Imaging demand is exploding. But the number of radiologists? Not so much. Health systems are already feeling the pressure, and the worst may still be ahead.
For hospitals and clinics running staffing, hiring, and operations, this is urgent. If you want to survive this, you need strategic moves.
That’s why we’ll share with you practices we use in-home when hiring radiologists for our clients.
We’ll discuss:
- How to build a ready-to-go radiologist pipeline before gaps appear
- Ways cross-training ER and ICU teams can smooth demand surges
- What perks actually draw top radiology talent and keep them
- How teleradiology can be used smartly to scale, not scramble
- How to make radiology a board-level patient care priority
You’ll also get a clear view of where the field is heading, and a sharp “what you should do next” snapshot to turn insights into action, starting now.
Radiologist Shortage Statistics: The Current Picture
The radiologist shortage is real and the numbers prove it.
Demand vs. Supply
- Imaging volumes are expected to grow 3–4% annually, while workforce growth remains constrained by retirements and training bottlenecks.
2. In the U.S., the Harvey L. Neiman Health Policy Institute projects that by 2055:
- The number of radiologists will grow by about 25.7%, from around 37,500 in 2023 to ~47,100, if residency slots stay flat.
- Meanwhile, imaging demand is expected to climb by up to 26.9%, driven by population aging and chronic disease, keeping the workforce shortage firmly intact.
- If imaging demand rises toward the higher end of projections (~26.9%), even a 40.3% increase in radiologists may be insufficient to close the gap.
Workforce Demographics & Pipeline
- In 2023, approximately 37,482 radiologists were actively seeing Medicare patients.
- About 32% of radiologists are aged 55 or older, signaling significant retirements ahead.
- Radiologist attrition has surged: rates increased by 50% since 2020, according to The Imaging Wire.
- Only 29 new PGY‑1 diagnostic radiology slots were added nationally from 2021 to 2025 as per The Imaging Wire. This highlights the slow expansion of the training pipeline.
- In the 2025 residency match, 961 diagnostic radiology applicants and 247 interventional radiology applicants went unmatched, according to Diagnostic Imaging data.
Workforce Distribution & Burnout
- The U.S. has roughly 13 radiologists per 100,000 people, with wide variability (e.g. some states like OK, NV, MS, WY have as few as 9 per 100k), states Diagnostic Imaging.
- About 50% of radiologist job openings in 2023 remained unfilled, as per Diagnostic Imaging.
- 46% of radiologists report burnout.
Broader Impacts & Specialties
- Interventional radiology is among the top 5 specialties facing the steepest physician shortages, partly driven by demand growing 1.5 - 2 X the national average in states like California.
- In the UK’s NHS, every radiology unit surveyed in 2024 missed waiting‑time targets due to staffing shortages. This can lead to delayed cancer diagnoses and treatment starts, with each month of delay increasing mortality risk by ~10% .
How to Fight the Radiologist Shortage
Now that we’ve seen the dangers of the radiologist shortage, it’s time to see how to fight it.
1. Build a Radiology Bench, Not Just a Role
Don’t wait for wave after wave of resignations or volume surges before you react. Instead, proactively build a pipeline of pre-vetted, on-call radiologists like locum tenens, teleradiology partners, and part-time clinicians. That way, when demand spikes or someone leaves, you’ve already got skilled clinicians in ready-to-go positions.
Why this matters for healthcare leaders:
- Instant coverage: Instead of wasting resources when someone quits or takes leave, pre-credentialed professionals can step in without delay.
- Flexibility when it counts: Use locums or telerads to manage after-hours or weekend surges without burning out your permanent team.
- Cost control through preparedness: With more predictable temporary coverage, you’re less likely to overpay under time-sensitive hiring pressure.
Pipeline setup best practices:
- Develop long-term agreements with locum or teleradiology firms (not spot contracts).
- Keep a shortlist of reliable part-time or remote radiologists who are familiar with your systems.
- Establish credentialing and onboarding readiness so that backups are scanned into your PACS and EMR systems.
- Track usage trends. If backlog or leave-of-absence events spike, lean on your bench before turning to costly last-minute hires.
By investing early in a well-stocked radiology bench, hospitals can transform coverage gaps into contingency strategies and avoid service breakdowns before they happen.
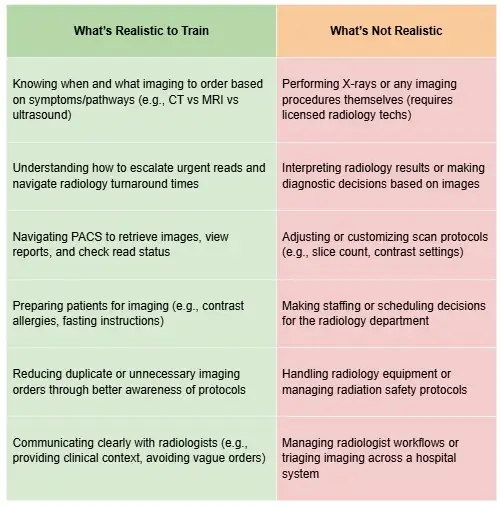
2. Invest in Cross‑Department Imaging Fluency
Train non‑radiology staff, especially in departments like the ER, ICU, and surgical units, on core imaging workflows to reduce unnecessary handoffs and lighten the load on your radiology team. This builds smoother coordination, better triage, and faster throughput when radiologist hours are tight.
Why this matters:
A study found that only 26% of radiology departments felt their operational capacity could meet growth in imaging volume over the next 2–3 years. The rest either need to consider locum tenens, teleradiology, or train other teams to step in to keep things moving.
How implementing this tip helps:
- Fast‑track intake: ER or ICU staff trained to tag studies by urgency and prep patients correctly (e.g., contrast protocols or positioning) helps speed up radiologist reviews downstream.
- Prevent idle time: When non‑radiology providers can coordinate scans and communicate directly with technicians, it smooths scheduling, which reduces repeat or delayed exams.
- Build mutual understanding: Training builds empathy and smoother communication across teams, which in turn eases friction during high‑pressure shifts.
Tips for rollout:
- Offer modular training. This can include short workshops or video tutorials on topics like MR/CT prep, contrast protocols, and basic anatomy for better triage.
- Designate key individuals (e.g., ICU nurse leads) as imaging “liaisons” who maintain expertise and act as go‑to contacts.
- Track imaging turnaround times (TAT), scan repeat rates, and ED length‑of‑stay, before and after training, to measure and quantify any gains in efficiency.
By upskilling key clinicians outside radiology, hospitals can break down bottlenecks and absorb pressure more gracefully, even when radiologist staff are stretched thin.
3. Prioritize Smart Triage for Imaging Orders
When imaging orders come in faster than they can be read, the real risk isn’t just backlog. It’s missing the most urgent cases in the noise. Implementing smart triage systems, whether manual protocols or AI-assisted tools, helps radiologists zero in on high-priority, high-impact studies first, instead of burning time on routine reads.
The results are obvious.
- A European Radiology review of AI-based triage tools found that using AI to reorder radiology worklists cut average report turnaround times (RTAT) by up to 43.7% for certain conditions like stroke, chest disease, and pulmonary embolism. Without worklist reordering, the improvement was just 7.6%.
- In another study focused on chest X-rays for pneumothorax, AI-prioritized worklists slashed RTAT from 80.1 minutes to 35.6 minutes, more than a 50% reduction in time to diagnosis.
Why this matters for healthcare leaders:
- Keeps the most critical cases from getting lost in a sea of routine imaging.
- Improves emergency department efficiency by speeding up diagnosis for acute conditions.
- Makes better use of radiologist hours by filtering out low-urgency reads during high-demand periods.
Here’s a good template for radiology triage:
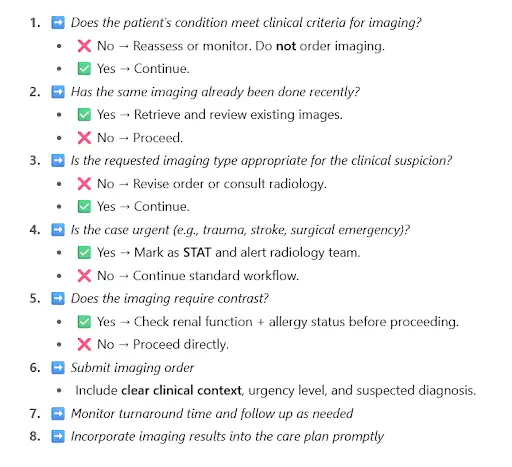
Pro tip: Start by piloting triage tools in high-volume or high-risk areas like chest CT, stroke imaging, or trauma cases, and then scale based on measurable results like RTAT and admission delays.
4. Rethink Compensation Beyond the Paycheck
Radiologists are in high demand, and they’ve got options. If your offer starts and ends with a salary number, you’re already behind. Flexibility, remote-read capability, and a real voice in department decisions are what make talent stick.
- A study published in Academic Radiology found that flexible work arrangements and remote options were top drivers of job satisfaction. This is especially true among early-career and female radiologists.
- McKinsey’s workforce insights show that more than 50% of U.S. employees would prefer a flexible or hybrid model, even if it means less money. Flexibility is now a core part of the value proposition, not just a perk.
Why this matters for healthcare leaders:
- Remote-read options give you access to talent outside your zip code and help retain staff who need schedule control.
- Flexible shifts and creative scheduling reduce burnout and appeal to radiologists juggling family, academic, or research commitments.
- Influence matters: radiologists want a say in tech, workflows, and staffing. Give them a seat at the table, not just a spot on the schedule.
Pro tip: Don’t just ask what it’ll take to hire a radiologist. Ask what it’ll take to keep them. That’s where the real competition is.
5. Build Partnerships with Academic Programs
Want a better shot at hiring top radiology talent? Start before they hit the market. Partnering with med schools and radiology residency programs gives you early access to up-and-coming clinicians and positions your hospital as the place they want to land.
In fact, a McKinsey report found that strong health system–university partnerships help address long-term staffing gaps quite well. And it does so by aligning education with real-world care delivery needs, especially in high-scarcity fields like radiology.
Why this matters for healthcare leaders:
- Get early exposure to residents and med students and let them get hands-on with your systems, team, and workflows.
- Build loyalty before the competition shows up with externships, part-time reading gigs, and mentorship opportunities.
- Shape future-ready staff by collaborating with program directors on curriculum updates that match your tools, tech, and protocols.
Pro tip: Don’t just treat academic partnerships like a future hiring funnel. Use them to strengthen your brand, support clinical education, and give your senior radiologists a chance to teach, mentor, and lead.
6. Use Teleradiology Strategically, Not Desperately
Some healthcare facilities treat teleradiology as a panic button, but this is wrong. Teleradiology trends show that this is a worthwhile strategy that should be part of your long-term plan. When used intentionally, teleradiology takes pressure off your in-house team, speeds up turnaround, and gives you access to subspecialists without blowing up your payroll.
The numbers prove it.
In a 2025 global radiologist survey, 73% said teleradiology is critical to clearing backlogs, and 72% said it helps reduce day-to-day workload stress. Nearly all (98%) agreed it improves hospital operations overall.
Its effectiveness is why the global teleradiology market is projected to grow at 13.2% annually, climbing from $7.5B in 2023 to over $20B by 2032. Of course, staffing gaps and growing imaging demand are also probable drivers.
Why this matters for healthcare leaders:
- It adds breathing room. Offload routine or after-hours reads so your internal team can stay sharp for complex, high-impact work.
- It scales with you. Have coverage ready for volume surges, vacations, or sudden exits.
- It protects your people. Consistent overnight coverage means your team doesn’t burn out.
Pro tip: The best telerad setups feel like an extension of your in-house team. Prioritize providers that integrate well with your systems, offer consistent readers, and commit to your quality standards.
7. Level Up Your Tech Stack With Radiologist Input
If you lock radiologists out of the software decision process, the tools you pick could end up slowing them down, breeding frustration, or even sending them packing. Involve them early, and you'll equip your department with tools that boost speed, accuracy, and loyalty.
One example here is PACS, which stands for Picture Archiving and Communication System. It’s the software that stores, retrieves, and displays medical images like X-rays, CTs, and MRIs… basically the tech backbone of radiology.
- A KLAS 2025 report on PACS systems highlights that ongoing customer satisfaction is tied to strong vendor support and active product development. Labs that listen to user feedback retain happier, more efficient clinicians.
- A multi-center survey of 1,518 clinicians in the UK showed that 83% said PACS benefited their work, and 79% preferred it over traditional film, which shows how key tech can be when deployed well with user input.
Here’s how PACS works:
Why this matters for healthcare leaders:
- Efficiency scales with usability. If radiologists can’t customize their viewer or reporting workflow, productivity dips and dissatisfaction rises.
- Input builds investment. Radiologists who shape their tools are more likely to adopt AI workflows, triage tools, or reporting aids faithfully. And the impact of AI in radiology is increasingly evident.
- Better tech = faster reads. When tools are intuitive and integrated, radiologist throughput improves and burnout drops.
Pro tip: Conduct a tech review panel with radiologists before signing any vendor contract. Their needs, from viewer layout to AI flagging tools, should inform your technology roadmap.
8. Audit and Fix Imaging Workflow Bottlenecks
A radiologist shortage puts weak spots in your imaging process into sharp relief. Now’s the time to pinpoint where scans stall, where delays sneak in, and overhaul the workflows before they break your system.
- A simulation study of an academic trauma center found that reducing imaging delays and bundling as few as 10% of imaging orders significantly shortened patient time in the ED, easing pressure across departments.
- McKinsey operational research highlights how capacity utilization and variability can create exponential increases in waiting times. They found that even minor inefficiencies can ripple into major bottlenecks across hospital workflows.
Why this matters for healthcare leaders:
- Find the choke points: Whether it's schedule gaps, prep delays, or unclear communication protocols, bottlenecks expose hidden inefficiencies.
- Free up radiologists: Streamlined intake and coordination mean radiologists spend more time reading and less time chasing information or correcting process errors.
- Shorter stays and smoother flow: When imaging moves faster, ED and inpatient throughput improve, which helps the whole institution run better.
Pro tip: Set up a cross-functional task force. Include radiology, ED, techs, and scheduling coordinators, and map the full imaging pipeline from referral to reporting. Use real data (like wait times, scan repeats, communication delays) to prioritize fixes with the highest impact.
9. Add Imaging Metrics to Executive Dashboards
Make radiology data a core part of your leadership dashboards so executives see where the squeeze is and can act proactively. You should be tracking turnaround times, backlog levels, read-report errors, and even repeat scans. This approach keeps staffing, funding, and workflow decisions data-driven.
But many healthcare organizations still lag: a survey revealed only 24.3% of hospitals use executive dashboards across facilities to guide strategic decisions. The rest stick to local or departmental metrics, which means they can miss the big-picture opportunities to act before things go off the rails.
Why this matters for healthcare leaders:
- Clarity leads to action: When execs can see backlog trends, TAT changes, or rising error rates, they’re more likely to authorize overtime, hiring, or tech investments.
- Smart staffing decisions: Real-time metrics let leaders anticipate where to lean in with locums, remote readers, or cross-training before shortages become crises.
- Improved accountability: Transparent dashboards help align radiology performance with broader hospital goals and make staffing and quality issues visible at the top.
Pro tip: Go beyond static dashboards. Use intelligent alternatives that flag anomalies like sudden TAT spikes. Then, suggest concrete steps, such as redistributing workload or expanding contract coverage.
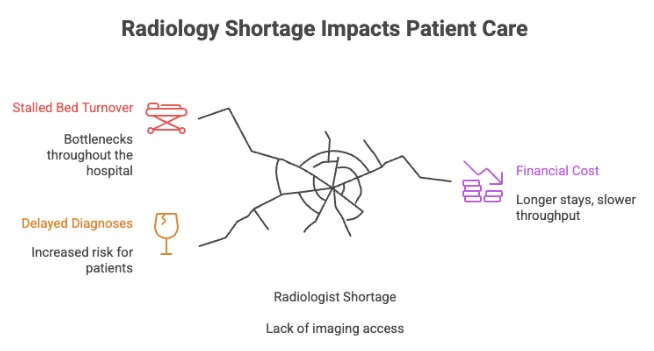
10. Frame Radiology Strategy as a Patient Care Issue
The radiologist shortage is a patient care crisis waiting to happen. When imaging access slips, diagnoses stall, length of stay balloons, and patient outcomes suffer. Framing radiology as a core clinical function instead of a support service earns executive buy-in and faster action.
- A study of over 20,000 emergency medical admissions found that longer imaging turnaround times were independently associated with longer hospital stays and higher costs. This shows you the clinical and financial damage of delays in the radiology department.
- A recent acute medicine analysis found that nearly half of patients with same-day scans and no abnormalities were discharged within 24 hours. Delays in imaging directly impacted the length of stay and throughput in acute units.
Why this matters for healthcare leaders:
- Delayed diagnoses increase risk, particularly for time-sensitive conditions like cancer or stroke.
- Bed turnover stalls, creating bottlenecks throughout the hospital.
- Financial and reputational cost rises, which means longer stays, slower throughput, and frustrated clinicians and patients.
Pro tip: When you’re asking execs for resources, whether hiring funds, tech investments, or workflow redesign, make it about patient impact metrics rather than just staffing numbers. Tie radiology access improvement to goals like shorter inpatient stay, faster admission throughput, and safer clinical outcomes. Those arguments are stronger and more likely to hit home.
What’s Next in Radiology Staffing?
If you’ve been reacting to the radiologist shortage, it’s time to start getting ahead of it. Here are three trends that forward-thinking healthcare leaders should have on their radar now, not five years from now.
AI Isn’t Just for Triage Anymore
Radiology AI is moving beyond basic prioritization. AI-generated draft reports can shave down radiologist reporting time dramatically: one pilot study dropped average reporting from 573 seconds to 435 seconds, with no impact on clinical accuracy. New tools can:
- Auto-detect and highlight abnormalities in real time
- Generate structured report drafts to speed up dictation
- Identify incidental findings that might otherwise get missed
Why it matters: These tools don’t replace radiologists; they make their work faster, safer, and more consistent. But only if your systems and workflows are ready to support them.
Virtual Training Pipelines Are Emerging
Med schools and residency programs are starting to experiment with:
- Remote radiology rotations
- Virtual mentorship networks
- Cross-state licensing pipelines for remote reads
Why it matters: Institutions that tap into virtual training networks can build relationships with top talent before they graduate or even before they apply for residency.
Predictive Staffing and Workload Modeling
New scheduling and analytics platforms are using predictive modeling to:
- Forecast radiologist workload by season, modality, and shift
- Recommend ideal staffing mixes (on-site, remote, per diem)
- Trigger alerts when backlog thresholds are at risk of being breached
Why it matters: This turns staffing from reactive fire-fighting into proactive planning, which is especially critical for high-volume imaging departments.
Final Takeaway: Radiology Shortage, or Strategy Shift?
The radiologist shortage is a pressure test for how adaptable your organization really is. Leaders who treat this as a pure staffing problem will stay stuck in reactive mode, always scrambling to fill gaps.
But if you see it as an opportunity to rethink how imaging is staffed, supported, and integrated into broader hospital strategy, you will come out ahead.
Your next move? Pick one area, like tech, triage, telerads, or training, and start there. Bring in your radiologists, map the bottlenecks, and make one high-leverage change this quarter. Then build from it.
Because at the end of the day, imaging isn’t just one department. It’s the heartbeat of diagnostic care, and your ability to staff and support it will shape patient outcomes, clinician retention, and operational resilience across your entire system.
Need a partner who can help you move from reactive to strategic?
Alpha Apex Group Health specializes in high-impact radiology staffing and systems support. If you’re ready to take the first step, reach out to our team and let’s build your next-level imaging strategy together.
FAQ: Understanding the Radiologist Shortage
Is the U.S. healthcare system facing a radiology workforce shortage?
Yes, big time. The gap between imaging demand and radiologist supply is widening. Population growth, aging patients, and rising diagnostic imaging requests (like CT scans) are all driving this trend. And with attrition rates among radiologists rising and limited expansion in graduate medical education, the supply isn’t keeping up.
How can Alpha Apex help if we’re facing a radiologist shortage?
Alpha Apex provides rapid access to experienced, pre-vetted radiologists, including teleradiology support and subspecialty coverage. That way, you can maintain diagnostic continuity without overloading your in-house team. We can help whether you need short-term gap coverage or long-term partnerships, without compromising quality or turnaround times.
How did the COVID-19 pandemic affect radiology services?
The pandemic accelerated burnout, delayed training for radiology trainees, and disrupted residency pipelines. Many older radiologists left the field early, increasing reliance on locum tenens radiologists and further straining the system. On the flip side, it fast-tracked adoption of teleradiology and clinical decision support tools.
Can AI and clinical decision support replace radiologists?
No, but they’re great assistants. AI is helping triage CT scans, flag urgent cases, and even draft reports. Clinical decision support systems are also reducing unnecessary imaging utilization. Together, they increase efficiency, but human expertise, especially in interventional radiology and nuanced diagnosis, remains irreplaceable.
Is radiology still a good career path for medical students?
Definitely. With strong demand, diverse subspecialties (like cancer cases, neuro, MSK), and growing integration with surgical and diagnostic teams, radiology remains a high-impact, future-proof specialty. That said, medical education and residency training programs need modernization and expansion to meet current workforce needs.
What are healthcare systems doing to adapt to the radiology shortage?
Forward-looking hospitals are:
- Cross-training nurse practitioners and physician assistants to support imaging workflows
- Building relationships with medical schools to engage future talent early
- Using teleradiology to fill gaps with vetted, off-site professionals
- Tracking imaging metrics to guide smarter staffing and workflow decisions
- Investing in workforce growth tools like predictive scheduling and AI triage

