administration (HRSA) clearly says telehealth “includes ‘telemedicine’ services but encompasses a broader scope of remote health care services.” That means it may include things like provider education, admin meetings, and continuing medical education in addition to clinical services.
Telemedicine, on the other hand, is more focused. It refers specifically to remote clinical services. This includes activities like diagnosing illnesses, managing medications, providing follow-ups, and consulting with other providers, all of which are done through secure, virtual platforms.
Think of telemedicine as a specialized tool within the larger telehealth toolbox.

The numbers
During the COVID-19 pandemic, telehealth usage skyrocketed: jumping 78 times higher than pre-pandemic levels according to the 2021 McKinsey article we previously cited. At its peak in April 2020, about 32% of outpatient and office visits happened virtually. While that number has leveled off, virtual care still makes up about 13–17% of visits, a massive leap from the 1% baseline seen before 2020.
Why this matters to clinics & health organizations
For clinics and healthcare organizations, understanding this difference is key. If you're only investing in telemedicine, say, adding video visit functionality, you might be missing out on the broader benefits of telehealth. This includes tools for staff training, automated patient engagement, and better data sharing across care teams.
Clinically focused telemedicine has clear ROI in the form of billable visits, but the larger telehealth ecosystem supports efficiency, collaboration, and long-term patient outcomes, often in ways that aren't directly reimbursed but still impact your bottom line.
2. Telemedicine vs Telehealth: Who Practices It?
Telehealth serves a wide range of professionals beyond just doctors. It’s commonly used by nurses (especially in telenursing), mental health providers, dietitians, physical therapists, and even administrative teams handling training, case reviews, and patient outreach.
According to federal data from Beckers Hospital Review, 57% of nurses reported using telehealth in 2022, up from 50% in 2018. Meanwhile, by 2023, nearly 96% of HRSA-funded health centers were using telehealth for primary care. These numbers show that telehealth is deeply embedded across clinical and administrative roles, not just in physician workflows.
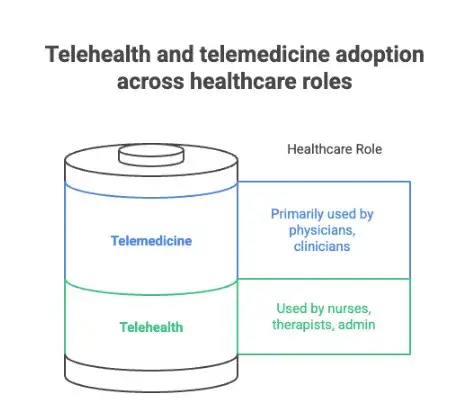
On the other hand, telemedicine is mostly used by physicians and other licensed clinicians, like nurse practitioners or physician assistants, who are directly delivering care to patients. The CDC’s National Health Statistics Report shows that in 2021, 80.5% of office-based doctors in the U.S. were using telemedicine via video to see patients, compared to just 16% in 2019. That sharp rise shows how clinicians adopted remote care in response to demand, but also that telemedicine remains a clinical, doctor-led activity.
The graphic below emphasizes the difference here:
Why this matters for clinics and healthcare organizations
If you're rolling out a telehealth initiative, whether it’s nurse-led remote monitoring, group sessions, patient education, or admin support, you’ll want to involve a broader stakeholder group. This means including nursing, allied health, and support staff in planning, training, and tool adoption.
If your focus is telemedicine, such as virtual doctor visits or specialist consults, your implementation can be tighter, centered on secure, compliant video platforms, EHR integration, and direct clinical workflows.
Understanding these "who uses it" distinctions helps you build a better rollout plan, set up proper training, and match the right tech tools to the right users.
3. Telemedicine vs Telehealth: Type of Care
As we said above, telehealth encompasses virtual patient visits, but also broad care support.
Think of it as your digital wellness hub. It includes patient education (webinars, automated reminders), wellness coaching, remote patient monitoring (like wearables or glucose tracking), and even text-based check-ins.
McKinsey noted in 2020 that post-pandemic, healthcare orgs have heavily invested in remote monitoring and digital therapeutics, expanding well beyond simple video visits. The market has kept its post-pandemic rise, growing to over $14 billion in 2024 and projected to grow at a forecasted CAGR of 12.8% to over $29 billion by 2030.
In contrast, telemedicine is laser-focused on clinical insights and treatment: It’s exclusively about delivering diagnosis, medical treatment, and clinical decision-making via virtual channels like video or phone calls.
Check out the image below for a breakdown:
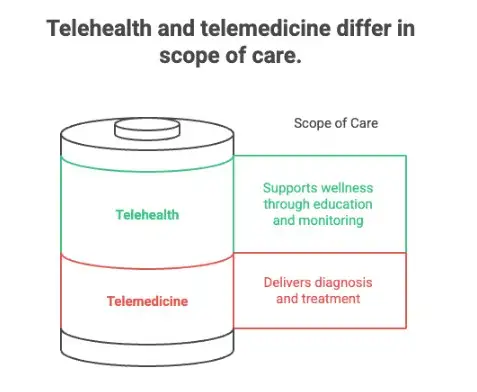
What this means for clinics and healthcare organizations
Patients and clinics navigating the two options should note:
- If a clinic offers telehealth, it's likely combining support services (like self-care tools, coaching, or staff education) with clinical access. This forms a holistic patient experience.
- If the service is labeled telemedicine, expect a tightly structured clinical interaction with real-time provider evaluation, diagnosis, treatment, and follow-ups using secure systems.
Clinics building a hybrid care model need both. Telemedicine brings in revenue through billable visits, while telehealth enhances patient engagement, improves outcomes, and supports long-term wellness, all of which helps clinics reduce readmissions and improve care continuity.
4. Telemedicine vs Telehealth: Use Cases
Telehealth and telemedicine each shine in different spotlights when it comes to practical use.
Telehealth is more versatile, going beyond clinical care to support the entire healthcare ecosystem:
- It’s used for staff training, like online continuing education and virtual case reviews.
- Ideal for public health campaigns, such as webinars on vaccination or chronic-disease prevention.
- Remote patient monitoring (RPM) is a cornerstone, tracking vitals from home through wearables or connected devices.
For example, Medicare data shows that the number of enrollees using RPM jumped more than 10× between 2019 and 2022. McKinsey also reports that over 50% of patients are now interested in digital health tools that let them track their health and share that data with providers. That kind of adoption supports a wider vision of telehealth where clinics can proactively engage, educate, and coach patients outside of office walls.
Telemedicine, in contrast, is once again focused laser-sharp on clinical care. It's all about real-time virtual visits, follow-ups, prescriptions, and consults.
Why this matters for clinics
If your clinic is aiming for telehealth, you're training staff online, launching community wellness initiatives, and monitoring patients between visits to catch issues early.
On the flip side, if you're focusing on telemedicine, you're streamlining for billable, clinical interactions like virtual checkups, medication management, and specialist consults. Ideally, clinics can layer both: telemedicine delivers care, while telehealth builds engagement and prevents complications to create a well-rounded care ecosystem.
5. Telemedicine vs Telehealth: Regulations
Telemedicine typically faces stricter regulatory oversight than telehealth because it deals directly with patient care. That means:
- Full compliance with HIPAA and HITECH privacy/security standards
- State-specific medical licensing for providers
- Controlled substance prescribing governed by federal laws like the Ryan Haight Act
Telehealth, on the other hand, includes non-clinical services like administrative meetings, education, or general wellness outreach that don’t always fall under the same regulatory microscope. However, once telehealth activities cross into clinical territory (like diagnosis or patient monitoring), the same rules that govern telemedicine often apply.
During the COVID-19 public health emergency, the U.S. Department of Health and Human Services temporarily relaxed enforcement of HIPAA compliance for telemedicine tools used in good faith. This flexibility allowed clinics to use platforms like Zoom or FaceTime to reach patients quickly, but the waiver officially ended in May 2023, and enforcement is back in full effect.
Regulatory variation also exists across states. As of late 2024, many state Medicaid programs reimburse for all four major telehealth modalities: live video, store-and-forward, remote patient monitoring, and audio-only services. But reimbursement doesn’t automatically mean you’re in the clear: each service type comes with its own rules around provider licensing, documentation, and consent.
Here’s a quick breakdown of the regulatory differences between telehealth and telemedicine:
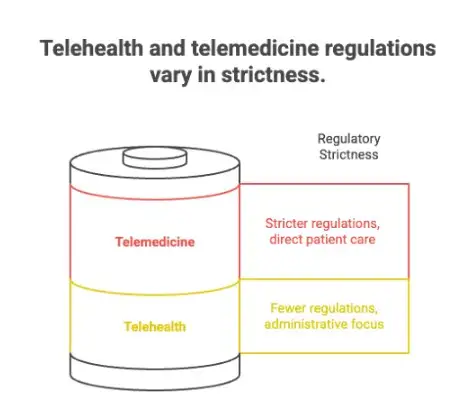
What does this mean for healthcare providers?
For clinics and healthcare organizations, the takeaway is this: telemedicine demands airtight compliance from day one when it comes to HIPAA-secure platforms, multi-state licensure planning, and close monitoring of legal changes. Telehealth gives you more room to maneuver, but only if you stay on the non-clinical side of the line. Once patient data or clinical advice gets involved, the guardrails come up fast. If you’re a healthcare provider, you need to make sure you’re following the current federal and state regulations.
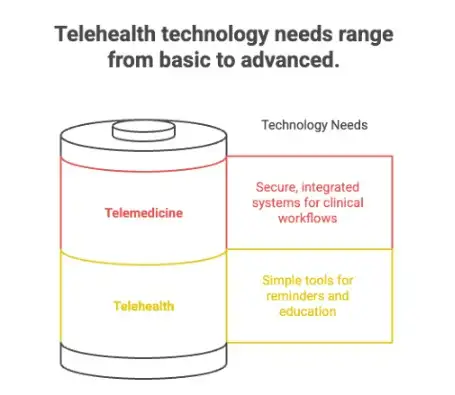
6. Telemedicine vs Telehealth: Technology Needs
Before the pandemic, health system leaders largely focused on synchronous telemedicine, but soon recognized that remote monitoring was the next investment frontier. In fact, a McKinsey analysis shows that virtual healthcare peaked at 38× pre‑pandemic levels.
Indeed, telemedicine comes with high-tech demands and tight data-handling requirements. Clinics offering virtual visits rely on HIPAA-compliant video platforms, strong EMR/EHR integration, and rigorous data security. These systems need to support real-time clinical workflows like scheduling, documentation, and teleprescribing, without compromising patient privacy.
Meanwhile, telehealth services that fall outside pure clinical care can work with lighter technology. You might use apps for patient reminders, wearable data syncs, or simple messaging tools. These tools are easier to implement and more cost-efficient, especially for wellness coaching or educational modules that don’t involve direct diagnosis or treatment.
McKinsey reports that the use of remote patient monitoring and digital therapeutics grew significantly following COVID‑19, with health systems expanding investments beyond just video visits to integrate richer data flows and analytics in patient care.
What this means for healthcare organizations
Understanding these tech needs helps healthcare organizations like yours:
- Choose the right platform: Telemedicine demands fully secure, integrated systems; telehealth may only need simpler reminder, education, or monitoring tools.
- Scale wisely: Integrating EMR/EHR is essential if you anticipate clinically driven workflows or teleprescribing.
- Keep data safe: Even wearable or remote monitoring info must feed into secure storage, especially when patient data is part of ongoing care.
In short, if you're prioritizing telemedicine, plan for enterprise-grade architecture. If telehealth is your focus, you can start lean with light-tech tools and build up as clinical functionality develops.
7. Telemedicine vs Telehealth: Billing & Reimbursement
Telemedicine services are generally billable under insurance and government programs. In fact, evaluation-and-management claims for telemedicine in 2021 were reimbursed by private insurers at nearly the same rate as in-person visits: $99 on average for telemedicine vs. $98 for in-person visits, according to a KFF Health System Tracker report.
Of course, Medicare reimbursement policies can vary.
Telehealth services outside direct clinical care like training, webinars, or patient engagement may not qualify for reimbursement unless they fall under approved clinical categories. Medicaid coverage varies by state, with only a subset covering non-clinical telehealth. Some states mandate private insurers reimburse for telehealth, but implementation remains patchy, and not every modality is covered.

What it means for healthcare
For clinics and health organizations, the implications are clear: telemedicine offers a direct revenue channel but only if you’re set up with the correct billing codes, CPT modifiers, and payer compliance. Telehealth might boost patient engagement or operational efficiency, but without clinical coding, it’s unlikely to generate direct reimbursement.
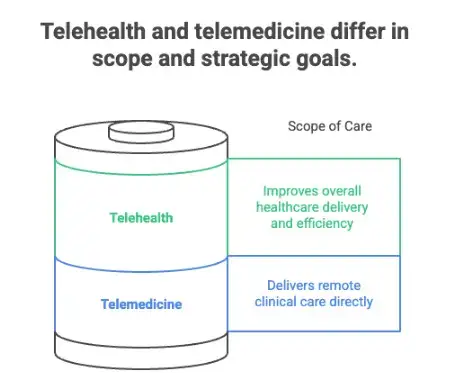
8. Telemedicine vs Telehealth: Goals
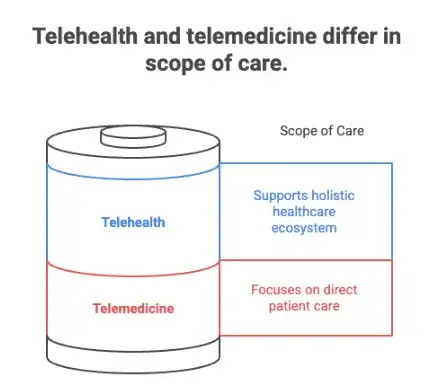
Telehealth aims to improve overall healthcare delivery, boost efficiency, and expand access, while telemedicine zeroes in on improving clinical care access specifically.
Telehealth’s broad mission is all about making care more convenient, affordable, and equitable. Virtual care, including telehealth services, has the potential to improve patient experience, outcomes, and system-wide efficiency, while reducing the cost and friction of in-person care.
Telemedicine’s goal is precise: delivering clinical care in a remote setting. Its growth has been driven by demand for accessible diagnosis, treatment follow-ups, and care continuity when patients can’t or don’t want to come into an office. Telemedicine helps clinics reduce no-shows, increase patient volume, and extend reach into underserved areas. When clinics integrate telemedicine with their workflows, they create a streamlined channel to deliver clinical care.
The image below highlights the main difference in terms of goals here:
What this means for hospitals and clinics
From the clinic or healthcare organization perspective, the difference is strategic:
- Telehealth programs give clinics a holistic toolkit for improving efficiency by feeding patient engagement pipelines, improving provider collaboration, and supporting non-clinical care initiatives.
- Telemedicine tools, on the other hand, directly align with clinical revenue goals. Virtual visits count as billable encounters, which allows for revenue continuity and better reach.
Combining both approaches offers the strongest value. Telemedicine secures revenue by delivering care; telehealth supports that care by improving engagement, education, and outcomes.
9. Telemedicine vs Telehealth: Patient Interaction
Telemedicine delivers direct, one-on-one clinical interaction: the kind of real-time appointments you're familiar with like virtual visits, live consults, or follow-ups.
Physicians engage directly via video or audio and make clinical decisions in real time. According to the 2024 Doximity State of Telemedicine report, 77% of physicians who use telemedicine do so at least weekly, and 35% use it daily, proving how deeply integrated it is in clinical workflows.
Telehealth can include interactions that don't involve real-time delivery. Patients might engage through patient portals, asynchronous messages, group webinars, or remote health tracking where data is collected over time and reviewed later. For instance, 44% of adults had multiple patient portals in use by 2022, though few people installed third‑party apps to consolidate them.
Here’s a summary of that difference:

What this means for hospitals and clinics
Clinics need to recognize this distinction. With telemedicine, patient interaction is live, clinical, and billable. With telehealth, interaction can be passive, educational, or non‑clinical, which adds engagement and support without necessarily needing real-time contact. Most modern clinics offer a mix: telemedicine for clinical care, and telehealth tools like portals or RPM to keep patients engaged outside appointments.
10. Telemedicine vs Telehealth: Strategic Value for Clinics
Telehealth helps modernize clinic operations, tighten up team collaboration, and deliver care more holistically, while telemedicine directly drives patient volume, reduces no‑shows, and expands clinical reach.
The strategic value of telehealth lies in its ability to transform patient engagement and internal workflows. Telemedicine, meanwhile, delivers measurable clinical impact by bringing revenue into clinics through virtual visits.
When offered consistently, telemedicine can reduce no‑shows, increase overall appointment volume, and extend reach into underserved communities. McKinsey’s analyses emphasize that more than 50 million in-person visits a year could potentially shift to virtual care if adoption were more evenly distributed across populations.
Here’s how that distinction works:
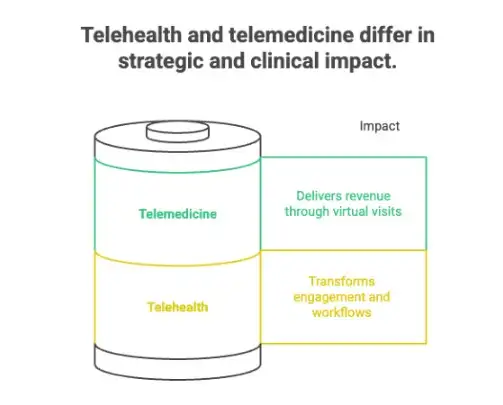
Why this matters for clinics & health organizations
For telehealth, you can deploy programs that automate patient outreach, support peer-to-peer provider training, and deliver educational content. These tools help streamline operations and keep teams in sync without adding patient visit overhead.
With telemedicine, the goals are more tangible: maintain or increase visit volume, reduce missed appointments, and tap into new patient segments. When integrated well with scheduling, EHRs, and care pathways, virtual clinical workflows can deliver revenue outcomes and improve access, especially in locations or populations where in-person care is harder to access.
How to Choose: Telehealth, Telemedicine, or Both?
Trying to figure out what’s right for your clinic? This quick checklist will help you match your goals, resources, and team setup with the right virtual care path so you can move forward with confidence.

1. What kind of care are you offering?
If your focus is on diagnosing, treating, and following up with patients, go telemedicine. But if you also want to offer coaching, education, or remote monitoring between visits, you’re in telehealth territory.
2. Is reimbursement a must?
Telemedicine services are usually billable through Medicare, Medicaid, and private insurers (with the right codes). Telehealth perks like education, outreach, or admin tools? Not so much, unless they’re bundled with a clinical service.
3. What’s your tech situation?
Already rocking a HIPAA-secure video platform and integrated EHR? You’re ready for telemedicine. Still building your digital toolbox? Start with lighter telehealth tools like messaging apps or RPM dashboards.
4. Who’s going to use it?
If it’s just your clinicians handling virtual visits, telemedicine gets the job done. But if nurses, care coordinators, or admin staff are in the mix, you’ll want the flexibility of telehealth.
5. What problems are you trying to solve?
Trying to boost visit volume or reduce no-shows? Telemedicine delivers. Need to keep patients engaged between visits or reduce manual outreach? Telehealth adds that support layer.
6. Want to reach more people?
Telemedicine helps you serve patients across locations. Telehealth helps you stay connected between visits, especially for underserved or high-risk populations.
Virtual is Best When It’s Also Smart
Telemedicine and telehealth are very useful tools. And like any tool, they only deliver value when you match them to the job at hand.
For clinics and healthcare organizations, the smart move is to get strategic. That means knowing when a secure video visit brings in billable care (telemedicine), and when a simple text or RPM tool keeps your patient engaged between visits (telehealth). It means seeing virtual care as a core part of how you serve, scale, and stay competitive.
So, what’s your next move?
- Start with your gaps: Where are you losing time, revenue, or patient trust?
- Then pick your path: Telemedicine, telehealth, or both?
- And don’t go it alone: The right partner can help you design a smart, compliant, and future-proof virtual care strategy.
You don’t need all the bells and whistles. You just need the right tools, used the right way, to deliver better care without burning out your team.
FAQ: Telemedicine vs Telehealth
What is the difference between telehealth and remote?
“Remote” simply means something is happening away from a traditional facility, like a patient being at home or a health care provider operating from a distant site. Telehealth is a more specific term that involves delivering healthcare using telecommunications technology, including clinical services, patient education, staff training, and even mobile health apps.
How is telemedicine different from telehealth?
Telemedicine refers specifically to clinical services, like diagnosis and treatment, delivered by a health care provider via secure digital channels. Telehealth, on the other hand, is a broader umbrella. It includes telemedicine plus services like remote patient monitoring, administrative communication, mobile health tools, and training. Telehealth policies also tend to cover both clinical and non-clinical care models.
What is virtual care vs. telemedicine?
“Virtual care” is a general term for any health service delivered through telecommunications technology. Telemedicine is a more targeted category within that, focused on direct clinical interactions between a patient and a health care provider, typically from a distant site.
Does telehealth always use Zoom?
Not at all. While Zoom is sometimes used, especially with proper compliance settings, telehealth can be delivered through many platforms that meet telehealth policy and security standards. These include HIPAA-compliant options like Amwell, Doxy.me, or systems integrated into electronic health records. The key is secure, private use of telecommunications technology.
Is telehealth available everywhere in the U.S.?
Technically yes, but real access depends on telehealth policies at the state level, internet access, and insurance coverage. Some states allow more flexibility for distant site providers or support wider use of mobile health services, while others limit reimbursement or provider eligibility.

