If you’re a clinic leader or healthcare exec trying to figure out whether to hire a Nurse Practitioner (NP) or a Physician Assistant (PA), you’re in the right place.
Because here’s the truth: most job descriptions won’t tell you: NPs and PAs aren’t interchangeable, and treating them like they are can cost you time, money, and operational headaches.
Both roles bring advanced clinical expertise, but their training, scope, billing models, and day-to-day impact on your team look very different. This guide breaks it all down.
MedPAC data shows that from 2010 to 2016, E/M office visits billed by Advanced Practice Providers (NPs and PAs) jumped 149%, and visits per patient with these providers grew faster than those with physicians. That kind of growth means hospitals and clinics are relying heavily on APPs. If you're hiring one, it better be the right one.
In this article, we’ll discuss:
- The real operational differences between NPs and PAs (beyond what their credentials say)
- A clinic-focused breakdown of training, autonomy, billing, and flexibility
- Tips on supervision, retention, and scope compliance
- A checklist of questions to ask before your next hire
- A strategic takeaway to help you staff smarter, not just faster
Let’s dive in.
What Are Nurse Practitioners?
Nurse practitioners (NPs) are advanced practice registered nurses (APRNs) who provide primary, acute, and specialty care services. They hold a master’s or doctoral degree in nursing and are licensed to:
- Diagnose conditions
- Prescribe medications
- Order and interpret diagnostic tests
- Develop treatment plans
They usually have a high level of autonomy.
In fact, in many U.S. states, NPs can operate independently without physician supervision, particularly in rural or underserved areas. This makes them a critical solution for expanding access to care, especially in telehealth, urgent care, and chronic disease management.
As such, NPs help reduce hospital admissions and improve long-term outcomes.
What Are Physician Assistants?
Physician assistants (PAs) are licensed medical professionals who diagnose illnesses, develop treatment plans, perform procedures, and prescribe medications under the supervision of a physician.
They complete a master’s-level PA program and are trained in the medical model. This means they’re highly versatile across specialties, such as emergency medicine, surgery, and internal medicine.
That’s why PAs are frontline providers, especially in fast-paced environments like urgent care clinics, hospitalist programs, and surgical teams. And since they can adapt to various roles, they’re very valuable in both in-person and telehealth settings.
While PAs generally practice under a supervising physician, many states allow flexible oversight, so PAs can expand care access and reduce bottlenecks in staffing.
Nurse Practitioners vs. Physician Assistants: Similarities at a Glance
While NPs and PAs follow different training paths, they can have overlapping roles in clinical settings. Here's how they align:
- Both complete rigorous graduate-level education and national certification before practicing.
- NPs and PAs diagnose conditions, prescribe medications, order tests, and manage treatment plans.
- Both can practice in primary care, emergency medicine, surgery, psychiatry, and more, on-site or via telehealth.
- In many states, both can work semi-independently, with varying levels of physician collaboration depending on local regulations.
Healthcare systems rely on both roles to expand access to care, reduce wait times, and manage high patient volumes. This is great especially during physician shortages.
Nurse Practitioners vs. Physician Assistants: Differences
Now that you understand the two roles and their similarities, let’s see the differences, too:
1. Nurse Practitioners vs. Physician Assistants: Training Background & Workflow Fit
When you're hiring for your clinic, the letters after someone’s name don’t tell the whole story. The real difference starts with how NPs and PAs are trained, which counts in how they fit into your day-to-day operations.
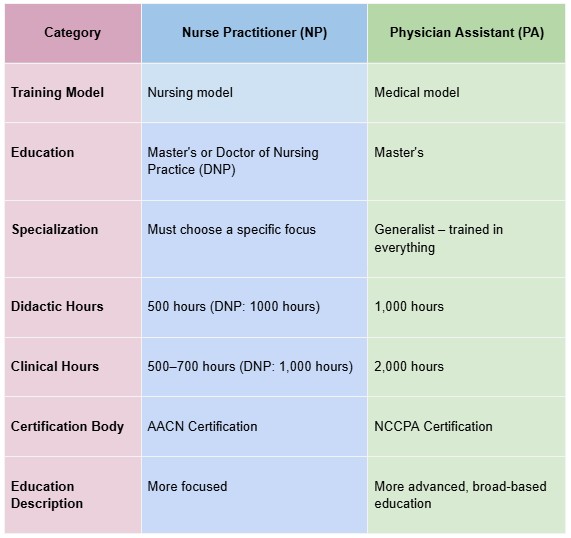
Nurse Practitioners (NPs) Training
NPs come up through the nursing world. They start as RNs, which means they’ve already spent years on the floor, managing patients, collaborating with care teams, and handling the human side of healthcare.
By the time they become NPs, they’ve logged at least 500+ hours of advanced clinical training (on top of their RN work). A lot of times, they specialize early in fields like family medicine, psych, or peds.
That makes NPs valuable in care coordination, chronic disease management, and patient education. They’re wired for holistic, continuity-focused care models.
Physician Assistants (PAs) Training
PAs take a different path. Their training mirrors med school, compressed into an intense 111-week program that blends classroom learning with clinical rotations across multiple specialties. As such, they complete over 1000 hours of clinical training.
Besides, they have a more generalist focus, which means they’re built for speed and adaptability. Plug them into physician-led workflows, and they’ll be able to handle it well. From urgent care to surgical support, PAs are generalists you can move around as needs shift.
What That Means for Your Clinic:
- Building a patient-centered care model with strong continuity? NPs are your go-to.
- Need flexible coverage across departments or a seamless fit with physician teams? PAs might be the better call.
- Want smoother onboarding? PAs tend to integrate faster into fast-paced, physician-led environments.
2. Nurse Practitioners vs. Physician Assistants: Specialization vs. Generalist Strategy
How NPs and PAs are trained affects how flexibly your clinic can use them.
Nurse Practitioners (NPs) Specialization
NPs don’t just “end up” in a specialty; they pick one from the start. Whether it’s family practice, peds, geriatrics, or psych, they build their training and clinical hours around that focus.
According to the American Association of Nurse Practitioners, 78% of NPs hold a Master’s degree, and nearly 18% have a Doctorate in Nursing Practice (DNP), with each path tailored to a specific patient population or setting.
That means when you hire an NP, you’re getting deep, specialty-aligned knowledge, which is great for clinics that rely on long-term patient relationships, chronic disease management, or niche care models like mental health or women’s health.
Pro tip: Read more about telehealth nursing trends to understand why licensure can be a distinct issue if you’re hiring NPs for telemedicine.
Physician Assistants (PAs) Specialization
PAs are trained differently. Their education is generalist by design, with rotations across internal medicine, emergency care, surgery, and more. The result? Close to 67% of PAs work outside primary care, filling roles in everything from dermatology to orthopedics to hospital medicine.
This makes them highly adaptable, perfect for multi-specialty practices, cross-coverage needs, or clinics that want the flexibility to shift providers between service lines as demand changes.
What That Means for Your Clinic:
- Need deep specialty coverage and long-term patient continuity? NPs are purpose-built for that.
- Need flexibility to move providers between urgent care, specialty clinics, or surgical support? PAs bring the versatility.
- Looking to scale fast with agile staffing? A PA’s generalist foundation gives you more options with fewer bottlenecks.
3. Nurse Practitioners vs. Physician Assistants: Operational Autonomy & Supervision Needs
NPs and PAs are governed by different oversight structures. And for clinics, that can either mean smooth sailing or a lot of extra admin work.
Nurse Practitioners (NPs) Autonomy & Supervision
NPs have been steadily gaining more independence. As of 2025, 34 states plus D.C. give NPs full practice authority (FPA), meaning they can diagnose, treat, and prescribe without needing a physician to sign off or supervise.
That means clinics in these states can:
- Schedule NPs solo without juggling physician availability.
- Reduce supervisory bottlenecks and compliance paperwork.
- Build more nimble, scalable care models, especially in rural, community health, or telehealth settings.
Physician Assistants (PAs) Autonomy & Supervision
PAs, by law, always need a supervising physician, no exceptions. That relationship has to be formalized with a collaborative practice agreement (CPA), which defines what the PA can and can’t do.
However, this supervision isn’t always direct:
Even though some states are relaxing those rules a bit, every state still requires some level of physician involvement, whether in person or remote.
That means:
- You’ll need to monitor how many PAs each physician is overseeing (some states cap it).
- Scheduling has to account for physician presence or backup.
- There’s a permanent layer of admin tied to oversight, renewals, and compliance logs.
What That Means for Your Clinic:
- Operating in a Full Practice Authority state? NPs give you staffing flexibility and lower supervision overhead.
- Staffing multiple PAs? Make sure your physicians have the capacity, and your admin team has the bandwidth, to manage compliance and collaboration.
4. Nurse Practitioners vs. Physician Assistants: Hiring and Onboarding
When it comes to rolling someone into your care team and making them productive fast, NPs and PAs follow different playbooks, and this has real implications for ramp time, retention, and admin burden.
Physician Assistants (PAs) Hiring and Onboarding
Trained under a medical-model curriculum, PAs typically slide into physician-led team structures with fewer orientation hurdles, so they reach full operational contribution faster. That’s because credentialing decisions and role delegation mesh more naturally with physician workflows.
That means your clinic gets:
- Quicker ramp-up to independent caseloads.
- Fewer orientation gaps around medical protocols and decision-making.
- Less friction in credentialing alignment with supervising physicians.
Even so, we don’t advise you to completely ignore onboarding.
Research shows that structured onboarding (for both PAs and NPs) directly improves engagement, retention, and clinical productivity.
Nurse Practitioners (NPs) Hiring and Onboarding
NP backgrounds vary. Some come from nursing that’s heavy on care coordination, others from acute settings. That diversity means onboarding needs to be customized, especially when you integrate NPs into physician-led models.
Evidence shows that onboarding programs that include clear expectations, mentorship, structured competency checks, and ramp-up timelines boost NP/PA job satisfaction and reduce early turnover.
Side note: Interested in hiring nurses for your healthcare organization? Here are 6 must-follow best practices for nurse recruitment.
What That Means for Your Clinic:
- If you need fast integration into physician-led teams, PAs onboard faster and align more tightly with existing clinical pathways.
- If your clinic relies on NPs’ specialized nursing background, be prepared to invest in structured onboarding that’s customized to bridge nursing and medical workflow norms.
- For both roles, clinics with clear onboarding programs see better retention, faster ramp-up, and less turnover headaches down the line.
5. Nurse Practitioners vs. Physician Assistants: Billing & Reimbursement Structures
How NPs and PAs bill for services impacts cash flow, revenue modeling, and payer navigation. Let’s break down what clinics really need to know.
Nurse Practitioners (NPs) Billing & Reimbursement
NPs typically bill using their own National Provider Identifier (NPI), but Medicare reimburses them at 85% of the physician fee schedule for identical services.
However, they can also bill “incident to” a physician under certain conditions. If all CMS rules are followed, that may qualify for 100% reimbursement. Still, this requires strict compliance (e.g., direct supervision, physician plan initiation), so many practices default to the standard 85% model.
Side note: Compensation is a bigger problem for travel nurses, but we’ve written an entire piece on travel nurse recruiting challenges that can help you make sense of it.
Physician Assistants (PAs) Billing & Reimbursement
PAs typically bill under a supervising physician’s NPI, which means services get reimbursed at 100% of the physician's fee schedule rate, the same as if the physician had done the visit themselves. That’s because their work may be billed as “incident to” the physician’s service, which Medicare and many payers pay at full rate.
This can reduce friction in multi-provider settings or shared services like procedure support, hospital consults, or team-based care models.
However, if PAs bill under their own NPIs, they get reimbursed 85%, just like NPs.
According to MedPAC, Medicare claims show that over 40% of NP visits and roughly 30% of PA visits for established patients are billed “incident to” a physician, so practices rely on these billing models more than you might expect.
What That Means for Your Clinic:
- Some insurers may credential NPs as independent providers more seamlessly than PAs, while PAs often align billing through group physician practices.
- PAs can boost per-service reimbursement by billing through physicians (when appropriate), while NPs offer autonomy and direct billing, though at a slightly lower rate.
- In short, go with an NP if you need billing autonomy and quicker onboarding. Choose a PA if you're optimizing reimbursement within a structured, physician-led team.
6. Nurse Practitioners vs. Physician Assistants: Turnover & Career-path Dynamics
Hiring is only half the battle. Keeping your providers long-term is what really protects your bottom line. NPs and PAs bring different retention profiles that can impact clinic planning, especially in high-churn environments.
Nurse Practitioners (NPs) Turnover and Career Development
NPs typically arrive with years of experience as RNs, which gives them a solid professional identity before they ever hit your clinic floor. That background usually translates into longer-term commitment and better retention. The current voluntary turnover rate for NPs seems to be 15% per year.
That RN foundation gives NPs:
- A clearer clinical identity and career purpose.
- Deeper ties to the healthcare system and culture of patient care.
- More resilience against burnout in primary care or high-volume roles.
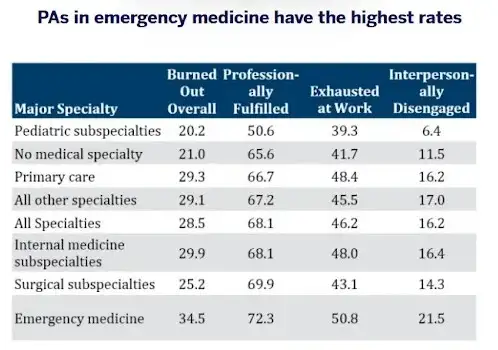
Physician Assistants (PAs) Turnover and Career Development
PAs jump straight into clinical roles after graduation, which can mean high agility but also high mobility.
A 2025 JAMA study found that 14.4% of new advanced practice providers (including PAs) leave their first job within one year, and 37% within five years (JAMA Network Open, 2025).
They also tend to shift specialties more often: 40.3% of PAs change specialties in their first decade, according to recent workforce data.
That’s probably because of high rates of work exhaustion according to AAPA:
What That Means for Your Clinic:
- Want better long-term retention? NPs offer more staying power, especially when they’re aligned with their specialty.
- Hiring new PAs? Be proactive about career development and role flexibility to keep them engaged.
- Have high churn? A structured onboarding and growth plan can reduce early exits, especially for new grads.
7. Nurse Practitioners vs. Physician Assistants: Scope Creep, Safety & State Variability
Scope of practice is a live factor in patient safety, operational risk, and how you structure your care teams across states.
Nurse Practitioners (NPs) Scope Creep
NP scope is defined by the state licensing authority. As of mid‑2023, 27 states, D.C., and two U.S. territories grant full practice authority (FPA) (remember, this means NPs can assess, diagnose, prescribe, and manage patient care independently under nursing board oversight with no physician collaboration required).
In the remaining states, NPs are tied to reduced or restricted practice models that may mandate collaborative agreements or supervision for certain care elements. And in some cases, NPs can be sued even for calling themselves “doctors:”
That means clinics must:
- Be aware of state-specific FPA rules that influence whether NPs can run autonomously or need physician oversight.
- Adjust staffing and responsibility allocation quickly if state laws shift: even modest legislative changes can alter how you deploy NPs.
- Factor in potential safe-practice caveats, especially in restricted/practice-limited states.
Physician Assistants (PAs) Scope Creep
PAs always operate under physician delegation. Each state defines what that means; some require in-person co-signatures, others allow remote supervision, and many set caps on how many PAs a physician may supervise simultaneously. Currently, 40 states impose limits on the number of PAs one physician can oversee at a time.
While some states have eased rigid requirements around co-location and chart review, medical oversight remains mandatory.
So for clinics:
- You need to track state-specific supervision rules, like who can sign off, how often, where the physician must be located, and how many PAs they can oversee.
- Oversight creep can introduce risk: when PAs practice beyond their written CPA, patient safety or credentialing issues can arise.
- Regular audits and clear documentation of delegations help prevent liability and scope overreach.
What That Means for Your Clinic:
- Navigating NP scope? Use FPA states to maximize autonomy; in restricted states, map NP responsibilities tightly to state rules and revisit post-legislation changes.
- Staffing PAs? Budget physician bandwidth and oversight carefully. State caps and supervision rules are real operational constraints.
- Want to avoid scope creep? Track CPAs closely, audit compliance regularly, and build clear escalation protocols.
8. Nurse Practitioners vs. Physician Assistants: Workforce Surge Planning & Flexibility
When patient volumes spike or service lines get stretched, how fast can your team adapt? NPs and PAs bring different levels of flexibility that matter big-time during surge planning.
Physician Assistants (PAs) Flexibility
PAs are trained as generalists, which makes them easy to move across departments without missing a beat. From urgent care to ER overflow or surgical support, they can plug in where needed.
This gives clinics:
- Operational agility during seasonal surges or unplanned absences.
- Lower need for retraining when coverage needs shift fast.
- A built-in backup plan for departments that see fluctuating volume.
Nurse Practitioners (NPs) Flexibility
NPs, on the other hand, tend to be more locked into their specialty. Whether it’s family practice, psych, or chronic care, their workflow is built for continuity and not necessarily for rapid reallocation.
That said, NPs excel at stabilizing long-term patient panels, which is just as critical during high-volume periods, especially when managing chronic conditions, care plans, or follow-ups.
What That Means for Your Clinic:
- Need someone you can shift across departments on short notice? PAs are built for that.
- Need consistency in patient relationships, chronic care, or specialty protocols? NPs bring continuity and stability.
- Facing seasonal volume spikes or staffing crunches? PAs give you flexibility without training overhead.
9. Nurse Practitioners vs. Physician Assistants: Team Dynamics & Organizational Culture
How NPs and PAs mesh with your team culture matters. Their differing roots influence communication style, collaboration, and fit within care models.
Nurse Practitioners (NPs) Team Dynamic
With deep nursing roots, NPs thrive in care settings that emphasize interprofessional teamwork, patient-centered rounds, and holistic, relationship-driven care.
And that’s great for patient care.
A 2023 systematic review in BMC Primary Care found that interprofessional collaboration (IPC), often including NPs, improved patient outcomes in 23 of 28 cardiovascular-risk studies, 8 of 18 elderly/polypathology cohorts, and most mental health trials.
More interestingly, nurse practitioners improve team collaboration.
A qualitative study reported that NPs routinely initiated collaborative interactions (like ‘brief knotworking’), making them centering figures in interdisciplinary teams, especially in acute or long-term care settings, across 384 hours and 1,284 observed interactions.
That means clinics where teamwork, education, and patient engagement matter see NPs as natural culture champions who help drive interdisciplinary care, peer communication, and patient-centered planning.
Physician Assistants (PAs) Team Dynamic
PAs integrate quickly into physician-led teams focused on diagnostics, procedure flow, and rotating specialty lines.
A case study of six UK hospitals found that PAs contributed to continuity, workload support, and freeing doctors for complex tasks, and were seen as safe, appropriate, and acceptable by physicians, nurses, and managers.
For clinics structured around physician-led protocols, fast assessments, or high-throughput diagnostics, PAs tend to slot cleanly into the existing culture and workflow with minimal adjustment.
What That Means for Your Clinic:
- Need strong collaboration, shared rounds, and a holistic care culture? NPs boost interprofessional teamwork and patient focus.
- Operate with physician-led systems, specialist rotation, or procedure-focused departments? PAs integrate seamlessly into that faster-paced, physician-aligned culture.
- Best outcome: clinics with mixed teams use NPs to strengthen team-based culture and PAs to amplify physician-aligned operations.
Real Talk: Questions to Ask Before Hiring
By now, it’s clear: NPs and PAs aren’t interchangeable. Before you post that job opening or make your next hire, run through these real-world questions to make sure you’re choosing the right role for the needs of your clinic.
.webp)
Scope & Autonomy
- Are we in a Full Practice Authority state for NPs, or will this role require physician oversight no matter what?
- Do we have the physician capacity to supervise multiple PAs, if needed?
Workflow & Setting
- Will this provider work in a single department (like primary care or psych), or do we need someone who can float across service lines?
- Is this role part of a team-based, interdisciplinary model, or a physician-led specialty team?
Patient Continuity vs. Flex Coverage
- Is long-term patient relationship continuity a core goal of this role?
- Or do we need someone who can jump into high-volume, procedure-heavy, or fast-paced environments?
Billing & Financial Impact
- Will we be billing independently under the provider’s NPI, or under a physician’s?
- How would reimbursement levels (85% vs. 100% of the Medicare fee schedule) impact our bottom line?
Onboarding & Retention
- Do we have a structured onboarding program in place?
- Is this a long-term hire, or do we need short-term flexibility with less emphasis on deep panel-building?
Wrapping It Up: Smarter Staffing Starts with Smarter Questions
Nurse Practitioners and Physician Assistants both bring serious clinical skills to the table, but they serve very different strategic functions inside a healthcare organization.
For clinic leaders, practice managers, and healthcare execs, the key takeaway is this: don’t hire reactively, hire intentionally. Think beyond credentials. Look at how each role fits into your care model, your billing structure, your state’s legal landscape, and your long-term growth plan.
Next step?
Audit your current provider mix. See where the gaps are. Then, revisit that “Real Talk” checklist before posting your next job. The difference between good staffing and great staffing often comes down to one thing: alignment.
And if you want to find the best APP for your healthcare organization 60% faster than the average industry benchmark, contact us today!
FAQ: Nurse Practitioners vs Physician Assistants
What’s the difference between a Nurse Practitioner and a Physician Assistant?
It comes down to training, scope, and fit. Nurse Practitioners (NPs) are trained under a nursing model, focusing heavily on patient education, chronic medical conditions, and developing treatment plans.
Physician Assistants (PAs), on the other hand, are trained under a medical model through Physician Assistant Studies, a rigorous program that mimics medical school and emphasizes diagnosing medical conditions, medical procedures, and working within physician-led teams. Both are licensed healthcare providers, but their clinical style and how they integrate into health systems are different.
Is a PA the same as an NP?
Not quite. While both are healthcare practitioners who can diagnose patient conditions, prescribe meds, and provide medical care, they’re built differently.
- NPs often specialize early and are tied to population-focused roles (like family or psych), working heavily in outpatient care centers or primary care.
- PAs are trained as medical generalists, rotating through general medicine, surgery, and emergency care. And while many NPs can practice independently depending on state regulations, PAs always require a medical doctor to oversee their clinical practice.
Can a PA perform surgery?
Yes, but not independently. PAs are trained to assist in surgical settings and often work in surgical specialties, supporting medical procedures like suturing, closing incisions, and prepping patients. They don’t replace a surgeon but are essential players on the surgical team, especially in high-volume or procedure-heavy clinics.
Which is more prestigious: NP or PA?
It’s less about prestige and more about alignment with your clinic’s model.
- In physician-led surgical specialties, PAs often carry more weight due to their medical training and clinical experience with procedures and diagnostics.
- In chronic care or patient-centered rounds, NPs may be more valued for their focus on care coordination, education, and long-term medical history management. Bottom line: it's about career goals, not rank.
Which role is better for diagnosing illnesses and creating treatment plans?
Both NPs and PAs are trained in diagnosing illnesses, conducting physical examinations, ordering diagnostic imaging, and developing treatment plans.
However, PAs typically handle more acute and procedural cases, especially in general medicine and specialty consults, while NPs tend to lead in chronic care management and preventive strategies.
Where do NPs and PAs typically work?
- NPs often staff outpatient care centers, community health clinics, and family practices.
- PAs are found everywhere, from ERs to surgical specialties to internal medicine teams. Their medical generalist training makes them versatile hires in diverse settings.
How do job growth and job outlook compare for NPs and PAs?
Both roles are surging. This kind of job outlook reflects their increasing role in solving provider shortages across all types of health systems.

