In 2025, hospitals are investing heavily in interventional radiology (IR), from new imaging suites to advanced devices and skilled physicians. Yet many programs stall when credentialing drags on for months. With ongoing radiologist shortages, every delay means lost productivity, longer patient wait times, and compliance risk.
This guide helps you avoid that. It explains what IR credentialing is, why it matters now, and how to streamline every step. You’ll find:
- What is IR credentialing anyway? We’ll define it clearly (and distinguish it from things like privileging and certification).
- Why it matters, and especially now. The IR field is expanding: the global IR market is estimated at US $31.2 billion in 2025 and is projected to grow at ~5.7 % annually through 2032.
- What makes it hard? Spoiler: internal silos, shifting regulations, verifying complex qualifications, and keeping pace with evolving technologies all conspire against smooth credentialing.
- Your 2025 IR credentialing checklist. A tactical, step‑by‑step playbook you can adapt to your organization.
- Pro advice. From tech to governance to cross-team alignment, we’ll show you how to turn credentialing from a bottleneck into a strength.
By the end of this guide, you’ll have a working framework, an Interventional Radiology (IR) Credentialing Checklist that you can plug into your hospital or clinic operations immediately. Ready? Let’s go.
P.S. If you are struggling to find credentialed radiologists fast enough, don’t worry. AAG Health fills the gap with board-certified tele-radiologists who are already licensed, credentialed, and can integrate seamlessly into your systems.
What Is Interventional Radiology (IR) Credentialing?
Interventional Radiology (IR) is one of the fastest-evolving specialties in modern medicine. These physicians use advanced imaging, like CT, fluoroscopy, ultrasound, and MRI, to guide minimally invasive procedures that treat everything from cancer to vascular disease. The work is highly technical, often high-stakes, and absolutely requires verified expertise.
That’s where IR credentialing comes in.
IR Credentialing is the formal process that healthcare organizations use to verify that an interventional radiologist has the training, licensure, experience, and qualifications to meet regulatory and institutional standards. It's a patient safety mandate, a compliance requirement, and a frontline defense against legal risk.
Credentialing is often confused with terms like privileging or board certification, but they’re not the same.
Here’s a quick overview:
- Board certification is earned from a national body such as the American Board of Radiology (ABR). It confirms that a physician has passed specialty examinations and demonstrated core competence.
- Privileging is about granting formal permission to perform specific IR procedures, like embolization or thrombectomy, based on what credentialing uncovers
- Re-credentialing is the ongoing review process (typically every 2–3 years) to make sure the physician stays qualified and up to date
Together, these processes make up the foundation of safe, quality-driven care in IR. And in 2025, the stakes are higher than ever. Demand for IR is on the rise globally, which means more procedures, more specialists, and more pressure on credentialing teams to keep up.
Yet credentialing remains slow and complex. It can take up to 120 days to credential a physician from start to finish.
And if things get held up, the financial impact can be drastic. For example, Merritt Hawkins found that credentialing delays cost healthcare organizations roughly $9,000 per provider per day in lost revenue due to extended wait times and disrupted revenue cycles.
Some estimates suggest providers lose over $120,000 in revenue during the waiting period.
For interventional radiology departments trying to scale services, such delays can derail growth, delay patient care, and throw off entire operational timelines. That’s why having a smart, proactive approach to IR credentialing is so incredibly important.
Why Interventional Radiology Credentialing Matters
You might think credentialing is just internal red tape, but in 2025, it's front and center for institutions trying to stay sharp, safe, and competitive. Here’s why this year demands you take IR credentialing seriously:
Surge in IR demand & market growth
Interventional Radiology services are quickly becoming integral to how hospitals manage everything from vascular disease to oncology.
The global IR market is growing fast, and some forecasts even predict that by 2035, the market could reach USD 49.4 billion, growing at around a CAGR of 5.2 % from 2025 to 2035.
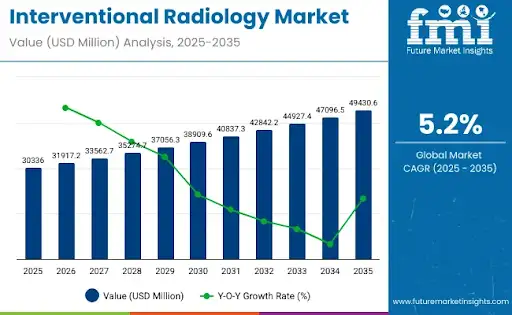
As procedure volumes rise and more specialists enter the field, hospitals must ensure their credentialing systems scale seamlessly to verify qualifications, privileges, and renewals on time.
Institutions that modernize their credentialing workflows will safeguard patient outcomes, accelerate onboarding, and maintain a competitive edge in the rapidly expanding IR sector.
Higher regulatory, payer & accreditation scrutiny
Healthcare regulators, payers, and accreditation bodies are tightening standards. They’re not just asking “Is the person a radiologist?” but “Has this radiologist been vetted for this procedure, in this facility, with these devices and safety protocols?” Modern credentialing has to meet multi-dimensional scrutiny:
- Insurance payers mostly reject claims when physicians are not fully credentialed and enrolled with each plan.
- Accreditation bodies (like Joint Commission equivalents in many countries) demand documented oversight and timely audit trails for credentialing.
- Government agencies and health systems increasingly demand transparency when it comes to provider qualifications, credentialing dates, and adverse-event histories.
So, having a sloppy credentialing process is a liability you’ll be penalized for.
Talent acquisition & retention in a competitive market
You’re competing for the same IR talent as every big hospital, academic center, and private practice out there. Lengthy or disorganized credentialing can quickly become a dealbreaker:
- IR physicians increasingly expect streamlined onboarding. Many request written guarantees that credentialing will be fast and transparent before accepting new positions
- Extended delays reduce engagement. When physicians wait weeks in limbo, they lose confidence and valuable billable hours that could be spent performing procedures elsewhere.
- Reputation matters. Institutions known for red tape or inconsistent onboarding lose top candidates to competitors with efficient, well-managed credentialing systems.
Remember, credentialing is part of your “employer brand” in the Interventional Radiology industry. Get it wrong, and the best talent will walk away.
Explore how remote and hybrid staffing models help hospitals retain talent and expand capacity in Remote Radiology: Solving Staffing, Speed, and Quality Challenges
Operational and financial risk
Every day, a credentialing delay keeps a new interventional radiologist from practicing. And hospitals lose both revenue and clinical efficiency. Procedures are postponed, schedules disrupted, and patients wait longer for care.
Credentialing delays often take up to 120 days, and some estimates suggest that credentialing delays can cost $6,000–8,000 per provider per month in lost opportunity costs.
These numbers might be U.S.-centric, but the principle holds globally. Inefficient credentialing drains financial resources, undermines operational momentum, and weakens institutional credibility.
Read Next: The Real Cost of Radiology: What Clinics Need to Know About Radiologist Salaries
Complexity & evolving practice
As we mentioned above, the pace of innovation in interventional radiology (IR) is accelerating, so credentialing must evolve in parallel. Robotics, AI‑assisted imaging, newer devices, hybrid suites, and outpatient IR centers demand faster, more adaptive verification systems:
- New procedures are becoming standard. Techniques that weren’t standard 5 years ago, such as neurovascular or structural heart IR interventions, are now routine in leading programs.
- Technology partnerships shape credentialing. Device-specific training, vendor partnerships, and manufacturer credentialing rules sometimes become part of your credentialing rubric
- Subspecialty crossover complicates privileges. Combined fields such as IR + cardiology or IR + oncology mostly raise questions about overlapping privileges and credential boundaries
Your credentialing process must be agile enough to adapt to changing IR scopes and tech innovations, without compromising safety or compliance.
Common Challenges in Interventional Radiology Credentialing
Credentialing an interventional radiologist might sound like a straightforward process where you collect some paperwork, verify a few licenses, sign off, and you’re done. But in the real world, it’s rarely that clean.
Some of the biggest hurdles healthcare institutions run into when it comes to IR credentialing are:
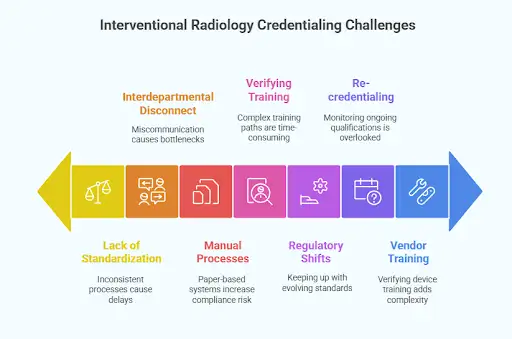
1. Lack of Standardization
Not all hospitals or clinics credential interventional radiologists the same way, and that inconsistency can lead to delays, confusion, and even compliance gaps. What one facility accepts as sufficient training might be a non-starter for another.
Without clear, standardized protocols, credentialing teams spend valuable time rebuilding workflows and reconciling requirements. This increases both the administrative burden and the potential for oversight.
2. Verifying Complex Training Paths
Interventional radiology isn’t a uniform specialty. Providers can come from diagnostic radiology, vascular surgery, or even international training programs.
If you’d like to explore the various subspecialties in more detail, see our guide on Different Types of Radiologists.
Verifying their subspecialty education, case logs, and specific procedural experience can be time-consuming, particularly when you’re dealing with overseas certifications or non-traditional career paths.
This variability increases administrative workload and extends verification timelines, often requiring direct communication with multiple licensing bodies or foreign institutions.
3. Keeping Up With Regulatory Shifts
Credentialing standards evolve continuously. Between updates from accrediting bodies, shifts in payer requirements, and changing scope-of-practice regulations, it’s easy for internal policies to fall behind.
More than half of practices (54%) have reported rising credentialing-related denials. This shows how frequent payer and accreditation changes can quickly translate into revenue losses and compliance challenges.
What was compliant last year may no longer suffice, and if you miss a beat, your institution could be held liable. Staying current requires dedicated oversight, clear documentation, and regular policy audits.
4. Interdepartmental Disconnect
Credentialing doesn’t live in one department. HR, medical staff services, legal, IT, and clinical leadership all play critical roles in the process. But when these teams aren’t aligned, on roles, timelines, or even what’s required, bottlenecks happen quickly.
Miscommunication and fragmented accountability are among the leading causes of credentialing delays that stretch from weeks into months. Therefore, establishing clear ownership and consistent cross-department workflows is essential for maintaining efficiency and compliance.
5. Manual Processes and Fragmented Systems
Let’s be honest, some organizations still rely on spreadsheets, emails, or even paper-based systems to manage credentialing. Without centralized digital platforms or integrated credentialing tools, tracking progress becomes a nightmare.
A 2024 survey, The State of Payer Enrollment & Credentialing by Medallion, found that 52% of credentialing workflows remain entirely manual, relying on paper documents, spreadsheets, and email exchanges.
The same report revealed that 33% of organizations spend more than 8 business days just gathering provider information before credentialing even begins.
These manual methods lead to duplicate data, version inconsistencies, and lost documentation, all of which extend onboarding timelines and increase compliance risk. Modernizing credentialing infrastructure with automated, auditable systems is now a prerequisite for speed, accuracy, and regulatory readiness.
6. Re-credentialing Gets Overlooked
Initial credentialing typically gets all the attention. But what about 18 months from now? Or after a clinical incident? Lots of institutions lack a structured process for monitoring ongoing qualifications, CME tracking, and re-evaluation.
Without structured re-credentialing, gaps can develop in licensure, training, or performance documentation. This, in turn, can increase exposure to compliance violations and patient-safety risks over time.
7. Vendor and Device Training Complications
Modern IR procedures now rely on specific devices, many of which require manufacturer-approved training or certification before use. But verifying that a provider has met these requirements, and building that into the credentialing process, adds another layer of complexity.
Missing or incomplete vendor training documentation can delay privileging and create liability during audits.
IR credentialing is harder than it looks, especially at scale. But the good news is that these challenges are solvable, especially when you’ve got a clear, modern checklist to work from.
Interventional Radiology (IR) Credentialing Checklist for 2025
If you’re overseeing credentialing for IR in your organization, this is your blueprint. Use it whether you're onboarding a new radiologist or refining your existing process.

How to Simplify and Speed Up Interventional Radiology Credentialing
Doing credentialing properly involves lots of moving parts and high stakes. But the right strategies and smart habits can make it much more manageable.
Below are key practices that improve speed, accuracy, and team coordination.
.webp)
1. Automate What You Can & Use Credentialing Technology
One of the biggest drags on credentialing teams is manual status checks, chasing documents, and following up with external bodies. A good credentialing platform or software tool can:
- Send reminders automatically for expiring credentials, CME, or re-credentialing deadlines
- Track progress via dashboards to see who’s stuck and where delays are
- Integrate with EHRs, HR systems, and payer portals
- Store digital records and audit trails
According to the 2025 Credentialing in Focus report, 67 % of credentialing teams say their processes are mostly or entirely manual, which drags efficiency and extends timelines.
Also, a recent survey found that 42 % of hospitals are already planning to replace outdated credentialing platforms in the next 18 months.
If your tech is sluggish or fragmented, that’s a weak link. Upgrading it can lead to significant returns in time, error reduction, and provider satisfaction.
2. Build Clear, Standardized Protocols & Templates
Credentialing should follow a predictable, repeatable structure, not a custom process every time. Standardization ensures consistency, speeds reviews, and strengthens compliance.
Create unified templates and criteria for:
- Required documents and forms: Credentialing, privileging, and vendor/device training forms.
- Acceptable levels of experience: Minimum case volume thresholds and procedural competencies.
- Evaluation template: Peer reference forms, site-visit checklists, and performance review guides.
- Workflow charts: Define each department’s review order and sign-off responsibility.
When all stakeholders (HR, medical staff office, and IR leadership) follow the same protocol, handoffs become smoother, verification cycles shorten, and credentialing errors decrease.
3. Cross‑Team Alignment & Communication Cadence
Smooth credentialing depends on ongoing coordination between all departments involved. Miscommunication or unclear handoffs often cause preventable delays, so consistent alignment is critical.
To avoid mistakes:
- Hold recurring coordination meetings during onboarding phases (weekly or bi-weekly) to track progress and flag bottlenecks early.
- Share a centralized “credentialing status board” that’s accessible to all stakeholders
- Assign clear ownership (Who is responsible for chasing reference? Who escalates if licenses aren’t confirmed?)
- Set service-level agreements (SLAs), establish specific turnaround times for each step, such as peer references due within seven calendar days.
4. Audit, Monitor, & Continuously Improve
Don’t let credentialing be something you set and forget. Monitor how you’re doing, spot weak spots, and iterate:
- Track KPIs like total credentialing cycle time (from application start to full approval). Best practices aim for 60–90 days for many specialties.
- Break down the cycle time by sub‑segments like document collection, primary source verification, committee review, and payer enrollment to see bottlenecks
- Conduct root cause reviews on delayed cases to determine corrective actions.
- Use feedback loops (from providers, other departments) to refine forms, templates, or handoffs
Remember that this is an ongoing process of trial and error. Your first process will rarely be your final polished version.
5. Prioritize Onboarding Plans with Credentialing in Mind
For new IR hires, treat credentialing as part of their onboarding plan. Embed it into the overall timeline:
- Start documentation early. Begin gathering required documents even before their official start date
- Map credentialing milestones. Align these with other orientation tasks to keep progress visible and measurable.
- Forecast the “dark period” when they can’t bill, and plan around it
- Consider provisional privileges (if safe and allowed) to let them do lower-risk work while full credentialing is underway
6. Leverage Vendor & Manufacturer Relationships Early
As we mentioned above, in Interventional Radiology, many devices have associated training or certification requirements (robotics, specialized imaging systems, etc.).
Here’s how you can smooth that path:
- Clarify device requirements upfront. Before finalizing hiring, ask: “Which devices will they use? Are vendor trainings required?”
- Coordinate vendor training in advance. Pre-arrange vendor credentialing or training slots so the candidate can complete them early
- Request verification directly from manufacturers. Obtain training validation letters or digital proof of completion.
- Store those confirmations in the credentialing file. Maintain these confirmations alongside licensure and CME evidence for full compliance.
7. Forecast & Build Resilience
Even with a perfect process, unexpected delays or missing documents are bound to crop up. To manage risk:
- Always build buffer time into your credentialing timeline to absorb unforeseen delays.
- Maintain a “credentialing reserve roster” of approved providers who can step in temporarily
- Use escalation protocols (like a senior leadership review of especially delayed or stuck cases)
- Keep backup copies or parallel processes (paper and digital) during system migrations
Close Credentialing Gaps Fast with AAG Health
Credentialing interventional radiologists is a frontline operational priority. When done right, it protects patients, speeds up onboarding, reduces legal risk, and sets your IR program up for long-term growth. But when it’s clunky or inconsistent, it slows everything down.
This year, the pressure is higher, which means more demand, more scrutiny, and more complexity. But with the right strategy and the right checklist, you can stay ahead of the curve.
Delays in IR credentialing or staffing can disrupt patient care. AAG Health helps hospitals and imaging centers fill these gaps quickly with board-certified, fully credentialed radiologists who can integrate seamlessly into your systems.
From short-term locum coverage to long-term staffing, AAG Health streamlines licensing, privileging, and onboarding, so your team can focus on helping patients.
Contact us today to ensure your IR department stays fully staffed, compliant, and patient-ready.
FAQs
1. What role does a residency program play in IR credentialing?
A completed residency program, especially one with a dedicated IR residency, is a key component of a physician’s credentials. It proves that they’ve had foundational training in radiology and clinical procedures, which are both essential for credentialing.
2. Do image-guided procedures require special credentialing?
Yes. Image-guided procedures like embolizations or biopsies demand specific training and verification, especially when using tools like Magnetic Resonance Imaging or fluoroscopy. These procedures must be explicitly listed in a provider’s privileges.
3. How does medical education factor into IR credentialing?
Your formal medical education is the starting point. Credentialing teams will verify your degree, training history, and whether your program meets regional accreditation standards. This includes credentials earned during or after clinical rotations.
4. How are residency transfers handled in IR credentialing?
Residency transfers aren’t uncommon, but they do complicate credentialing. Institutions will want to verify all training programs, rotations completed, and ensure that no lapses or disciplinary issues occurred during the transition.
5. Can AAG Health provide credentialed interventional radiologists for short-term coverage?
Yes. AAG Health maintains a network of board-certified, fully credentialed radiologists who can fill coverage gaps fast. Whether you need weekend, holiday, or multi-week locum tenens support, our team coordinates licensing and privileging so care continues without disruption.
6. How fast can AAG Health deploy credentialed radiologists to a new facility?
In most cases, placement occurs within days rather than months. Because our physicians are pre-vetted and pre-credentialed across multiple states and health systems, onboarding and payer enrollment move quickly. We help you avoid the 90-day delays of traditional hiring cycles.
7. What quality standards does AAG Health use when credentialing its radiologists?
Every physician in our network meets national board certification standards, verified clinical experience, malpractice screening, and background checks. We also require ongoing CME participation and periodic performance reviews to maintain credentialing integrity.

