Quiet quitting happens across all industries, but it’s also showing up across hospitals, clinics, and corporate healthcare offices alike. What starts as quiet disengagement typically turns into higher employee turnover, delayed patient rounds, and rising risk to patient care.
The ripple effects touch everything from staffing ratios to HCAHPS scores. That’s why you need numbers you can present in the boardroom.
In this article, you’ll get fresh 2025 data on how deep the problem runs, which departments are most affected, and how your metrics compare to others. Let’s start by looking at the key statistics.
Key Quiet-Quitting Statistics
Quiet quitting is no longer limited to a few burned-out employees. It’s now a measurable trend across the healthcare workforce. These numbers show just how widespread disengagement has become and why it demands your attention.
Here are the key statistics that define the state of quiet quitting in healthcare for 2025:
- 50% of U.S. employees are now considered “not engaged” at work, a group the organization defines as quiet quitters.
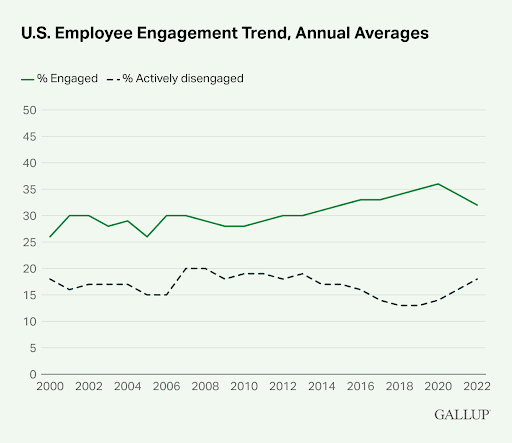
- According to Gallup, employee engagement in the U.S. fell to about 31% in 2024 (the lowest in a decade) while the share of actively disengaged workers, or “loud quitters,” held steady at 17%.
- Gallup’s 2024 State of the Global Workplace report indicates that just 21% of employees worldwide are engaged, while 62% are not engaged and 17% are actively disengaged.
- The decline in global employee engagement led to $438 billion in lost productivity worldwide.
- The American Hospital Association projects a shortage of up to 3.2 million healthcare workers in the U.S. by 2026.
- 67% of nurses are showing signs of quiet quitting by sticking to only their basic duties.
- In the Press Ganey 2025 Healthcare Employee Experience report, physician engagement has declined by 0.06 points on a 5-point scale.
- Press Ganey’s 2025 report finds that trust, respect, and belonging (not pay) are the top drivers of engagement and retention.
- A recent global study highlights record-high levels of burnout among nurses, with serious implications for patient safety and the sustainability of healthcare systems.
- According to The 2025 State of Internal Communications report, half of employees say they’ve spent periods only meeting minimum job requirements.
Healthcare Quiet-Quitting Statistics
Quiet quitting in healthcare is now backed by measurable trends across job categories and clinical roles. These figures show where employee disengagement is spreading fastest and what impact it’s already having.
Here are the latest statistics shaping your response strategy.
11. In a study of healthcare professionals in ResearchGate, 57.9% were identified as quiet quitters and only 42.1% as engaged.
The study revealed a clear engagement gap, with nearly six in ten healthcare professionals now identified as quiet quitters. That means most of your clinical and support teams could be disengaged while still on the payroll. This silent drop in effort can severely affect organizational performance and patient satisfaction scores.
12. A survey by Workvio found that 57% of frontline clinicians reported not being fully engaged at work.
More than half of frontline clinicians reported being disengaged at work to some degree. This percentage is higher than the national average across industries, and highlights a serious risk for hospitals relying on bedside care roles. Disengaged frontline staff can reduce the speed and quality of nursing care, and that can directly impact patient recovery times.
13. According to Gallup, healthcare worker engagement dropped by 7 points, and almost the entire decline involved engaged workers moving into the “not engaged” category.
Engagement among healthcare workers dropped, with most shifting from engaged to not engaged. That shift doesn't always show up in performance reviews but usually results in reduced initiative and weaker team collaboration. Over time, it strains leaders already trying to maintain consistent staffing and care delivery.
14. The study of 1,760 healthcare professionals in ResearchGate identified 67.4% of nurses as quiet quitters (those doing only the bare minimum) compared to 40.3% among other healthcare workers.
This discrepancy shows how heavily nursing personnel are affected, especially in units with high acuity and minimal staffing buffers. Quiet quitting in nursing usually looks like skipped rounding, shorter patient visits, or reduced mentoring of junior staff. These habits slowly erode team function and leave nurse leaders with fewer reliable go-to team members.
Pro tip: High quiet-quitting rates among nurses show why recruitment can’t rely on old tactics. Here are six practices that can help you reach, hire, and retain nurses in today’s environment.
15. The same study found quiet quitting rates of 53.8% among physicians.
These rates suggest a tiered disengagement pattern, with clinical license holders showing higher withdrawal than non-clinical staff. That’s typically due to higher exposure to emotional exhaustion and less perceived flexibility in roles. For you, this means support efforts can’t be a general approach. Physicians and nurses need different re-engagement strategies to address their distinct stress points.
16. A 2025 report by NCSBN states that 39.9% of RNs and 41.3% of LPN/VNs intend to leave the workforce or retire within the next five years.
The intent to leave at this scale is a workforce crisis in motion. These rates reflect more than people’s retirement age. Some unresolved turnover intentions are driven by chronic fatigue, workplace politics, and pay compression. Waiting to intervene until exits begin will leave you scrambling to replace roles that take months to backfill.
Pro tip: Losing nurses is a morale and a budget problem. To learn what turnover actually costs, read our guide on 38 statistics on the true cost of healthcare recruiting and retention to see how to factor it into your 2025 workforce planning.
17. Press Ganey data indicate that physician engagement is rising modestly from a 5-point scale score of 3.98 to 4.00 year-over-year.
While this small uptick may suggest some stability, it's not enough to drive real change. The slight improvement could reflect isolated policy wins or wellness programs, but not system-wide engagement. Without structural changes to organizational culture, burnout and disengagement will continue to linger just below the surface.
18. Sermo found that 79% of physicians believe their health systems are not effectively recognizing or addressing quiet quitting among healthcare providers.
This shows a wide perception gap between leadership intentions and staff experience. When physicians feel unseen, they usually reduce effort without warning by skipping team meetings, avoiding extra consults, or delaying charting. If you’re not using pulse surveys or feedback tools to measure sentiment, you’re likely underestimating the need for organizational support.
Pro tip: Physicians who feel unseen tend to disengage faster. Our guide on seven physician recruiting strategies can help you build teams that stay aligned and committed longer.
19. According to the same Sermo report, 43% have cut their documentation down to the bare minimum, while 37% have scaled back their patient-contact hours.
These aren’t policy violations because the legally required minimum still gets done. However, they’re quiet shifts in behavior that affect patient throughput, billing, and compliance. Reduced documentation also leads to charting gaps that can slow audits and impact reimbursement. For hospital finance and quality teams, this creates downstream burdens they may not be equipped to handle.
20. Sermo also found that 43% turned down leadership roles, and 37% skipped optional professional development to avoid extra duties.
Essentially, these patterns reveal an aversion to visibility and growth, which limits your ability to build next-gen leadership. When experienced staff pull back from stretch roles, you lose key succession options. That leads to over-reliance on a few remaining high performers, which raises the risk of quiet firing due to unbalanced workloads.
21. The report from Sermo also notes that 45% now limit after-hours patient communication, while 42% feel less empathetic because of burnout.
These behaviors reflect withdrawal from the emotional labor side of care, something your organization’s metrics may not always capture. As empathy fades, so does patient satisfaction, care continuity, and staff reputation. If your teams are already stretched thin, this kind of emotional retreat can directly damage healthcare services delivery and outcomes.
Pro tip: This erosion of empathy isn’t just among physicians. CRNAs also report disengagement tied to recognition gaps. If that's happening in your teams, this guide can help you get the recognition you deserve as a CRNA.
22. Gallup reports that the ratio of engaged to actively disengaged U.S. employees dropped to a decade low of 1.8:1 in 2022, before modestly improving to 2.1:1 in 2023.
Even with the small recovery, this ratio is still dangerously low. That means for every two engaged workers, one is actively working against the grain and creates friction in team dynamics and morale. Without quick adjustments to work attitudes and recognition systems, that friction will stall performance during critical operational periods.

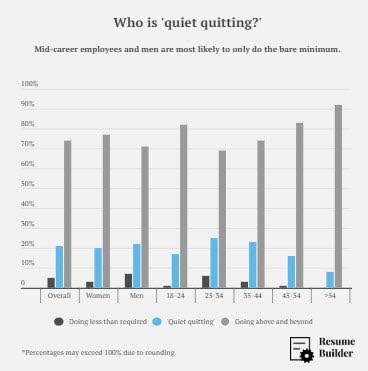
23. ResumeBuilder found that 21% of workers described themselves as “quiet quitting” by doing only the bare minimum, and a further 5% admitted they were doing less than even that.
The data shows that some employees are beyond disengaged but actively checked out. In healthcare, that’s where errors, missed labs, and communication breakdowns begin. It’s also where the quality of work life deteriorates for peers who are left covering the gap in effort.
24. ResumeBuilder also discovered that mid‑career staff aged 35-44 are most likely to quietly quit at a rate of 24%, compared to just 17% among workers under 25.
This mid-career withdrawal is especially risky because these are usually team leads, mentors, or department anchors. Their disengagement disrupts onboarding continuity, peer learning, and morale. If your culture isn’t set up to retain this group, you’ll soon face compounding losses in both headcount and person‐organization fit.
Healthcare Quiet-Quitting Drivers, Risk Factors, and Impact
Disengagement rarely happens without cause. In healthcare settings, it's usually triggered by exhaustion, poor recognition, toxic dynamics, or long-term misalignment with values and leadership. These patterns are measurable, preventable, and in many cases, fixable.
Here are the latest statistics that explain why quiet quitting is happening and where your biggest risks may lie.
Pro tip: If you’re tracking disengagement, you’ll need to stay ahead of broader workforce shifts, too. These 61 HR stats for 2025 give you a clearer picture of what’s changing now.
25. One study found that emotional intelligence protects nurses by reducing quiet quitting, turnover intention, and job burnout.
When nurses can regulate stress, manage conflict, and communicate effectively, they’re more likely to stay engaged even under pressure. That’s why some systems are investing in leadership coaching or resilience workshops tailored for clinical teams. You can strengthen nurse retention by prioritizing emotional intelligence development within team training cycles.
26. Quiet-quitting correlates with higher burnout and elevated turnover risk across all roles.
Disengagement typically begins with emotional fatigue and ends in resignation. What you’re seeing as quiet quitting now may soon lead to exits across nursing, allied health, and administration. If you aren’t actively addressing burnout rates, you’ll face growing gaps in staffing and rising cost-per-hire later.
27. A study of health professionals working in public hospitals revealed a strong association between burnout and disengagement across all roles.
This link cuts across departments, showing that no function is immune, not even ancillary services. When burnout becomes embedded in your hospital environment, even top performers lower their effort to cope. That’s why burnout should be monitored with regular engagement surveys and tied directly to department-level action plans.
28. According to ResumeBuilder, 83% of employees who do the bare minimum and 88% of those who do even less say they feel at least somewhat burned out, compared to 71% of overachievers.
These numbers show that reduced effort isn’t always about attitude but typically about capacity. Quiet quitters may be protecting themselves from further job burnout because they’ve seen what overexertion leads to. The solution lies in redesigning workflows and care models to allow for sustainable output without eroding team morale.
29. Organizations with strong workplace cultures average around 85% engagement and see better retention and performance.
That level of engagement doesn’t happen by accident. It reflects years of investment in values, people practices, and leadership alignment. If your organizational culture isn’t being shaped intentionally, it will default to silence, burnout, or turnover. High-functioning teams are a product of high-trust systems with built-in feedback loops.
30. Gallup reports that disengaged employees would switch jobs for a 22% raise, while engaged workers need about 31% to do the same.
That 9-point gap represents how much engagement acts as a buffer against attrition. If your team feels ignored or undervalued, they’re more likely to leave for modest pay bumps. To protect employee retention, focus on intrinsic motivators like autonomy, peer recognition, and visible support from managers.
31. Wider research shows that toxic work environments and ongoing conflicts increase the likelihood of quiet quitting.
Tension between coworkers or a lack of psychological safety drives people to pull back from contributing fully. Over time, that damages collaboration and leads to workplace conflict cycles that erode trust. Clear conduct policies, conflict resolution training, and manager accountability all help interrupt this spiral.
32. Disengaged nurses are significantly more likely to plan on leaving their jobs than their engaged peers.
This is one of the clearest signals for future staffing shortages. If you track engagement closely across nursing units, you can predict exit trends before formal resignations occur. Acting early helps you stabilize care delivery, maintain staffing ratios, and stay aligned with broader organizational goals.
Global Healthcare Quiet-Quitting Statistics
Quiet quitting isn’t limited to one country or system. In fact, it’s happening across global healthcare settings, from major hospitals to local clinics. These international findings help you benchmark disengagement levels and spot patterns that may be emerging inside your own teams.
Here are the latest global statistics that offer a broader lens on quiet quitting in healthcare.
33. A MDPI report shows that 62% of hospital staff surveyed were identified as quiet quitters based on the Quiet Quitting Scale (QQS).
This measurement, based on validated scoring, points to a majority disengagement across hospital departments. This staff may be completing tasks but withholding extra effort, which erodes collaboration, innovation, and service quality. If you lead hospital staff strategy, this is your early warning signal to act.
34. AIMS Public Health noted 74.3% of nurses were classified as quiet quitters based on their QQS scores.
That level of disengagement means nearly three in four nurses are operating below full capacity. The risk extends beyond performance since it also creates instability in patient experience and mentorship pipelines. Nurse leaders and every Chief Nursing Officer should see this as a call to intervene with targeted support.
35. The MDPI report showed that only 13% of healthcare workers felt they received the rewards they deserved for their performance.
Perceived underappreciation drives quiet quitting and undermines organizational commitment. Without visible recognition (monetary or otherwise), staff usually conclude that extra effort brings no added value. If your rewards framework is outdated or unclear, you’re likely fueling disengagement unintentionally.
36. MDPI found out that hospital staff who felt management was unaware of their contributions were significantly more likely to engage in quiet quitting.
When leaders fail to acknowledge work, team members usually disengage in quiet but consistent ways. This breaks trust and accelerates withdrawal, especially in under-resourced roles. Using rounding tools or manager check-ins can help rebuild that lost visibility.
37. According to a Wiley Journal of Evaluation Clinical Practice report, a strong negative correlation (r = -0.62) was found between quiet quitting scores and workplace happiness.
This statistical link shows how disengagement and morale move in opposite directions. As quiet quitting rises, workplace happiness falls and vice versa. You can’t solve this with surface-level perks since it requires real action on fairness, voice, and team dynamics.
38. A March 2025 report from OPUS found that job burnout partially mediates the link between low organizational support and quiet quitting among nurses.
This means that burnout doesn’t cause quiet quitting alone. In fact, poor organizational support makes it worse. Nurses without access to debriefing spaces, mentoring, or recovery time are more likely to disengage. Rebuilding support systems is one of the fastest ways to stabilize frontline morale.
39. PMC PubMed Central reports that higher moral resilience was associated with lower levels of quiet quitting, burnout, and intent to leave.
Nurses and clinicians who feel aligned with their work values are more likely to stay engaged under pressure. You can build employee resilience through ethical leadership, team-based learning, and reflection practices. These small changes help anchor purpose even when demand spikes.
40. The same report from PMC shows that psychological (β = −0.307), physical (β = −0.136), and cultural (β = −0.247) work-life factors significantly reduced quiet quitting scores, while social factors had no significant effect.
This data reveals what actually drives sustained engagement, and that's autonomy, rest, and cultural fit, not just social interaction. Leaders who invest in flexible scheduling, meaningful work design, and value-aligned onboarding will see stronger retention and daily effort. Social activities alone won’t move the needle.
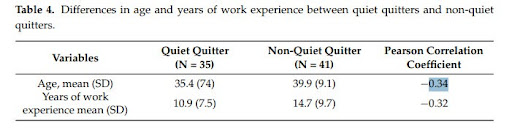
41. Another report noted that quiet quitting was more common among younger and less experienced nurses, with negative correlations found between both age (r = −0.34) and experience (r = −0.32) and QQS scores.
Early-career nurses may lack the tools, mentorship, or support to stay engaged under stress. Without intervention, this group may exit early or remain disconnected. Assigning experienced preceptors, building career pathways, and involving them in decision-making can improve engagement from the start.
Strategies to Address Quiet Quitting in the Healthcare Sector
Reducing quiet quitting starts with how your teams feel, act, and are supported day to day. There are solutions that can give you practical ways to shift behaviors, rebuild trust, and prevent disengagement from spreading.
Here are the targeted strategies you can apply across clinical and non-clinical teams:
- Coach managers to run structured one-on-ones that go beyond tasks. Use a simple three-question format, like "What’s going well?" "What’s blocking progress?" "What support would help right now?" These conversations typically surface disengagement before it becomes a pattern.
- Use quarterly pulse surveys to track team sentiment. Collect data and follow up within two weeks by summarizing results and outlining actions you’re taking. Silence after surveys makes quiet quitting worse.
- Revisit recognition programs to make them faster and more visible. Peer-to-peer tools like Kudos or Bonusly work well, especially when tied to values or behaviors, not just output.
- Give units flexibility to pilot shift redesigns. For example, let departments test 4-on-3-off models or split high-load shifts. Autonomy at the schedule level usually leads to better effort during working hours.
- Review internal mobility paths for nurses, physicians, and support staff. Disengagement rises when capable people feel stuck. So, show them options, and follow up with coaching or mentorship.
Pro tip: Quiet quitting usually signals misalignment in staffing models. For many hospitals, shifting to RPO support creates structure and relief that internal teams can’t always manage alone.
Rebuilding Engagement Starts with Better Support
Quiet quitting is a sign of deeper strain inside your teams, not a temporary trend. When effort drops quietly, performance and care quality follow. The most effective response combines targeted staffing, stronger leadership practices, and clear engagement strategies.
That’s where AAG Health can help. We connect you with skilled clinicians, handle recruitment through flexible RPO models, and guide workforce decisions with data-backed consulting. Whether you need nurse staffing, leadership recruitment, or system-wide engagement planning, we’ll work with your team to get ahead of the problem.
Contact AAG Health to start building a workforce that’s committed and fully engaged.
FAQ
Why is it called quiet quitting?
The term "quiet-quitting" refers to employees doing only what’s required in their job, without taking on extra hours, added responsibilities, or making any stretch efforts. It isn’t an actual resignation but a form of disengagement where staff continue working but mentally disconnect from the role or the organization’s goals.
Why is Gen Z quiet quitting?
Younger staff tend to value boundaries and expect workplaces to support mental health, flexibility, and purpose. When they feel their voice doesn’t matter or their well-being is ignored, many choose to scale back instead of speaking up. Without early mentorship, feedback, or clarity on advancement, Gen Z staff usually disengage faster.
Is quiet quitting a good thing?
From a workforce strategy perspective, no, because it signals something is broken. It means staff no longer feel motivated to go beyond what’s required. Left unchecked, it reduces team reliability, increases risk in care delivery, and affects retention in critical units.
What are the rules of quiet quitting?
There are no formal rules. Quiet quitting typically starts as personal boundary-setting but turns into a performance risk if left unaddressed. What matters is how consistently you identify and respond to it.
What is an example of quiet quitting?
There are plenty of examples of quiet quitting. One example is a nurse who stops mentoring, declines committee roles, and avoids extra charting, yet still shows up and completes shift duties, is likely engaging in quiet quitting.
Why did people start quiet quitting?
Quiet quitting likely gained momentum after the COVID-19 pandemic exposed long-standing gaps in recognition, support, and flexibility. Many staff realized overperformance wasn’t rewarded and began pulling back as a coping response.

