When talking about radiologist salaries in 2025, you have to remember that the raw average numbers on their own don’t tell the full story; this is just the tip of the iceberg. Clinics and healthcare organizations are grappling with rising demand, workforce gaps, and emerging technologies redefining how quality and cost are measured.
Imaging demand is set to grow by up to 26.9% by 2055, while radiologist supply may only increase 25.7%, which means the current shortage isn’t going anywhere unless you take action.
In this article, we go beyond headlines and help you build a smarter compensation and staffing strategy that aligns talent costs with your clinical needs and future vision.
Here’s what you’ll learn:
- Why base salary is only half the story and what costs really drive total compensation
- How specialty, location, and shift type reshape your salary strategy
- When AI and teleradiology create opportunities to do more with less
- What top candidates want beyond salary and how to stand out in a competitive market
- How to plan ahead when radiology demand spikes
Let’s get started.
1. Total Radiology Compensation Includes More Than Base Salary
The sticker figure for a radiologist’s salary, often quoted in the $450K–$550K range for permanent roles, and $500K–$650K for locums, is just the starting point. What clinics and healthcare organizations need to budget for is the true total compensation, which typically adds another 15–25 percent on top of base pay when fully loaded.
Why this matters:
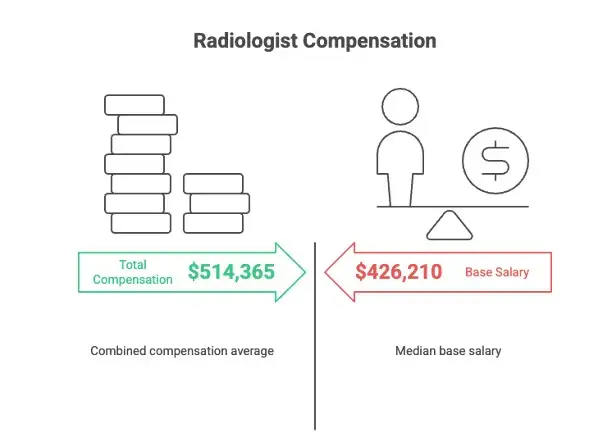
- Radiology Business found that performance bonuses alone can average $124,500 per radiologist, lifting total comp well above base levels. In one survey, the combined compensation averaged $514,365, substantially exceeding the median base of $426,210.
- According to this source, radiologists earn the highest hourly compensation among surveyed specialties (roughly $281 per hour), which suggests that, beyond salary, operational costs and productivity incentives are significant drivers of cost.
The graphic below breaks this down:
What gets added in practical terms:
- Signing bonuses (often $20K–$100K upfront) to attract talent in tight markets.
- Professional development perks like CME allowances, paid memberships, and license fees.
- Night-call differentials; particularly critical if 24/7 coverage is needed.
- Relocation packages to make geographic mismatches viable.
- wRVU/performance bonuses are directly tied to throughput or quality metrics.
If you want to avoid nasty financial surprises when hiring your next radiologist, make sure to factor in these additional costs and don’t focus on base salary alone.
2. The Radiology Subspecialty Drives Differences in Value
Not all radiologists cost the same, and in 2025, what they do matters just as much as how good they are.
The latest MGMA Provider Compensation Report shows that surgical and procedural specialists pulled in around $585,000 on average.
Meanwhile, more traditional diagnostic roles like body imaging and mammography are clocking in closer to $300K to $400K. That’s a huge spread, and it’s only growing as subspecialty demand heats up.
The image below breaks down this disparity
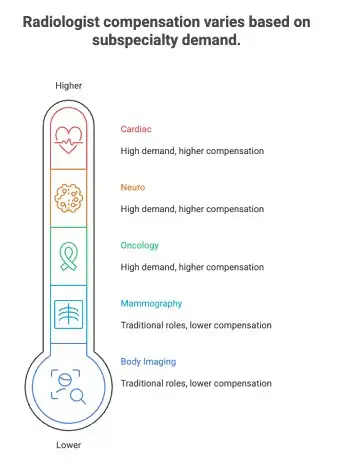
So if your clinic is building out oncology, neuro, or cardiac programs, your staffing budget should reflect those needs. Using “average radiologist” salaries as a guide is a fast track to sticker shock or worse, losing top candidates to faster-moving systems.
Ultimately, specialty drives price. Get clear on what skills your team actually needs, and plan your compensation accordingly.
3. AI & Workflow Tech in Radiology Changes Hourly Capacity
AI has a massive impact on radiology. Instead of slogging through stack after stack of scans, radiologists now serve as expert supervisors of AI-prepared reads. In many operational settings today, routine cases are being triaged and drafted by AI, effectively shifting human oversight into higher-value, clinical decision-making roles.
Here are hard numbers from respected studies:
According to a pilot study published on arXiv in late 2024, AI-generated draft reports helped drop average reporting time from 573 seconds to 435 seconds per study, a 24% reduction, with no loss in diagnostic accuracy.
What this means in real terms for your clinic:
Instead of hiring more radiologists to keep up with volume growth, you can:
- Cover the same scan volume with fewer FTEs by shifting low-acuity cases to AI supervision.
- Or get more reporting output per FTE, boosting your throughput without increasing headcount.
- Redeploy human talent to interpret complex cases where clinical judgment matters most, and drive better value.
Put another way: staffing models based on legacy reads or hourly assumptions are increasingly outdated. With workflow efficiencies fueled by AI, healthcare organizations can negotiate smarter contracts where they pay for radiologist oversight instead of raw reading volume.
4. Teleradiology as a Budget Lever
Teleradiology is a proven financial lever for clinics and health systems that want to control costs and streamline coverage.
A recent analysis shows that outsourcing night and weekend radiology coverage through teleradiology can reduce imaging service costs by 50–63% compared to maintaining in‑house staff.
For many hospitals, those savings come not only from lower staffing costs (like in this analysis). More importantly, you can also expect reduced burnout and fewer errors associated with overworked on‑call teams. That’s becoming more important as 69% of radiologists report understaffing in their organizations.
Beyond staffing relief, cost savings are real. Analyses of NHS-backed programs in the UK show that contracting with external teleradiology providers can drive annual radiology service costs down by about 25 percent compared to traditional in-house staffing—and in some cases deliver up to 50 percent savings versus using locum cover.
Without needing to dock the value of round-the-clock reporting or subspecialty availability, teleradiology lets organizations shift expensive premiums away from in-house anchor doctors, especially for after-hours or weekend coverage. You’re essentially paying only for output, not idle capacity or infrastructure maintenance.
This flexibility is especially powerful if you're operating outside metro centers or managing fluctuating scan volumes. Outsourcing can help fill weekday night shifts, weekend gaps, or holiday backlogs at a fixed, usage-based rate, without any long-term PSA commitments or fixed clinician salaries.
Use teleradiology as a strategic staffing and budget tool, so your organization can keep clinical service up and premium costs down. That way, your internal radiologists can focus on higher-value cases and operational priorities.
Pro Tip: Want to see how cost-effectiveness in radiology is actually calculated? This short explainer walks through the basics of measuring costs. Use the same framework to assess whether teleradiology can be a good lever in your healthcare organization:
5. Radiology Burnout and Shift Costs Ripple into Retention
More than just a wellness issue, burnout has real financial consequences for healthcare facilities, and night shifts play a big part in that.
According to a global survey published in Radiology Business, 47% of radiologists say working night shifts reduces their diagnostic accuracy. Even worse, 63% report negative effects on their performance and patient care, with 61% experiencing impaired performance the following day.
Meanwhile, Medscape data shows burnout is widespread: in 2022, 54% of radiologists reported burnout symptoms, up from 49% the year prior. This highlights the persistent stress that affects not only individual physicians but organizational health, too.
Of course, certain radiology specialties tilt the balance in the other way, which makes burnout even worse for the most affected radiologists.
These issues translate directly into retention risks. A systematic review published in BMJ covering 170 observational studies found that physicians experiencing burnout are three to four times more likely to regret their career choice or consider quitting, and their productivity drops significantly. For organizations, that means turnover costs, not just the salary itself, must be baked into staffing strategies.
So what's the bottom line? High burnout driven by night shifts and heavy workload means clinics face:
- Increased turnover and recruitment costs
- Lower radiologist performance per shift
- Greater risk of clinical errors, slower throughput, and disrupted service quality
The graphic below shows some of the hidden costs of burnout:
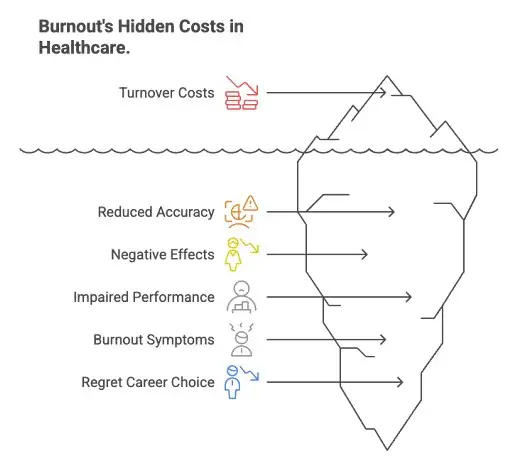
Here’s what this means for salaries: if you're managing staffing budgets, make room not only for high salaries, but also contingency for burnout-related churn and overtime. Long-term solution? Tackling shift distribution, workload balance, and scheduling flexibility can reduce burnout and avoid high-cost turnover cycles.
6. Urban vs Rural Pay & Incentive Tradeoffs in Radiology
Salaries for radiologists often seem more appealing in metro areas, but total costs (like benefits, housing, and retention strategies) can actually outpace what you'd spend in a well-designed rural program.
Analyzing MGMA data and nationally vetted surveys, here's what we see:
According to a New England Journal of Medicine-linked analysis based on MGMA’s compensation survey data, primary care doctors in non-metro areas earned a median of $205,588, only slightly above the $200,000 median in metro areas, suggesting base compensation doesn’t swing wildly once cost-of-living is accounted for.
But for specialists (like radiologists), the differences are far more pronounced: the same survey noted median guaranteed pay of roughly $320,000 in metro regions versus about $250,000 in non-metro surgical specialties.
This disparity isn’t always a disadvantage for clinics. Many rural and underserved regions counteract lower base pay by offering substantial incentives, especially in the form of loan repayment programs. For example, analyses of the AMGA survey published in NEJM Career Center show that loan forgiveness offers to non-urban physicians typically average $75,000, with top-tier packages reaching $100,000 or more.
Compared to urban systems, which often cover relocation and modest bonuses, rural loan incentives can be more financially impactful. That’s especially true for early-career or debt-burdened candidates.
For healthcare organizations, particularly those looking to staff oncology, imaging, or advanced diagnostic services, here’s what to consider:
- While base salaries in rural areas may look lower, generous loan repayment incentives can significantly outweigh the metro premium.
- Urban hires often involve higher retention packages, housing allowances, and relocation support, which can drive up your real cost per clinician by 10–20% beyond base pay.
- For smaller systems or those in underserved regions, combining a modest base salary with strong incentive structures can deliver a competitive total package and attract candidates who value long-term flexibility and financial cushioning.
In short, urban-rural tradeoffs aren't just about geography; they’re about strategy. Decide whether you're competing on base salaries or smart-for-service incentives, and structure your comp models accordingly.
7. Locum vs Permanent Radiologists: Hidden Upsides and Downsides
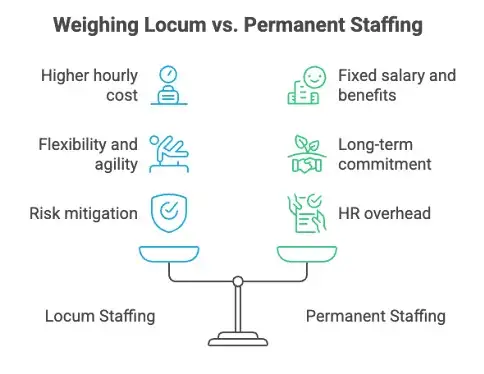
At first glance, locum tenens roles might seem pricey, and many annualized estimates push up to the $600K–$650K range in high-demand specialties like radiology. Yet despite that headline, the true value of locum coverage comes in the form of flexibility, risk mitigation, and staffing agility.
A reliable data point from AMN Healthcare reveals that nearly 90% of hospitals and medical groups used locum providers to maintain services while searching for permanent staff during the past year. This widespread adoption speaks to the strategic utility of locums as a built-in buffer against hiring delays and staff turnover.
On the pay front, locum radiologists can earn more per hour: one survey indicates that locum physicians generally make about $32.45 more per hour than their permanent counterparts. While that adds up quickly in gross pay, it’s balanced by removing the burden of benefits, malpractice coverage, pension contributions, and long-term retention costs.
So what does that mean for your organization?
Where permanent staff involves fixed salary, benefits, onboarding, and ongoing HR overhead, locum arrangements let you pay only for hours delivered. You’re not running the risk of covering unused capacity during slow periods or losing millions in revenue from unfilled shifts.
In many cases, using locum radiologists for holiday shifts, weekend coverage, or short-term spikes can actually be more cost-efficient than stretching permanent staff or paying higher premiums to local anchor doctors. And if volumes stabilize, you still have the option to recruit permanent hires without being locked in financially.
In short: locums come at a higher hourly cost, but remove long-term expense and workforce uncertainty, which makes them a savvy short- or mid-term staffing tool for facilities that want flexibility without sacrificing coverage.
8. Equity & Pay Transparency Trends in Radiology
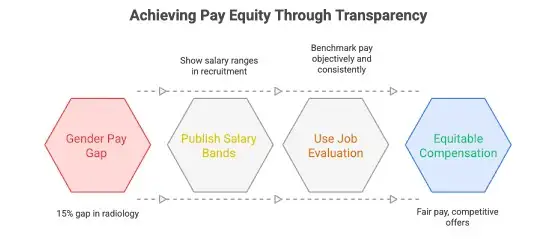
Gender pay gaps are narrowing, but up to 15% in interventional radiology is still too wide, especially as pay transparency becomes part of your employer brand.
Gender Pay Equity in Focus
According to a 2024 peer-reviewed study published in Academic Radiology, intersectional analysis revealed that female assistant professors in interventional radiology earn up to $75,000 less than their white male counterparts, which equates to a gap of about 15% in total compensation.
However, the study doesn’t explain whether this gender pay gap is due to systemic gender discrimination; factors like moonlighting and years of experience may also contribute to this disparity.
Transparency on the Rise
From a global corporate audit by Aon, 69% of organizations now publish salary bands during recruitment, and 44% use consistent job evaluation frameworks to benchmark pay objectively. These moves signal that structured pay information has moved from being an optional nice-to-have to an expected condition, especially by equity-focused candidates.
What that means for clinics and systems:
If your organization promotes salary transparency or structured pay bands, especially for high-demand subspecialty roles like IR, you’ll not only improve fairness but also make your offers more competitive and credible.
Clinics that work to close gaps and publish clear compensation structures send a strong signal to candidates: your system is inclusive, transparent, and merits pay that matches performance.
In the following graphic you can see how healthcare facilities can more towards more equitable pay:
9. Predictive Workforce Planning Is Key in Radiology
Radiology demand is advancing faster than the available workforce, and that mismatch can leave clinics scrambling or overspending unless you plan ahead.
A recent census by the Royal College of Radiologists found that UK CT and MRI scan volumes grew by 8% in 2024, while the radiology consultant workforce increased just 4.2%, deepening the existing supply-demand gap. That imbalance is projected to worsen, with consultant shortfalls expected to hit 39% by 2029, threatening capacity and timely care.
Looking further ahead, the Neiman Health Policy Institute’s analysis projects the U.S. radiologist supply will grow by only 25.7% between 2023 and 2055, but imaging demand is forecast to rise by 17% to 27% over the same period. That means the current shortage isn’t closing; it’s likely to persist unless residency positions expand or imaging utilization stabilizes.²
What this means for hiring orgs and finance teams:
Predictive staffing is now essential. To build proactive budgeting and avoid costly catch-up moves:
- Model projected scan volume growth with inflation, demographic shifts, and program expansion in mind.
- Factor in retirements and attrition, especially as pandemic-era burnout accelerates exits.
- Layer in AI-based efficiency gains, raising capacity per FTE as workflows evolve.
- Base hiring calendars on future needs, not historical headcounts alone.
When radiology organizations plan with real foresight, they can avoid reactive premium pay cycles, reduce reliance on pricey locum coverage, and better justify strategic AI or talent investments. This kind of proactive modeling turns a staffing costs risk into a business outcome that you can control.
What to Include in a Competitive Offer (Beyond Salary)
If your only lever is salary, you're playing a limited game. In 2025, the best radiologists, especially subspecialists, are weighing total compensation, work-life balance, and practice quality just as much as the dollar figure.
Here’s what top-tier offers are bundling in to stay competitive:
1. Loan Repayment or Forgiveness
Especially powerful for early-career radiologists. Programs offering $75K–$100K+ in loan relief are increasingly common in non-metro systems, according to NEJM Career Center.
2. Flexible Shifts or Scheduling Autonomy
Burnout is real. Radiologists value autonomy over shift patterns, options for hybrid work, and reduced night-call load, sometimes more than raw pay increases.
3. Structured Reporting Systems
Clinics that provide structured templates and AI drafting tools cut report time and error rates. That boosts radiologist productivity and improves job satisfaction, a low-friction benefit with a high upside.
4. AI-Enabled Workflow Support
Tech-forward systems that triage, pre-read, or automate follow-ups attract radiologists who want to focus on clinical value, not grunt work. It also shows your clinic is investing in the future.
5. CME and Career Development Stipends
Annual budgets for continuing education, conference travel, or board prep show you're committed to clinical excellence, not just coverage.
6. Signing and Retention Bonuses
Still effective, but best used alongside long-term incentives or milestone payouts to promote retention, not just fast recruitment.
7. Relocation Assistance and Onboarding Perks
Especially critical in rural or relocation-heavy roles. These perks smooth the transition and show that your organization supports physician wellbeing from day one.
8. Performance Incentives Tied to Quality, Not Just Volume
Shift the bonus model from raw wRVU to outcomes or peer-reviewed quality, which aligns better with modern expectations and reduces burnout.
See the image below for a visualization of these tips:

The most successful hiring organizations think beyond the paycheck. They create packages that speak to what radiologists really want: things like clinical support, personal balance, and long-term value. In a tight talent market, it’s these details that make your offer stand out.
AAG Health Can Reduce Your Radiology Hiring Costs
The reality is that radiologist salaries are rising, and shortages are only making the market tighter. But you don’t have to shoulder those costs alone. AAG Health helps hospitals and imaging centers reduce the financial and operational strain of radiology hiring by delivering board‑certified, fully credentialed radiologists when and where you need them.
Instead of absorbing the hidden costs of long hiring cycles, overtime, or locum premiums, AAG Health’s network of pre‑vetted professionals allows you to:
- Fill staffing gaps faster: Avoid revenue loss and patient backlogs by accessing radiologists ready for immediate placement.
- Cut recruitment overhead: Skip lengthy searches, credentialing delays, and high agency fees with AAG’s streamlined process.
- Match the right fit: Our candidates are screened for both clinical expertise and cultural alignment, improving retention and lowering turnover costs.
- Stay flexible: Whether you need short‑term coverage, after‑hours shifts, or permanent placements, AAG provides scalable solutions.
With AAG Health as your staffing partner, you’re controlling salary inflation, protecting margins, and ensuring uninterrupted patient care.
Conclusion: Make Every Dollar Count
Radiologist salaries are rising, but so is the complexity behind them. It’s no longer about matching a number from a compensation survey. It’s about building a smarter, more strategic compensation model that reflects your clinic’s needs, patient volume, tech stack, and long-term goals.
Whether you're a rural facility trying to stretch your budget or a specialty clinic competing for top-tier subspecialists, the winning approach isn’t just about paying more; it’s about paying smarter. That means knowing when to use locums, how to structure incentives, and how AI, burnout, and reporting workflows all shape your cost-per-outcome.
Your next radiology hire should fit into a broader staffing strategy that scales with your care model and your budget. If you’re still planning salaries in a vacuum, it’s time to zoom out.
Contact AAG Health today to discuss your staffing needs and see how we can reduce your radiology hiring costs while improving patient outcomes.
FAQ: Radiologist Salaries in 2025
What type of radiology pays the most?
Among all subspecialties, interventional radiology (including locum tenens NIR radiologists) consistently earns the highest compensation, often $500K–$650K+. Other high earners include Neuro Radiology and Breast Radiology, especially in private practice or high-volume hospital settings.
How can hospitals and healthcare systems attract better radiologists?
Competitive pay matters, but top talent looks for more: flexible schedules, clear contract negotiations, sign-on bonus, structured reporting tools, AI-supported workflows, and incentives that drive up Net Income. For hospital systems, offering these benefits, especially in less saturated geographical locations, can be a strong draw.
How do you know how much to pay your radiologists?
Use a current radiologist salary guide like MGMA or AAMC to benchmark by specialty, region, and setting. Salaries vary by:
- Metropolitan areas (typically higher base but also higher costs)
- Facility type (e.g., radiology group vs hospital-owned)
- Role type (e.g., locum tenens diagnostic radiologists vs full-time)
Don’t forget: total compensation includes more than just salary: it often runs 15–25% higher once bonuses, benefits, and night-shift differentials are factored in.
How much do radiologists get paid in the US?
Across the board, U.S. radiologists typically earn $450K–$550K in base pay for permanent roles. Locum tenens diagnostic radiologists may see annualized comp reaching $600K–$650K, especially when covering urgent care or hard-to-fill shifts.
What makes contract negotiations with radiologists different?
Radiology contracts often involve more complexity than other roles. Compensation may be tied to wRVUs, night shift premiums, subspecialty demands (like Abdominal Radiology or Neuro Radiology), and whether they’re joining a Private Practice or a hospital-employed group. Understanding benchmarks and aligning expectations around Net Income and call responsibilities is key.
How does geographical location affect radiologist pay?
In metropolitan areas, salaries tend to be higher, but so are living costs and retention challenges. In contrast, rural or underserved regions often offer loan repayment, relocation assistance, or flexible schedules to offset lower base salaries. Understanding the tradeoff between location and total compensation helps optimize your offer.
Where can clinics find qualified radiologists to hire?
In addition to referrals and recruiter networks, top-performing clinics are turning to medical career websites, residency program job boards, and partnerships with leading radiology groups. For niche roles like Breast Radiology or locum tenens NIR radiologists, it’s critical to advertise in the right corners of the medical community.

