Night and weekend coverage remains one of the most persistent operational challenges for hospitals and imaging centers. When radiologists are unavailable after hours, emergency reads are delayed, patient flow slows, and quality of care suffers.
Recent data highlights the growing strain:
- The WHO projects a global shortfall of 11 million healthcare workers by 2030
- According to The Global Radiologist Report 2025, 63% of radiologists report that overnight work reduces performance and diagnostic accuracy.
- The same report notes that 53% identify radiologist burnout as their top professional concern.
For healthcare facilities managing around-the-clock services, these numbers underscore a serious issue. The shortage of radiologists, combined with the demand for immediate results, makes traditional staffing unsustainable.
Teleradiology offers a practical, scalable solution, delivering expert image reads during nights, weekends, and holidays without compromising turnaround time or accuracy.
In this article, we’ll dive into:
- Challenges of night and weekend coverage: staffing, fatigue, costs, and workflow gaps
- Impact on hospital operations: patient risk, workflow delays, and staff retention issues
- How teleradiology is beneficial and where it fits in modern care models
- Selecting the right teleradiology partner for reliable after-hours coverage
- Future trends: hybrid radiology models and 24/7 virtual reporting
P.S. Looking for trusted partners who can deliver reliable after-hours radiology support? Check out our detailed guide about Top Teleradiology Staffing Companies to explore top providers that can help you maintain seamless night and weekend coverage.
The Challenges of Night & Weekend Radiology Coverage
Night and weekend coverage in radiology remains one of the most difficult operational, clinical, and financial challenges for hospitals and imaging centers.
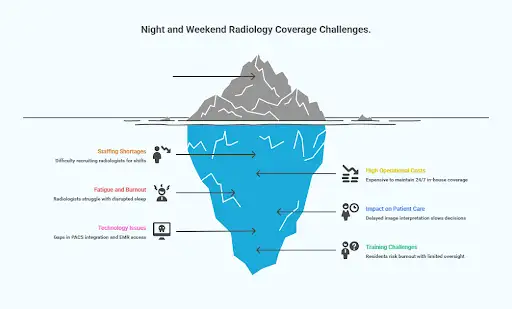
1. Staffing shortages
Recruiting and retaining radiologists for overnight or weekend shifts is increasingly difficult. The national shortage makes it even harder to sustain consistent after-hours coverage without overloading existing teams.
2. High operational costs
Providing 24/7 in-house coverage is expensive. One academic medical center reported spending $850,000 per year to maintain around-the-clock attending radiologist coverage, often for shifts that see limited use.
3. Fatigue and burnout
Radiologists working nights often struggle with disrupted sleep, stress, and reduced accuracy. Research links radiologist fatigue directly to higher diagnostic error rates. When daytime teams arrive at a backlog of unfinished overnight reads, it further compounds burnout and workflow strain.
4. Impact on patient care
Delayed image interpretation can slow emergency and inpatient decisions. One study found that CT turnaround times improved from over eight hours to just 1.4 hours after implementing full overnight attending coverage.
5. Technology and workflow issues
After-hours operations often reveal weaknesses in PACS integration, image transfers, and EMR access. When systems don’t communicate smoothly, radiologists may lose access to prior studies, patient histories, or referring physician notes.
These gaps increase the risk of delayed interpretations, incomplete reports, or diagnostic errors, especially in facilities using multiple unlinked platforms.
6. Training and supervision challenges
Teaching hospitals face an added layer of complexity during overnight shifts. Residents often handle urgent or complex cases when attending radiologists are unavailable for immediate review.
Limited oversight increases stress, heightens the chance of diagnostic mistakes, and reduces learning opportunities. Over time, this leads to burnout and weaker training outcomes for future specialists.
In short, staffing fatigue, high operational costs, and technological gaps combine to make night and weekend radiology coverage one of healthcare’s toughest problems to solve.
What happens if hospitals don’t know how to solve it?
How Poor Night and Weekend Radiology Coverage Impacts Hospitals and Patient Care
When night and weekend radiology coverage is weak or patchy, the problems aren’t abstract; they ripple across the hospital and affect patients, staff, operations, and finances.
Delayed Diagnoses & Patient Harm
Slow or missed imaging reads can lead to serious clinical consequences.
- In England, imaging errors and delays have been directly tied to avoidable operations and even deaths. Between 2021 and early 2025, the Parliamentary and Health Service Ombudsman (PHSO) upheld or partially upheld 45 cases involving failures in imaging, ranging from missed cancers to untreated infections
- According to the Royal College of Radiologists (RCR) analysis, nearly 976,000 scans in England weren’t reported within a month, violating national targets, and that’s despite millions spent outsourcing to solve the backlog
- Radiology is central to so many clinical pathways: as one paper notes, it features in four out of five patient pathways. That means delays in radiology tend to cascade downstream into surgical, oncologic, and emergency workflows.
In short, delayed or inaccurate reads slow down treatment, shrink windows for intervention, and compromise care standards.
Workflow Gridlock & Operational Stress
Weak after‑hours radiology coverage doesn’t just affect the night shift; it also overloads daytime operations.
- The morning team often inherits a backlog of overnight studies, many of which were only preliminarily read. That “catch-up” workload strains resources, delays elective cases, and crowds schedules.
- Turnaround times (TATs) rise sharply. For example, data from NHS England show that too many patients wait over four weeks for imaging results, which is a clear signal that capacity is outstripped
- Departments end up outsourcing just to keep up. In 2024, NHS trusts spent UK£325 million managing excess demand, with £216 million going directly to private teleradiology services.
- While outsourcing offers temporary relief, it’s not a sustainable fix. Costs escalate, integration challenges grow, and reliance on external systems deepens.
So the hospital might temporarily avoid a crisis, but it ends up paying for it elsewhere, through inefficiencies, staff strain, and fragmented care.
Financial, Reputation & Staffing Fallout
When radiology staffing coverage gaps persist, the consequences extend far beyond delayed reports; they affect the hospital’s bottom line, reputation, and workforce stability.
- Hidden costs vs. visible bills. The price of delayed diagnoses (e.g., longer stays, complications, readmissions) is often even more than what you think you’re losing. Also, outsourcing at scale becomes a huge budget line.
- Brand and trust risk. If your facility gets known for slow imaging turnaround or frequent diagnostic errors, clinicians might steer patients elsewhere, which means referrals drop and your reputation takes a hit.
- Staff burnout and turnover. Radiology teams, ERs, and inpatient services all feel the squeeze. Overloaded daytime staff, constant overtime, and strained working relationships can push clinicians to leave.
- Recruitment disadvantage. Top radiologists increasingly seek roles with flexible or hybrid coverage. Facilities that can’t offer balanced scheduling or reliable teleradiology support fall behind in attracting and retaining qualified talent.
Teleradiology: The Modern Solution for After-Hours Radiology Coverage
When you lay out all the challenges tied to night and weekend radiology coverage, teleradiology quickly shifts from a “nice to have” to a no‑brainer.
What is Teleradiology?
Teleradiology is the remote interpretation of medical images by qualified radiologists. Hospitals transmit scans securely to off-site specialists, who review the images and send back detailed reports, often in real time.
The tech behind it includes encrypted image transfers, integrated PACS and EMR systems, diagnostic-grade workstations, and quality control protocols.
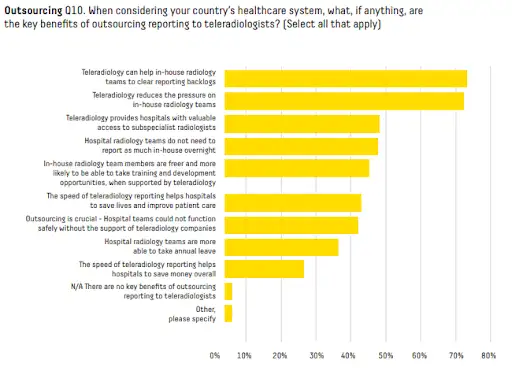
What started as a workaround for small or rural hospitals has become a core part of how many health systems handle after-hours and overflow demand. The same Global Radiologist Report mentioned earlier noted that 98% of radiologists now say teleradiology benefits their healthcare system, and nearly half of them say it reduces the need for overnight staffing.
How Teleradiology Solves the After-Hours Gap: Key Benefits
Teleradiology is most effective at night and on weekends, when in-house coverage is thin or unavailable. Hospitals can route late-night reads to teams in other time zones or to dedicated night shifts, without overtime or on-call rotations.
Faster clinical decisions
A public hospital system cut median report turnaround from >43 hours to 4.6 hours after adopting teleradiology, which reduced delays and improved patient satisfaction. This faster access to reports allows emergency and inpatient teams to make treatment decisions sooner, reducing overall length of stay.
Subspecialty access on demand
Hospitals gain immediate coverage for pediatrics, neuroradiology, MSK, and breast imaging at 3 a.m., without building those services internally. It ensures that even complex or time-sensitive cases receive expert interpretation when specialists aren’t physically available.
Backlog control and less burnout
Survey data show 73% of radiologists say teleradiology helps clear report backlogs, and 72% say it reduces pressure on internal teams. By shifting overnight reads off-site, in-house radiologists can focus on subspecialty work, education, and daytime priorities. This leads to lower fatigue and better retention.
Cost efficiency and predictable spend
Compared with staffing 24/7 in-house, hospitals avoid fixed costs for additional FTEs, benefits, workstations, and infrastructure while maintaining timely reads. Many providers offer flat-fee night and weekend coverage, which stabilizes budgets and limits surprise charges.
Flexibility and Operational Reliability
Teleradiology allows hospitals to scale coverage with demand—whether seasonal spikes, disaster recovery, or multi-site needs. Clear SLAs, credentialing standards, and integrated PACS/EMR workflows ensure consistent report quality. This reliability builds clinician trust and keeps after-hours reporting aligned with daytime standards.
.webp)
How You Can Implement Teleradiology Successfully
To make teleradiology work well, you need tight integration between systems, clear communication channels, and a strong commitment to quality control.
Images and reports need to flow cleanly between your local systems and remote. Prior studies, patient notes, and clinical context need to be available to remote readers; otherwise, you risk slow reports or errors. And with radiologists working remotely, strong SLAs and escalation paths are critical, especially for STAT or emergency cases.
Licensing and credentialing also matter. Radiologists must be certified to practice in the hospital’s state or country, and quality assurance needs to be built in, including peer review, double reads, and discrepancy tracking.
Lastly, technology needs to be rock-solid: from reliable bandwidth and high-resolution image quality to robust cybersecurity and consistent system uptime, there’s no room for system failures at 2 a.m.
Once your internal systems, workflows, and quality controls are in place, the next step is choosing the right teleradiology partner. A partner that aligns with your operational goals, clinical standards, and technology setup.
What to Look for in a Teleradiology Partner
Selecting the right teleradiology partner is make-or-break for night and weekend coverage. A mismatch can lead to delays, errors, frustration, or worse.
Below are the key criteria you should weigh:
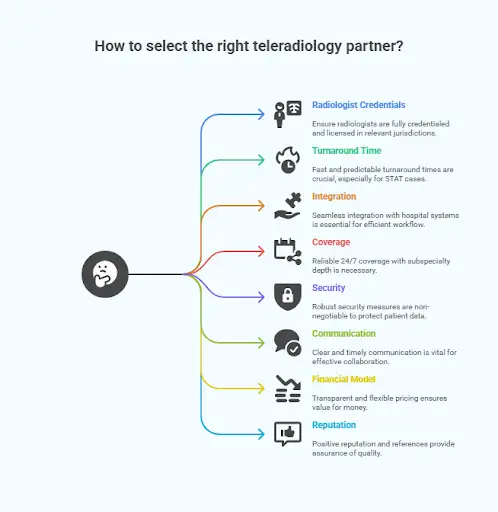
1. Radiologist Credentials, Licensing & Quality Assurance
First and foremost, every radiologist working your night/weekend reads must be fully credentialed, licensed, and board-certified in the jurisdictions where your hospital operates.
If you're crossing states or countries, make sure they meet those specific legal requirements. The American College of Radiology has published guidelines on legal/medico‑legal practices for teleradiology.
Quality assurance should be integral to any partnership. Look for structured peer review, discrepancy tracking, periodic audits, and double reads when necessary. Continuous performance feedback and transparent reporting are equally important.
The Royal College of Radiologists (UK) laid out standards requiring governance, reporting identity, and consistent QA in teleradiology.
Providers such as AAG Health follow these benchmarks closely, coordinating multi-state licensing, privileging, and credentialing while maintaining consistent peer review and discrepancy tracking to uphold diagnostic quality.
As a member of the American Staffing Association (ASA), we align our practices with national standards for compliance, ethics, and workforce excellence in healthcare staffing.
2. Turnaround Time (TAT) & SLAs for STAT Cases
Your teleradiology partner must deliver fast, predictable turnaround times, especially for STAT or emergency cases. When lives or critical treatment paths hinge on imaging, a “fast-ish” report won’t cut it.
Ask about their:
- Typical TAT for routine and emergent studies
- Hour-by-hour performance (overnight vs. daytime)
- Peak‑volume performance
- Escalation protocols when standards aren’t being met.
Also, check whether these SLAs are contractually guaranteed, with financial credits or penalties.
3. Integration & Workflow Compatibility
A good teleradiology partner should have a system that integrates cleanly with your PACS, RIS, EMR, and clinical decision systems.
- Reports and images should flow seamlessly back into your local systems with minimal manual intervention
- Prior studies, patient clinical notes, and imaging history should be available to the remote radiologist as though they were on site
- The handoff between in-house and remote radiologists (or between shifts) should feel like one continuous workflow
Remember, if data exchange is fragmented or inconsistent, delays and reporting errors can occur regardless of any SLA commitments.
4. Coverage & Subspecialty Depth
Your partner must be able to reliably cover nights and weekends. That means true 24/7 staffing (or shifting across time zones), not overstretching internal staff or outsourcing only parts of the schedule.
Also, check the radiologist's subspecialty competence. If your hospital handles neuro, pediatrics, MSK, nuclear medicine, cardiac imaging, or other niche modalities, your teleradiology partner must have specialists ready for after-hours cases. Without that depth, remote reports risk becoming safe but generic interpretations instead of true expert reviews.
5. Security, Data Privacy, and Compliance
With patient data flying back and forth, strong security is non-negotiable. Your partner must:
- Use robust encryption in transit and at rest
- Comply with all relevant data protection laws like HIPAA, GDPR, and national regulations
- Maintain audit trails and logging of access
- Have defined user access controls (who sees what)
- Undergo regular security audits and certifications (ISO 27001, or equivalent)
Your organization should also carefully check the partner’s policies for data breaches, incident response, and business continuity.
6. Communication, Support & Accountability
Even with perfect tech, remote reading demands close, trusted communication. Good partners offer:
- Clear protocols for urgent findings
- Easy and timely communication between radiologists and referring clinicians
- Transparent dashboards or reporting on performance (look at metrics like volumes, TATs, and discrepancy rates)
- A dedicated account manager or liaison for your hospital
- Rapid technical support, even in off-hours
When things go sideways, as they occasionally will, you want a partner who acts like part of your team instead of an outside contractor.
7. Financial Model & Flexibility
The best partners structure pricing so you pay for value and not unused capacity. Look for:
- Contracts that include nights & weekends in base or blended rates (not surprise surcharges)
- The ability to scale up or down based on volume, season, or growth
- Transparent pricing (per read, per modality, by service level)
- Exit clauses or smooth transitions if the partnership ends
8. Reputation, References & Track Record
Finally, you need evidence. A good partner will:
- Show you metrics from similar hospitals (like size, case mix, and off‑hours dependency)
- Share client references (especially for night/weekend performance)
- Be transparent about audits, past performance, and any service failures
- Meet standard guidelines and practices in your country or health system (e.g., RCR in the UK and ACR in the US)
The Future of Teleradiology in Healthcare
Teleradiology will continue to redefine hospital operations. Facilities that prepare early will gain faster diagnostics, stronger collaboration, and greater efficiency.
- AI-assisted reads: Advanced algorithms will pre-screen images, flag critical findings, and prioritize urgent cases so radiologists can focus on complex interpretation.
- Cloud-based infrastructure: Hospitals will move from local servers to secure, cloud-native systems that allow faster data transfer and seamless collaboration across sites.
- Real-time clinical collaboration: Radiologists will work more closely with telemedicine teams, joining live consults and remote treatment discussions when needed.
- Global coverage models: Cross-border radiologist networks will expand to maintain 24/7 coverage through time-zone alignment and regional licensing frameworks.
- Regulatory modernization: Licensing, credentialing, and data standards will evolve to support safe, compliant international reporting networks.
Hospitals that adopt these advancements early will improve turnaround times and strengthen radiology’s role as a central part of patient care.
Why Teleradiology for Night and Weekend Coverage Isn’t Optional Anymore
Relying solely on in-house radiology teams for night and weekend coverage is no longer sustainable for most hospitals and clinics, especially in the long run.
The pressure points are clear:
- Radiologist shortages
- Rising patient volumes
- Staff burnout
- Cost control demands
- Increasing quality expectations
Teleradiology helps you improve patient care, protect your staff, and stretch limited resources further. It brings in specialist talent when and where you need it. It smooths over the workflow friction that late-night reads used to create. And it helps organizations deliver timely, accurate reports without compromising quality, even at 3 a.m. on a holiday weekend.
Hospitals that thrive in the years ahead will be those that plan early and invest in flexible, integrated radiology models that support both patients and staff. That starts with asking the right questions, choosing the right partners, and ensuring your infrastructure adapts to changing demand.
Because in a world where every minute matters and every scan tells a story, there’s no room for delays when the lights are low.
Partner with AAG Health for Reliable Teleradiology Coverage
Teleradiology is no longer an optional backup plan; it’s an essential part of delivering consistent, high-quality diagnostic care. Hospitals that invest early in scalable, integrated radiology solutions will maintain faster turnaround times, reduce burnout, and protect both patient outcomes and operational performance.
As hospitals look for dependable partners to achieve those goals, AAG Health stands ready to deliver.
We keep your diagnostic care uninterrupted with board-certified teleradiologists who read across all modalities. Our team manages licensing, credentialing, and onboarding across all 50 states, ensuring your imaging flow never stops, even on nights, weekends, or holidays.
Partner with AAG Health to strengthen your radiology department, control costs, and ensure every scan receives the expert attention it deserves.
FAQs
What is teleradiology coverage, and why does it matter after hours?
Teleradiology coverage means having licensed radiologists remotely interpret scans when your in-house team isn’t available, especially nights, weekends, and holidays. It ensures 24/7 access to radiology services without overloading your internal staff.
How do teleradiology providers work with existing radiology groups?
Teleradiology is designed to complement, not replace, your local radiology group. Many hospitals use remote readers to cover overflow or off-hours shifts so their core team can focus on daytime volume and subspecialty reads.
Can teleradiology services handle subspecialty radiology cases like neuro or pediatrics?
Absolutely. Leading teleradiology providers like AAG/Health offer access to subspecialty radiology experts across modalities, including neuro, pediatric, MSK, and even interventional radiology consultations, depending on the setup.
Are remote radiologists held to the same standards as on-site ones?
Yes. Radiologists working in teleradiology services must be board-certified, fully licensed in your state or region, and follow the same clinical and legal standards as in-house staff, including QA protocols and peer review.
How fast can AAG Health provide credentialed teleradiologists for coverage?
AAG Health can quickly place fully credentialed, board-certified teleradiologists. With an average placement time of 55–90 days for physician roles, well below the industry norm, i.e, 90-120 days, we handle licensing, privileging, and onboarding efficiently so your coverage remains uninterrupted.
Does AAG Health offer nationwide teleradiology coverage?
Yes. AAG Health provides 24/7 coverage across all 50 states to ensure continuous reads during nights, weekends, and holidays. Our national network of credentialed radiologists reads across all major modalities, including neuro, MSK, and pediatric imaging.
What makes AAG Health different from other teleradiology providers?
We combine advanced data platforms, rapid credentialing, and a high-touch partnership model that prioritizes precision over volume. AAG Health focuses on placing mission-aligned clinicians who integrate smoothly into your systems and maintain long-term continuity of care.

